- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT STUDY DESIGN Pilot study. OBJECTIVES To examine if functional electrical stimulation therapy (FEST) improves neuromuscular factors underlying upper limb function in individuals with
SCI. SETTING A tertiary spinal cord rehabilitation center specialized in spinal cord injury care in Canada. METHODS We examined 29 muscles from 4 individuals living with chronic, cervical,
and incomplete SCI. The analysis was focused on the changes in muscle activation, as well as on how the treatment could change the ability to control a given muscle or on how multiple
muscles would be coordinated during volitional efforts. RESULTS There was evidence of gains in muscle strength, activation, and median frequency after the FEST. Gains in muscle activation
indicated the activation of a greater number of motor units and gains in muscle median frequency the involvement of higher threshold, faster motor units. In some individuals, these changes
were smaller but accompanied by increased control over muscle contraction, evident in a greater ability to sustain a volitional contraction, reduce the co-contraction of antagonist muscles,
and provide cortical drive. CONCLUSIONS FEST increases muscle strength and activation. Enhanced control of muscle contraction, reduced co-contraction of antagonist muscles, and a greater
presence of cortical drive were some of the findings supporting the effects of FEST at the sensory-motor integration level. You have full access to this article via your institution.
Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS NON-INVASIVE SPINAL CORD ELECTRICAL STIMULATION FOR ARM AND HAND FUNCTION IN CHRONIC TETRAPLEGIA: A SAFETY AND EFFICACY TRIAL Article Open
access 20 May 2024 EFFECTS OF REPETITIVE TRANSCRANIAL MAGNETIC STIMULATION ON RECOVERY IN LOWER LIMB MUSCLE STRENGTH AND GAIT FUNCTION FOLLOWING SPINAL CORD INJURY: A RANDOMIZED CONTROLLED
TRIAL Article Open access 09 September 2021 CHARACTERIZING NEUROLOGICAL STATUS IN INDIVIDUALS WITH TETRAPLEGIA USING TRANSCUTANEOUS SPINAL STIMULATION Article Open access 06 December 2023
INTRODUCTION Any damage causing transient or permanent functional change to the spinal cord can cause a spinal cord injury (SCI). A cervical SCI impairs upper limb function and reduces
independence and quality of life. Therefore, upper limb function is the top priority of recovery for individuals with tetraplegia [1]. SCI interrupts the signal transmission between the
central and peripheral nervous systems at the level of the spinal cord, but the functional state of the spinal networks can be changed through neuromodulation [2]. Functional electrical
stimulation is a method of neuromodulation that focuses on producing functionally useful contractions through peripheral stimulation [3]. Since the 1960 s, functional electrical stimulation
has been used to improve the function of the upper extremities for individuals with neurological disorders including cervical SCI in the context of both neuroprostheses and electrotherapy
[4]. Functional electrical stimulation therapy (FEST) refers to the application of electrical stimulation as a therapeutic modality rather than a neuroprosthetic assistive device [5]. The
majority of clinical trials on FEST to retrain hand reaching and grasping after SCI uses FEST sessions of 45–60 min delivered 3–5 days a week, for 8–16 weeks, for a total of ~40 sessions
[6]. During these sessions, the patient attempts voluntary movements, such as forward-reaching, lateral pinch, and palmer grasping for performing activities of daily living such as object
manipulation and self-feeding. Pulsed electrical stimulation is applied through electrodes placed close to the motor points of the target muscle groups in order to produce functional
patterns of muscle contraction [6, 7]. A therapist activates the stimulation when the patient is not able to complete the movement on their own. The positive immediate effect of FEST has
been shown to improve hand function of individuals with cervical SCI [8]. When applied over a period of several weeks, FEST has demonstrated promising improvements in clinical assessments of
upper extremity function compared with conventional therapies for individuals with subacute or chronic cervical SCI, even in cases with motor complete SCI (American Spinal Injury
Association [ASIA] Impairment Scale [AIS] A or B) [7, 9,10,11,12]. The efficacy of FEST in improving voluntary reaching and grasping after stroke has also been demonstrated in series of
pilot studies and clinical trials, further confirming its potential for upper limb neurorehabilitation [13,14,15,16,17]. Despite these positive results, the mechanisms underlying FEST at the
neuromuscular level remain incompletely understood [18]. The assessment of independence and function after SCI is commonly performed using well-established assessments of function and
strength [8, 11], including the Spinal Cord Independence Measure version III [19], the Functional Independence Measure [20], the Graded Redefined Assessment of Strength, Sensibility, and
Prehension (GRASSP) [21], the Toronto Rehabilitation Institute—Hand Function Test [22], and the Capabilities of Upper Extremity Test [23]. It is known that weakness of upper limb muscles is
related to performance in functional tasks [24, 25], and the strength of a combination of defined, specific upper limb muscles is able to predict upper limb function [26]. In this line of
thought, understanding the chronic changes in muscle strength with FEST may provide insights into the mechanisms of action of FEST at the muscle level, which are likely accounting for the
functional gains seen after FEST. When it comes to evaluating muscle strength, Manual Muscle Testing (MMT) is the standard test used in both the International Standards for Neurological
Classification of Spinal Cord Injury (ISNCSCI) and GRASSP [27,28,29,30]. Nonetheless, neurophysiological assessments would afford a more detailed description of the effects of FEST on muscle
activation and motor control [31]. Surface electromyography (sEMG) is a widely used technique to measure muscle activation noninvasively, providing complimentary information to the
aforementioned clinical assessments of muscle strength. In individuals with SCI, even without visible contractions of impaired muscles during voluntary movement attempts, sEMG signals can in
some cases be detected [32, 33]. Under the International Classification of Functioning, Disability, and Health framework (ICF) [34], sEMG can provide valuable information measured at the
level of body functions and structure, which is complimentary to clinical assessments of upper extremity function that are predominantly associated with the activity domain of the ICF.
