- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
Removing a patient’s race from an equation used to assess lung function — a change called for by health equity advocates — would mean that the lung disease of nearly half a million Black
Americans would be reclassified as being more severe, and that Black veterans could receive more than $1 billion in additional disability payments, according to a study published Sunday in
the New England Journal of Medicine. The issue of how race is used in clinical algorithms has become a topic of widespread discussion, and controversy, in recent years, and the American
Thoracic Society is among many medical societies that have been grappling with the issue. Last year it said that a racial correction may contribute to health disparities in lung disease and
should no longer be used, but it called for more research on the downstream effect of such changes. The new paper, which is being presented during the society’s annual meeting in San Diego,
is an attempt to quantify those effects. The study’s senior author, Raj Manrai, an assistant professor of biomedical informatics at Harvard Medical School, said he hoped the results would
help prepare clinicians and health systems for the large number of patients whose lung disease status may change as a result of new race-free equations. Pulmonary function labs in hospitals,
the authors said, may need to build more capacity and be prepared for a possible increase in patient volume as more patients require follow-up lung testing. Nirav Bhakta, a pulmonologist at
the University of California, San Francisco who was first author on the thoracic society’s statement, called the new study “a huge effort” and said it painted the clearest picture yet of
the changes health systems might anticipate due to the use of the new equations. He told STAT that other data indicated extra tests and imaging were warranted to prevent mortality and that
pulmonary function labs could respond by adding capacity and also by reducing unnecessary pulmonary testing “not proven yet to change outcomes.” Remote, at-home spirometry using AI-driven
quality control and coaching could also help ease the burden on hospital labs, he said. Boston Medical Center, a safety net hospital that serves a diverse and international population of
patients, recently updated its spirometers to use the race-neutral equation. The change requires software updates and integration into electronic health records, but BMC was fortunate to be
in the midst of an update so incurred little additional cost, said Michael Ieong, an assistant professor at Boston University who directs the hospital’s pulmonary function testing lab. Ieong
said it would take time to see how many patients were actually affected and that the mix of patients seen by a hospital system would likely play a role. He noted Johns Hopkins physicians
reported they have been using the race-neutral equation for more than a year with little change to patient volume. The paper makes clear, he said, that “the use of simple cutoffs by
non-medical entities (such as those who assess disability claims or make hiring decisions) should be urgently reassessed.” The racial correction had been used to adjust readings from
spirometers, devices used to assess lung function and diagnose and manage respiratory diseases. This adjustment — by as much as 15% in Black patients — had been questioned for decades by
health equity advocates because it traces back to slavery-era science, which was used to justify slavery by suggesting that Black people had to be forced to work to keep their supposedly
weaker lungs healthy. The adjustments were also criticized because categorizing people as Black for medical reasons is problematic given that race is not a biological category and many Black
Americans have significant European ancestry. “We found profound clinical, financial, and occupational implications of how race is operationalized in pulmonary function testing,” the
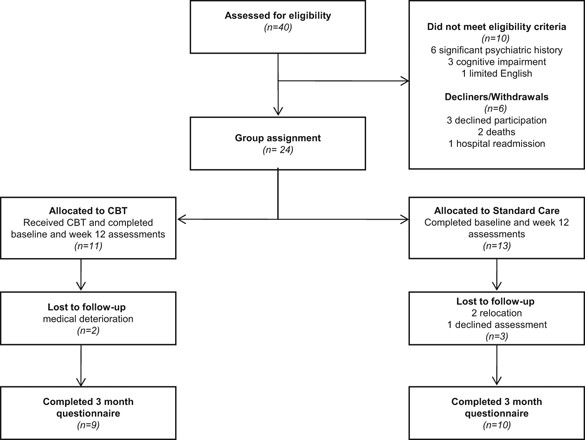
study’s lead author, fourth-year Harvard Medical School student James Diao, said in a statement. The authors used the data from nearly 370,000 patients in five datasets and calculated lung
function using both the old and new equations. They found that the race-specific and race-neutral equations performed similarly in predicting symptoms of lung disease, health care
utilization, and death, but that they resulted in major differences in how lung disease was classified in terms of severity. “Black patients who have been previously evaluated for lung
function impairment should strongly consider seeking re-evaluation using the new race-free equations, particularly if they were evaluated specifically for disability or workers’
compensation” because they could be eligible for substantially increased disability payments, said Rohan Khazanchi, a co-author who is an internal medicine and pediatrics resident physician
in Boston and a research affiliate at Harvard University’s FXB Center for Health & Human Rights. “The downstream inequities in disability and workers’ compensation reflects a unique
example of racism in medicine, as it may worsen the tremendous racial wealth gaps that already exist and persist in our country,” he added. All told, the authors said, 12.5 million Americans
may see reclassifications in levels of their lung impairment. The study found, for example, an additional 430,000 Black people would be diagnosed with moderate to severe COPD, while 1.1
million fewer white patients would be diagnosed. Veterans Administration disability payments could grow by 17% overall for Black veterans — with increases from nearly $2,000 to $10,000
annually for many vets — and could decrease by 1.15% for white veterans. The change could result in an overall redistribution of $1.94 billion each year among more than 400,000 eligible
veterans. The study “compels us to reconsider how eligibility determinations are made for disability or occupational fitness. For too long, such determinations have relied on simple
measures,” two pulmonologists, Meredith McCormack and David A. Kaminsky, wrote in an accompanying editorial. “We need new approaches that apply equally to everyone.” The results, the study
authors said, will lead to “tradeoffs.” Some patients with more severe disease might become eligible for new treatments, benefits, and breathing support, but lose eligibility for other
treatments, such as surgery to remove lung tumors. The equation could also affect the eligibility of people for certain jobs that require healthy lungs. More than 750,000 Black Americans
would no longer be eligible for firefighting jobs under the new equation, while 1.27 million white Americans would be newly eligible. “At the end of the day, our hope is that clinical
decision support tools serve all patients in an evidence-based way,” Khazanchi said. “Our study helps reinforce this point by demonstrating no significant differences in accuracy between
race-based and race-free lung function equations.”