Thereby, sEMG may be useful for evaluating therapeutic outcomes of FEST for individuals with SCI, beyond the functional gains, and provide insights on the mechanisms of action of FEST at the
neuromuscular level - which are currently lacking in the literature [18]. In this pilot study, we seek to describe the outcomes of FEST using sEMG amplitude (sEMGamp) and frequency
(sEMGfreq) during voluntary movement attempts. We also quantify the efficacy of FEST on segmental strength recovery for individuals with an SCI using a standard clinical assessment of muscle
strength, the well-established MMT. While prior research studies have focused on the intrinsic muscle changes after FEST [18], here we also explore different elements of the neuromuscular
system, namely the control of muscle contraction and the coordination between multiple muscle groups. We expect that the well-established gain in upper limb function with FEST [6, 7, 10, 35]
will be supported by changes in strength, activation, control, and coordination, at the single- or multi-muscle level. METHODS PARTICIPANTS AND ASSESSMENTS Individuals with SCI who
participated in this study were receiving FEST for upper extremity rehabilitation either through a clinical program at our institution (SCI cases 1 and 4) or through an ongoing clinical
trial (SCI cases 2 and 3) [36] (Institutional REB approval number: 17-6029, Research Ethics Board of the University Health Network, Toronto, Canada). Written consent was obtained from all
individuals with SCI to undergo EMG assessments and MMT tracking (REB approval number: 19-5395.6), and from non-disabled individuals (ND) for sEMG assessments (REB approval number: 19-6175).
Nine participants were enrolled in this study: 5 ND participants (reference group) and four individuals with SCI. There were two assessments for individuals with SCI, the first assessment
was conducted before the FEST initiation, and the second assessment was after the last FEST session. All the assessments were conducted on days of the week when there were no FEST sessions
scheduled or immediately before FEST administration. Only one assessment was performed for the ND group to obtain reference values. All the assessments were performed by the same
investigator. FEST DELIVERY FEST was delivered using the MyndMove® stimulation device (MyndTec, ON, Canada). The device offers a variety of stimulation protocols for the upper extremity,
including protocols specifically designed for individuals with SCI [6, 7]. The pre-programmed stimulation sequences facilitate functional movements of the arm and/or hand(s), employing a
wide variety of reaching and grasping movements. The therapy was tailored to each participant based on the therapists’ assessment of the individual’s needs and therapy goals. Supplementary
Table 1 provides a detailed breakdown of the FEST protocols used with each participant. OUTCOME ASSESSMENT: MMT We used the MMT, which is the muscle strength test used in both the ISNCSCI
and GRASSP [21, 27, 28, 37] If a muscle did not have a defined MMT protocol in the ISNCSCI nor the GRASSP, the physiotherapist would develop custom protocols to assess muscle strength in
these muscles. The MMT was scored using a standard 0–5 grading system [38] by a trained physical or occupational therapist before each FEST session. All the ND participants were considered
as grade 5, and the MMT consisted of providing full resistance in a functional muscle position. OUTCOME ASSESSMENT: SEMG To acquire sEMG signal from upper limb muscles, we used the
eight-channel Bagnoli® system (Delsys, MA, USA) with a 4 kHz sampling frequency and ×1000 amplification (hardware filter at 20–450 Hz). The electrodes were positioned over the muscle belly
using double-sided adhesive tape after trimming the hair and cleansing with alcohol. The positioning and orientation of the electrodes were based on the SENIAM guidelines [39] (i.e., _biceps
brachii, triceps brachii, anterior deltoid, abductor pollicis brevis, opponens pollicis, flexor pollicis brevis_) or elsewhere in the literature if not included in the SENIAM guidelines
(i.e., extensor carpi radialis, flexor carpi radialis, extensor digitorum communis, flexor digitorum superficialis, flexor pollicis longus, extensor carpi ulnaris, 1st dorsal intersossei)
[40]. sEMG signals were acquired from upper extremity muscles during isometric voluntary attempts using the standard MMT assessment protocol for each muscle, both in SCI and ND participants.
Three maximum voluntary contraction trials were obtained, followed by three trials at 50% MVC. The detailed protocol for sEMG acquisition is provided in the Supplementary Material. ANALYSIS
OF DATA ON MMT To understand the change in muscle strength after treatment, MMT change (ΔMMT) was calculated by subtracting baseline strength (the average of the first two MMT scores) from
endpoint strength (the average of the last two MMT scores). Considering that most clinical studies show long-term effects of electrical stimulation (13 days to 6 weeks) on muscle strength
[41], this averaging procedure was conducted to account for variability in the initial and final assessments. ANALYSIS OF DATA ON SEMG All of the sEMG metrics described below were extracted
from each trial and averaged over the 3 100% MVC trials and over the 3 50% MVC trials. Off-line sEMG signal processing involved the visual inspection of each contraction to ensure the
absence of artifacts in the signal. sEMG was filtered using a 2nd order Butterworth filter, band-pass between 10 and 450 Hz, and a band-stop filter between 59–61 Hz (to remove the power line
interference). The protocol for quality checking and extraction of analysis windows is provided in the Supplementary material. The amplitude of the sEMG (sEMGamp) was quantified using the
root mean square of the filtered sEMG signal for the entire analysis window during maximal voluntary contractions. To quantify the variability of the sEMG during the 50% maximal
contractions, the root mean square of 0.1-second bins were calculated throughout the contraction, and the coefficient of variation of the root mean square bins was calculated [COV =
(SD/Mean) × 100%]. Co-contraction was calculated for pairs of muscles using Eq. 1 [42]. $$Muscle\,co-activation = \frac{{2\,\times\,sEMG_{Antagonist}}}{{sEMG_{Agonist} +
sEMG_{Antagonist}}}\times\,100{{{\mathrm{\% }}}}$$ (1) The frequency-domain representation of the sEMG signal was assessed by the median frequency of the sEMG spectrum between 0 and 250 Hz
(sEMGfreq), also for the entire analysis window during maximal voluntary contractions. The median frequency was calculated using a procedure previously described [43]. Briefly, for the
calculation of the median frequency, the spectral profile of each window was divided into 100 bins (2.5 Hz resolution), and the numerical integral was calculated. The integrated sEMG was
then split into two halves of equal areas, this value (split point) constituting the median frequency in Hz. To understand the change in muscle activation after treatment, the sEMGfreq at
the baseline was subtracted from the sEMGfreq at endpoint (ΔsEMGfreq). To visualize the frequency component of the sEMG throughout the volitional contraction, we computed the short-time
Fourier transform-based spectrogram of sEMG signal (parameters are provided in the Supplementary material). To detect functional coupling in the frequency-domain, intermuscular coherence was
calculated. sEMG recordings of submaximal contractions were rectified, low-pass filtered, and down-sampled to 100 Hz sampling rate. The recordings were divided into 1-second nonoverlapping
windows. Denoting the Fourier transform of the _i_th window of the sEMG from two different muscles as _X__i_(_f_) and _Y__i_(_f_), respectively, the coherence is given by (Eq. 2) [44]:
$$Coh\left( f \right) = \frac{{\left| {\mathop {\sum }\nolimits_{i - 1}^L X_i^ \ast (f)Y_i(f)} \right|^2}}{{\mathop {\sum }\nolimits_{i - 1}^L X_i(f)X_i^ \ast (f)\mathop {\sum }\nolimits_{i
- 1}^L Y_i(f)Y_i^ \ast (f)}}$$ (2) where _L_ is the number of data windows available and * denotes the complex conjugate. The analysis of variability (COV), co-contraction, and intermuscular
coherence was conducted using the 50% maximal contraction trials. Where coherence was evaluated in the beta band (13–30 Hz), data from 20–30 Hz only was used due to hardware filtering below
this range. FEST INTENSITY AND DURATION Each FEST protocol described in Supplementary Table 1 involved a different set of muscles. The muscles stimulated during each protocol were obtained
from the manufacturer’s manual. Detailed information about the current delivered to each muscle and the time of treatment in each protocol was extracted from the reports generated after each
FEST session. For each muscle in each session, the current delivered was multiplied by the number of cycles the protocol was administered. This yielded the FEST dose delivered to each
muscle per session in mA, which was summed across all FEST sessions for each muscle [FESTdose(mA)]. Similarly, the time (in minutes) of FEST to each muscle was calculated [FESTdose(min)].
STATISTICAL ANALYSIS LabVIEW and GraphPad Prism were used to conduct the statistical analysis. Descriptive statistics were expressed using mean ± SD followed by a qualitative analysis of
graphs and results in comparison to the reference group (ND group). For the correlational analysis, the unit of measure was the individual muscle (_N_ = 29). Data normality was assessed
using the Shapiro–Wilk test, which indicated 7/12 variables used in the correlational analysis failed the normality test. Spearman correlation was used to test the relation between the
clinical assessments, electrophysiological assessments, and the FEST dose. Significance was set at _α_ = 0.05. RESULTS Baseline data and treatment modalities applied for rehabilitation after
SCI are summarized in Table 1. CASE 1 The first case is a 43-year-old male with a C5 motor complete (AIS B), chronic (8 months from injury onset), traumatic SCI. Prior to treatment, several
upper limb muscles were assessed using MMT and considered weak (_triceps brachii_ = 2; _extensor carpi radialis_ = 1.5; _extensor digitorum communis_ = 2.5; _flexor digitorum superficialis_
= 2.5; _flexor pollicis longus_ = 1; _flexor pollicis brevis_ = 0; _extensor carpi ulnaris_ = 1). These muscles were the focus of the FEST. The participant was enrolled in usual
physiotherapy sessions (14 sessions) and FEST sessions (20 sessions). The treatment was focused on the muscles presenting with weakness, and also muscles involved in integrated functional
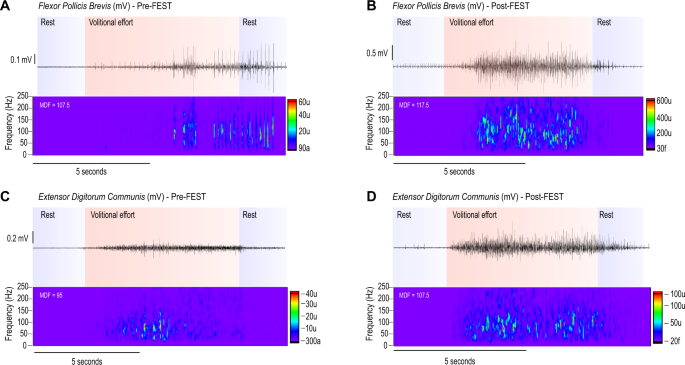
movements. After the FEST, an increase in muscle activation (sEMGamp and sEMGfreq) and strength (ΔMMT) was evident (Fig. S1). Pre-FEST, the participant had limited voluntary activation and
difficulty in deactivating motor units (MUs) upon command to relax (Fig. 1A, C). Post-FEST, voluntary activation, and deactivation was improved, with an MDF shift towards higher frequencies,
suggesting the involvement of faster MUs (Fig. 1B, D). CASE 2 The second case is a 63-year-old male with a C4 motor complete (AIS B), chronic (3 years and 6 months from injury onset),
traumatic SCI. Persistent and chronic muscle weakness were evident at the baseline MMT assessment, especially for hand muscles (_anterior deltoid_ = 2.5; _triceps brachii_ = 1; _extensor
carpi radialis_ = 2.25; _flexor carpi radialis_ = 1; _extensor digitorum communis_ = 0.5; _opponens pollicis_ = 1; _flexor digitorum superficialis_ = 0.5; _first dorsal interosseous_ = 0).
These muscles were the focus of the FEST. The participant was prescribed daily home exercise (30 min) and 40 FEST sessions at the clinic. The FEST sessions consisted of active-assisted
functional movements of the shoulder, elbow, and wrist coupled with the stimulation. Movements like reaching forward, grasping an object, reaching to the mouth were performed by the
participant with the help of the therapist. Prior to FEST, many muscles displayed absent sEMG with amplitude similar to noise levels—especially the hand muscles [noise levels (mV): _opponens
pollicis_ = 0.0079; _flexor digitorum superficialis_ = 0.0042; _first dorsal interosseous_ = 0.0028] (Fig. S2). FEST was able to increase muscle activation of _triceps brachii_—an increase
not detectable by the MMT assessment (Fig. 2A), and _extensor digitorum communis_. The effect of FEST in multi-muscle activation is also notable. For example, before the FEST, the
participant was not able to hold the muscle activation of some muscles, shifting between muscles of close innervation (e.g., C7, C8). In Fig. 2B this shift is depicted, where the activation
of the _extensor digitorum communis_ was not sustained and shifted to the _triceps brachii_. In this effort to activate the intended muscle, the intermuscular coherence between this pair of
muscles was high in the 13–30 Hz frequency, indicating great cortical drive in executing the motor task (Fig. 2C). From before to after FEST, the co-contraction between these muscles was
reduced and the coherence shifted to control levels, indicating greater ability to selectively activate and control the contraction of the _extensor digitorum communis_ muscle (Fig. 2D).
CASE 3 The third case is a 64-year-old male with C6 incomplete (AIS D), chronic (2 years and 8 months from the injury onset), traumatic SCI. Despite the close-to-normal strength and function
of proximal upper extremity muscles, this participant displayed persistent hand muscle weakness on both sides based on MMT assessments [_flexor digitorum superficialis_ = 0 (right), 0
(left); _abductor pollicis brevis_ = 0 (right), 1 (left); _opponens pollicis_ = 1 (right), 0 (left)]. The participant was enrolled in 60 minutes of recreational therapy (3x per week) and
completed 40 FEST sessions at the clinic. Generally, the session started with unilateral simple functional tasks like pinching and grasping different objects with assistance when needed and
progressed to bilateral more complex tasks like 3D puzzles and opening containers. Prior to FEST, the sEMGamp of the intrinsic hand muscles was close to noise levels (_abductor pollicis
brevis_ and _opponens pollicis_ ≈ 0.0028) with an absent change post-FEST (noise levels ≈ 0.0051). On the other hand, extrinsic hand muscles such as the _flexor digitorum superficialis_
displayed residual muscle activity pre-FEST, and this activity increased post-FEST with respective gains in strength (ΔMMT) (Fig. S3). The muscle activation for the _flexor digitorum
superficialis_ muscle was less steady pre-FEST with respective co-activation of the antagonist, _extensor digitorum communis_ (Fig. 3A). After FEST, the muscle activation of the _flexor
digitorum superficialis_ muscles was steadier and the reduced co-contraction with the agonist involves high-frequency coherence—which is indicative of greater volitional drive (Fig. 3B).
These results are summarized in Fig. 3C–F, where the bilateral reduction in the COV of the sEMG amplitude for the _flexor digitorum superficialis_ muscles is evident (Fig. 3C), indicating
greater control. Also, the co-contraction with the antagonist, _extensor digitorum communis_, was reduced alongside the greater contribution of intermuscular coherence in the β-frequency
range (indicative of greater cortical drive) (Fig. 3D–F). CASE 4 The fourth case is a 56-year-old male with a C3 incomplete (AIS D), chronic (1 year from the injury onset), traumatic SCI.
This participant displayed preserved against gravity strength in proximal upper limb muscles but weakness in extrinsic and intrinsic hand muscles [MMT score: _anterior deltoid_ = 3.5 (L), 2
(R); _triceps brachii_ = 3.5 (L), 2.5 (R); _biceps brachii_ = 4 (R); _extensor digitorum communis_ = 2.5 (R); _flexor digitorum superficialis_ = 2 (R); _first dorsal interosseous_ = 2 (R)].
The participant was enrolled in a shorter but intensive FEST program with 5 sessions of physiotherapy and 11 sessions of FEST at the clinic. Despite the lack of more pronounced effects on
sEMG amplitude, which was only evident for the _extensor digitorum communis_ and the 1st _dorsal interossei_ muscles, there was an overall gain in strength (Fig. S4). After FEST, the
participant was able to exert against gravity strength in all arm and hand muscles [MMT score: _anterior deltoid_ = 4 (L), 3.5 (R); _triceps brachii_ = 5 (L), 4.5 (R); _biceps brachii_ = 5
(R); _extensor digitorum communis_ = 4 (R); _flexor digitorum superficialis_ = 4 (R); 1st dorsal interosseous = 4 (R)]. This discrepancy between gains in strength and MU activation may
indicate: (i) less co-contraction or (ii) compensatory use of other muscles not assessed using sEMG but involved as agonists in the movements measured by the physiotherapists. Indeed, for
some pairs of antagonist muscles, the reduced co-activation is evident (Fig. 4A). We also observed the gain in fine control of the hand muscles during sustained 50% maximal voluntary
contractions after FEST (Fig. 4B–F). RELATIONSHIP BETWEEN MUSCLE STRENGTH, MUSCLE ACTIVITY, AND FEST INTENSITY AND DURATION To explore the relationship between the clinical assessments,
electrophysiological assessments, and the FEST dose, we used a correlational analysis (Fig. 5A). Hand muscles were overall weaker at baseline, with respective reduced activation (Fig. 5B–D).
There was a correlation between muscle strength (MMT score) and muscle activation (sEMGamp) both at the baseline and endpoint measurements (Fig. 5E, F). The amount of strength gain
post-FEST was related to the level of muscle activation at baseline, indicating that residual MU activity at baseline is important for this type of treatment (Fig. 5G). The dose of the FEST
delivered to each muscle was related to the strength of the muscles at baseline, likely reflecting the therapist’s choice of delivering most of the treatment to weaker muscles (Fig. 5H, I).
DISCUSSION In this pilot study, we show evidence that FEST promotes gains in muscle strength, which are accompanied by several electrophysiological changes. Some individuals display a
pronounced response to the treatment, with increases in both muscle strength and activation. This includes a greater amplitude of the muscle activation and frequency-domain changes that
reflect altered MU recruitment patterns. Small gains in muscle activation are accompanied by greater control during sustained activation or greater coordination between muscle groups. This
is evident in reductions in the variability in activation during controlled contractions, in reductions in muscle co-activation between pairs of antagonist muscles, and changes in
intermuscular coherence between muscles. The dose of therapy is related to how weak the muscle was at baseline—the latter likely reflecting the therapist’s choice of treating weaker muscles.
A recent scoping review documented the effects of FEST on the muscles, encompassing the changes in muscle composition, peripheral nerves, and central nervous system [18]. Evidence from
animal models of SCI indicated that FEST can improve neurovascular activation [45] and reduce the inflammatory response in the spinal cord (microglia activation) [46], suppress muscle
fatigue [47], and prevent muscle hypotrophy [48, 49]. Clinical studies indicate the maintenance or increase of muscle size, changes in muscle structure, increase in muscle fatigue
resistance, increase in muscle blood flow, increase in H-reflex excitability, and increase in the excitability of corticospinal pathways (for references see [18]). Because of the positive
relationship between muscle cross-sectional area and strength [50, 51], we indirectly corroborate the changes in muscle size by reporting strength gains after FEST in individuals with SCI,
similar to other treatments [52]. We further report changes in MU activation, evident in the greater amplitude and frequency components of the sEMG, indicating that a greater number of MUs
are activated post-FEST. In addition, the observed shifts in sEMGfreq toward higher frequencies likely indicate that higher threshold, faster MUs are active or that the muscles are overall
less fatigued after FEST. Nonetheless, these effects were not common to all muscles among the cases included in this study. Weaker muscles did not display a pronounced gain in strength or
activation, but yet there was evidence of enhanced control and coordination—likely explaining the striking ability of the FEST in improving upper limb function [6, 7, 10, 35]. sEMG analysis
adds subclinical details to the clinical picture of lesion severity and progression during hand rehabilitation, including the amount of muscle activation and the ability to activate prime
movers without involuntary activity in the other muscles [53]. This enabled us to study the effects of FEST in great detail and to unveil subtle neuromuscular changes with therapy. In the
nerve fibers innervating the human arm, it is known that the axonal components are mostly composed of sensory axons, which outnumber motor axons by a ratio of at least 9:1 [54]. Therefore,
when the electrical stimuli are delivered to the mixed peripheral nerve both efferent and afferent fibers are recruited, but ~90% of the triggered activity will ascend to the central nervous
system by the afferent pathways. This contrasts with the Rushton hypothesis of therapy-related synaptic modifications at the anterior horn cell level—by antidromic stimulation of motor
fibers [55], which are known now to represent a much lower percentage of the fibers contained in the mixed peripheral nerve [54]. Ascending afferent volleys are also generated by (secondary)
reafference arising from the invoked muscle contraction (reviewed in [56]). In this line of thought, the sensory-mediated consequences of the stimulation significantly alter the state of
sensory networks and induce sustained neuroplastic modifications within central motor networks [56]. Indeed, changes in corticospinal excitability are evident after electrical stimulation
both in ND [57, 58], and individuals with SCI [18, 59]. Here we provide insights on the ability of FEST in increasing sensory-motor integration, which was evident in the greater control of
muscle contraction and between muscles coordination post-FEST. Before the treatment, some individuals activated multiple and often functionally unrelated muscles upon command to contract a
single and specific muscle. This effort also demanded more cortical drive, evident in the predominance of coherence in the β-band [51], compared to ND individuals—reflecting the difficulty
in selecting the activation of the correct muscle. In other individuals, the co-contraction of antagonists muscles was reduced post-FEST while accomplishing this coordinated multi-muscle
action, with a respective increase in the cortical drive [51, 60,61,62,63] evident in increases in β-band intermuscular coherence. Finally, it was also evident that some individuals improved
the control of MU activation, reflected in a lower variability of the amplitude during sustained and controlled submaximal, visually guided contractions. The bulk of these findings provide
the first evidence on what neuromuscular factors may be responsible for the improvement in motor function seen after FEST [6, 7, 10, 35]. Further studies are necessary to confirm these
findings in a large sample of individuals, under similar or enhanced sEMG instrumentation and analysis such as high-density EMG or the decomposition of the sEMG [32, 64]. Finally, we
demonstrated the correlation between sEMGamp and the well-established MMT assessment, which agrees with previous findings [65]. Another important insight indicates that the sEMGamp at
baseline was related to the change in MMT with the FEST treatment. This indicates that the level of residual muscle activity is important for the efficacy of FEST on muscle strength, similar
to previous reports [66]. Therefore, the results of this study indicate that sEMG has the potential to complement the clinical assessment on the efficacy of FEST with valuable information,
including the opportunity to predict the efficacy of FEST - as discussed below in the “Clinical perspectives” section. CLINICAL PERSPECTIVES In addition to supporting the use of FEST in
rehabilitation programs following an SCI, the results of this pilot study suggest that longer FEST duration could increase meaningful and functional gains. The stimulation was delivered to
very weak muscles without active movement against gravity (i.e., MMT score <3) and promoted increased activation and strength in most of them. Future studies should investigate the
effects of longer FEST regimens. This study also demonstrated the potential use of sEMG to assess the efficacy of FEST for very weak muscles for which MMT might not be sensitive enough. The
sEMG could also be helpful to assess which muscle might benefit from FEST and if they are responding to the treatment in order to offer customized and efficient FEST programs to each
individual. Finally, sEMG can be a valuable biomarker, and has been used to identify discomplete patients [67]. However, the question remains whether treating a muscle with a grade 0 or 1
with good sEMG signal can show motor function recovery. LIMITATIONS This pilot study shows potential, clinically relevant benefits of FEST in individuals with chronic SCI, which can be
electrophysiologically evaluated using sEMG. However, there are limitations to this case series that must be taken into consideration in future studies. For example, our data analysis did
not control for the presence of spasticity and the important differences between spastic in contrast to flaccid paralysis because of the small sample size. Future full-scale studies should
account for the presence of spasticity given its importance for recovery after SCI. CONCLUSION In this pilot study, we explored the ability of FEST to increase muscle strength and activation
and provided insights on how the therapy might change sensory-motor integration. Enhanced control of the muscle contraction during visually guided half-maximal contractions, reduced
co-contraction of antagonist muscles, and a greater presence of cortical drive were some of the findings supporting the effects of FEST at the sensory-motor integration level. FEST has the
striking ability to generate ascending afferent volleys, with the sensory-mediated consequences of the stimulation being able to alter the state of sensory networks and induce sustained
neuroplastic modifications within central motor networks. Here we support the use of FEST to increase muscle strength and activation in individuals with an SCI and provide preliminary
evidence on how FEST can change sensory-motor integration to enhance upper limb function. DATA AVAILABILITY Data generated during the study is available upon reasonable request to the
corresponding author. REFERENCES * Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371–83. Article PubMed Google Scholar *
Taccola G, Sayenko D, Gad P, Gerasimenko Y, Edgerton VR. And yet it moves: recovery of volitional control after spinal cord injury. Prog Neurobiol. 2018;160:64–81. Article CAS PubMed
PubMed Central Google Scholar * Ho CH, Triolo RJ, Elias AL, Kilgore KL, DiMarco AF, Bogie K, et al. Functional electrical stimulation and spinal cord injury. Phys Med Rehabil Clin N Am.
2014;25:631–54. Article PubMed PubMed Central Google Scholar * Singer B. Functional electrical stimulation of the extremities in the neurological patient: a review. Aust J Physiother.
1987;33:33–42. Article CAS PubMed Google Scholar * Marquez-Chin C, Popovic MR. Functional electrical stimulation therapy for restoration of motor function after spinal cord injury and
stroke: a review. Biomed Eng Online. 2020;19:1–25. Article Google Scholar * Kapadia N, Moineau B, Popovic MR. Functional electrical stimulation therapy for retraining reaching and grasping
after spinal cord injury and stroke. Front Neurosci. 2004;14:718. Article Google Scholar * Popovic MR, Kapadia N, Zivanovic V, Furlan JC, Craven BC, Mcgillivray C. Functional electrical
stimulation therapy of voluntary grasping versus only conventional rehabilitation for patients with subacute incomplete tetraplegia: a randomized clinical trial. Neurorehabil Neural Repair.
2011;25:433–42. Article PubMed Google Scholar * Martin R, Johnston K, Sadowsky C. Neuromuscular electrical stimulation-assisted grasp training and restoration of function in the
tetraplegic hand: a case series. Am J Occup Ther. 2012;66:471–7. Article PubMed Google Scholar * Alon G, McBride K. Persons with C5 or C6 tetraplegia achieve selected functional gains
using a neuroprosthesis. Arch Phys Med Rehabil. 2003;84:119–24. Article PubMed Google Scholar * Kapadia N, Zivanovic V, Popovic MR. Restoring voluntary grasping function in individuals
with incomplete chronic spinal cord injury: pilot study. Top Spinal Cord Inj Rehabil. 2013;19:279–87. Article PubMed PubMed Central Google Scholar * Ditunno JF, Stover SL, Freed MM, Ahn
JH. Motor recovery of the upper extremities in traumatic quadriplegia: a multicenter study. Arch Phys Med Rehabil. 1992;73:431–6. PubMed Google Scholar * Popovic MR, Thrasher TA, Adams ME,
Takes V, Zivanovic V, Tonack MI. Functional electrical therapy: retraining grasping in spinal cord injury. Spinal Cord. 2006;44:143–51. Article CAS PubMed Google Scholar * Thrasher TA,
Zivanovic V, Mcilroy W, Popovic MR. Rehabilitation of reaching and grasping function in severe hemiplegic patients using functional electrical stimulation therapy. Neurorehabil Neural
Repair. 2008;22:706–14. Article PubMed Google Scholar * Marquez-Chin C, Bagher S, Zivanovic V, Popovic MR. Functional electrical stimulation therapy for severe hemiplegia: Randomized
control trial revisited. Can J Occup Ther. 2017;84:87–97. Article PubMed Google Scholar * Popovic MB, Popovic DB, Sinkjaer T, Stefanovic A, Schwirtlich L. Clinical evaluation of
functional electrical therapy in acute hemiplegic subjects. J Rehabil Res Dev. 2003;40:443–53. Article PubMed Google Scholar * Santos M, Zahner LH, McKiernan BJ, Mahnken JD, Quaney B.
Neuromuscular electrical stimulation improves severe hand dysfunction for individuals with chronic stroke: a pilot study. J Neurol Phys Ther. 2006;30:175–83. Article PubMed Google Scholar
* Popovic MB, Popovic DB, Schwirtlich L, Sinkjaer T. Functional electrical therapy (FET): clinical trial in chronic hemiplegic subjects. Neuromodulation. 2004;7:133–40. Article PubMed
Google Scholar * Furlan JC, Pakosh M, Craven BC. Popovic MR insights on the potential mechanisms of action of functional electrical stimulation therapy in combination with task-specific
training: a scoping review. Neuromodulation. 2022;25:1280–1288. Article PubMed Google Scholar * Itzkovich M, Shefler H, Front L, Gur-Pollack R, Elkayam K, Bluvshtein V, et al. SCIM III
(spinal cord independence measure version III): reliability of assessment by interview and comparison with assessment by observation. Spinal Cord. 2018;56:46–51. Article CAS PubMed Google
Scholar * Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil.
1993;74:531–6. Article CAS PubMed Google Scholar * Kalsi-Ryan S, Curt A, Fehlings MG, Verrier MC. Assessment of the hand in tetraplegia using the Graded Redefined Assessment of Strength,
Sensibility and Prehension (GRASSP): Impairment versus function. Top Spinal Cord Inj Rehabil. 2009;14:34–46. Article Google Scholar * Kapadia N, Zivanovic V, Verrier M, Popovic M. Toronto
rehabilitation institute-hand function test: assessment of gross motor function in individuals with spinal cord injury. Top Spinal CordInj Rehabil. 2012;18:167–86. Article Google Scholar
* Marino RJ, Patrick M, Albright W, Leiby BE, Mulcahey M, Schmidt-Read M, et al. Development of an objective test of upper-limb function in tetraplegia: the capabilities of upper extremity
test. Am J Phys Med Rehabil. 2012;91:478–86. Article PubMed Google Scholar * Zariffa J, Curt A, Verrier MC, Fehlings MG, Kalsi-Ryan S. Predicting task performance from upper extremity
impairment measures after cervical spinal cord injury. Spinal Cord. 2016;54:1145–51. Article CAS PubMed Google Scholar * Kramer JLK, Lammertse DP, Schubert M, Curt A, Steeves JD.
Relationship between motor recovery and independence after sensorimotor-complete cervical spinal cord injury. Neurorehabil Neural Repair. 2012;26:1064–71. Article PubMed Google Scholar *
Velstra IM, Bolliger M, Krebs J, Rietman JS, Curt A. Predictive value of upper limb muscles and grasp patterns on functional outcome in cervical spinal cord injury. Neurorehabil Neural
Repair. 2016;30:295–306. Article PubMed Google Scholar * Ciesla N, Dinglas V, Fan E, Kho M, Kuramoto J, Needham D. Manual muscle testing: a method of measuring extremity muscle strength
applied to critically ill patients. J Vis Exp 2011. https://doi.org/10.3791/2632. * Schmitt WH, Cuthbert SC. Common errors and clinical guidelines for manual muscle testing: ‘the arm test’
and other inaccurate procedures. Chiropr Osteopat. 2008;16:16. Article PubMed PubMed Central Google Scholar * Furlan JC, Fehlings MG, Tator CH, Davis AM. Motor and sensory assessment of
patients in clinical trials for pharmacological therapy of acute spinal cord injury: psychometric properties of the ASIA standards. J Neurotrauma. 2008;25:1273–301. Article PubMed Google
Scholar * Furlan JC, Noonan V, Singh A, Fehlings MG. Assessment of impairment in patients with acute traumatic spinal cord injury: a systematic review of the literature. J Neurotrauma.
2011;28:1445–77. Article PubMed PubMed Central Google Scholar * Hubli M, Kramer JLK, Jutzeler CR, Rosner J, Furlan JC, Tansey KE, et al. Application of electrophysiological measures in
spinal cord injury clinical trials: a narrative review. Spinal Cord. 2019;57:909–23. Article PubMed Google Scholar * Balbinot G, Li G, Wiest MJ, Pakosh M, Furlan JC, Kalsi-Ryan S, et al.
Properties of the surface electromyogram following traumatic spinal cord injury: a scoping review. J Neuroeng Rehabil. 2021;18:105. Article PubMed PubMed Central Google Scholar *
Balbinot G, Joner Wiest M, Li G, Pakosh M, Cesar Furlan J, Kalsi-Ryan S et al. The use of surface EMG in neurorehabilitation following traumatic spinal cord injury: a scoping review. Clin
Neurophysiol https://doi.org/10.1016/j.clinph.2022.02.028 2022. * World Health Organization. International classification of functioning, disability and health: ICF. 2001. * Sheffler LR,
Chae J. Neuromuscular electrical stimulation in neurorehabilitation. Muscle Nerve. 2007;35:562–90. Article PubMed Google Scholar * Anderson KD, Wilson JR, Korupolu R, Pierce J, Bowen JM,
O’Reilly D, et al. Multicentre, single-blind randomised controlled trial comparing MyndMove neuromodulation therapy with conventional therapy in traumatic spinal cord injury: a protocol
study. BMJ Open. 2020;10:e039650. Article PubMed PubMed Central Google Scholar * Committee A. and IscIS. The 2019 revision of the International Standards for Neurological Classification
of Spinal Cord Injury (ISNCSCI)—what’s new? Spinal Cord. 2019;57:815–7. Article Google Scholar * Hislop H, Montgomery J. Daniels and Worthingham’s muscle testing: techniques of manual
examination. 6th Edn. WB Saunders: Philadelphia, 1995. * Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G, Ray G. Development of recommendations for SEMG sensors and sensor placement
procedures. J Electromyogr Kinesiol. 2000;10:361–74. Article CAS Google Scholar * Perotto A. Anatomical guide for the electromyographer: the limbs and trunk. 5th. Charles C. Thomas, 2011.
* Maffiuletti NA, Roig M, Karatzanos E, Nanas S. Neuromuscular electrical stimulation for preventing skeletal-muscle weakness and wasting in critically ill patients: a systematic review.
BMC Med. 2013;11:137. Article PubMed PubMed Central Google Scholar * Cremoux S, Tallet J, Dal Maso F, Berton E, Amarantini D. Impaired corticomuscular coherence during isometric elbow
flexion contractions in humans with cervical spinal cord injury. Eur J Neurosci. 2017;46:1991–2000. Article PubMed Google Scholar * Thongpanja S, Phinyomark A, Phukpattaranont P, Limsakul
C. Mean and median frequency of EMG signal to determine muscle force based on time-dependent power spectrum. Electron Electr. Eng 2013; 19. https://doi.org/10.5755/j01.eee.19.3.3697. *
Baker SN, Chiu M, Fetz EE. Afferent encoding of central oscillations in the monkey arm. J Neurophysiol. 2006;95:3904–10. Article PubMed Google Scholar * Beaumont E, Guevara E, Dubeau S,
Lesage F, Nagai M, Popovic M. Functional electrical stimulation post-spinal cord injury improves locomotion and increases afferent input into the central nervous system in rats. J Spinal
Cord Med. 2014;37:93–100. Article PubMed PubMed Central Google Scholar * Hahm SC, Yoon YW, Kim J. High-frequency transcutaneous electrical nerve stimulation alleviates spasticity after
spinal contusion by inhibiting activated microglia in rats. Neurorehabil Neural Repair. 2015;29:370–81. Article PubMed Google Scholar * Oba M. Histological changes, muscle force and
fatigability after electrical stimulation to experimentally paralyzed muscles]. Nihon Seikeigeka Gakkai Zasshi. 1995;69:708–20. CAS PubMed Google Scholar * Butezloff MM, Zamarioli A,
Maranho DA, Shimano AC. Effect of electrical stimulation and vibration therapy on skeletal muscle trophism in rats with complete spinal cord injury. Am J Phys Med Rehabil. 2015;94:950–7.
Article PubMed Google Scholar * de Freitas GR, Santo CC, do E, de Machado-Pereira NAMM, Bobinski F, dos Santos ARS, et al. Early cyclical neuromuscular electrical stimulation improves
strength and trophism by Akt pathway signaling in partially paralyzed biceps muscle after spinal cord injury in rats. Phys Ther. 2018;98:172–81. Article PubMed Google Scholar * Maughan
RJ, Nimmo MA. The influence of variations in muscle fibre composition on muscle strength and cross-sectional area in untrained males. J Physiol. 1984;351:299–311. Article CAS PubMed
PubMed Central Google Scholar * Aguiar SA, Baker SN, Gant K, Bohorquez J, Thomas CK. Spasms after spinal cord injury show low-frequency intermuscular coherence. J Neurophysiol.
2018;120:1765–71. Article CAS PubMed PubMed Central Google Scholar * Signorile JF, Banovac K, Gomez M, Flipse D, Caruso JF, Lowensteyn I. Increased muscle strength in paralyzed patients
after spinal cord injury: effect of beta-2 adrenergic agonist. Arch Phys Med Rehabil. 1995;76:55–58. Article CAS PubMed Google Scholar * Zoghi M, Galea M. Brain motor control assessment
post early intensive hand rehabilitation after spinal cord injury. Top Spinal Cord Inj Rehabil. 2018;24:157–66. Article PubMed Google Scholar * Gesslbauer B, Hruby LA, Roche AD, Farina
D, Blumer R, Aszmann OC. Axonal components of nerves innervating the human arm. Ann Neurol. 2017;82:396–408. Article CAS PubMed Google Scholar * Rushton DN. Functional electrical
stimulation and rehabilitation-an hypothesis. Med Eng Phys. 2003;25:75–8. Article CAS PubMed Google Scholar * Carson RG, Buick AR. Neuromuscular electrical stimulation-promoted
plasticity of the human brain. J Physiol. 2021;599:2375–99. Article CAS PubMed Google Scholar * Del Vecchio A, Holobar A, Falla D, Felici F, Enoka RM, Farina D. Tutorial: analysis of
motor unit discharge characteristics from high-density surface EMG signals. J Electromyogr Kinesiol. 2020;53:102426. Article PubMed Google Scholar * Mang CS, Clair JM, Collins DF.
Neuromuscular electrical stimulation has a global effect on corticospinal excitability for leg muscles and a focused effect for hand muscles. Exp Brain Res. 2011;209:355–63. Article CAS
PubMed Google Scholar * Zhou R, Alvarado L, Kim S, Chong SL, Mushahwar VK. Modulation of corticospinal input to the legs by arm and leg cycling in people with incomplete spinal cord
injury. J Neurophysiol. 2017;118:2507–19. Article CAS PubMed PubMed Central Google Scholar * Laine CM, Valero-Cuevas FJ. Intermuscular coherence reflects functional coordination. J
Neurophysiol. 2017;118:1775–83. Article PubMed PubMed Central Google Scholar * Boonstra TW, Breakspear M. Neural mechanisms of intermuscular coherence: implications for the rectification
of surface electromyography. J Neurophysiol. 2012;107:796–807. Article PubMed Google Scholar * Jaiser SR, Baker MR, Baker SN. Intermuscular coherence in normal adults: variability and
changes with age. PLoS One. 2016;11:1–16. Article Google Scholar * Norton JA, Gorassini MA. Changes in cortically related intermuscular coherence accompanying improvements in locomotor
skills in incomplete spinal cord injury. J Neurophysiol. 2006;95:2580–9. Article PubMed Google Scholar * Silverman JD, Balbinot G, Masani K, Zariffa J. Validity and reliability of surface
electromyography features in lower extremity muscle contraction in healthy and spinal cord-injured participants. Top Spinal CordInj Rehabil. 2021;27:14–27. Article Google Scholar *
Calancie B, Molano R, Broton JG, Bean JA, Alexeeva N. Relationship between EMG and muscle force after spinal cord injury. J Spinal Cord Med. 2000;24:19–25. Article Google Scholar * Bryden
A, Kilgore KL, Nemunaitis GA. Advanced assessment of the upper limb in tetraplegia: a three-tiered approach to characterizing paralysis. Top Spinal Cord Inj Rehabil. 2018;24:206–16. Article
PubMed PubMed Central Google Scholar * Sherwood AM, Dimitrijevic MR, McKay WB. Evidence of subclinical brain influence in clinically complete spinal cord injury: discomplete SCI. J
Neurol Sci. 1992;110:90–8. Article CAS PubMed Google Scholar Download references ACKNOWLEDGEMENTS This work was supported in part by the Wings for Life Spinal Cord Research Foundation
(Project #210). We would like to thank MyndTec Inc. and their sponsored clinical trial “Restoration of Reaching and Grasping Function in Individuals With Spinal Cord Injury Using MyndMove®
Neuromodulation Therapy” (USAMRAA CDMRP-SCRIP—Protocol SC150251, Clinicaltrials.gov: NCT 03439319) for access to individuals receiving FEST. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS *
KITE Research Institute, University Health Network, Toronto, ON, M5G 2A2, Canada Gustavo Balbinot, Guijin Li, Cindy Gauthier, Kristin E. Musselman, Sukhvinder Kalsi-Ryan & José Zariffa *
Institute of Biomedical Engineering, University of Toronto, Toronto, ON, Canada Guijin Li & José Zariffa * Department of Physical Therapy, University of Toronto, Toronto, ON, Canada
Cindy Gauthier, Kristin E. Musselman & Sukhvinder Kalsi-Ryan * Rehabilitation Sciences Institute, University of Toronto, Toronto, ON, Canada Kristin E. Musselman, Sukhvinder Kalsi-Ryan
& José Zariffa * Edward S. Rogers Sr. Department of Electrical and Computer Engineering, University of Toronto, Toronto, ON, Canada José Zariffa Authors * Gustavo Balbinot View author
publications You can also search for this author inPubMed Google Scholar * Guijin Li View author publications You can also search for this author inPubMed Google Scholar * Cindy Gauthier
View author publications You can also search for this author inPubMed Google Scholar * Kristin E. Musselman View author publications You can also search for this author inPubMed Google
Scholar * Sukhvinder Kalsi-Ryan View author publications You can also search for this author inPubMed Google Scholar * José Zariffa View author publications You can also search for this
author inPubMed Google Scholar CONTRIBUTIONS G.B. collected data, carried out analysis, interpreted and wrote the results and figures, and wrote the first draft of the manuscript. G.L.
contributed to manuscript drafting and analysis. C.G. contributed to data collection. J.Z., S.K.R., and K.E.M. supervised the study and contributed to the analysis and drafting of the
manuscript. All authors edited and approved the final manuscript. CORRESPONDING AUTHOR Correspondence to Gustavo Balbinot. ETHICS DECLARATIONS CONFLICT OF INTEREST The authors declare no
competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
SUPPLEMENTARY INFORMATION SUPPLEMENTARY MATERIAL FIGURE S1 FIGURE S2 FIGURE S3 FIGURE S4 REPRODUCIBILITY CHECKLIST RIGHTS AND PERMISSIONS Springer Nature or its licensor (e.g. a society or
other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of
this article is solely governed by the terms of such publishing agreement and applicable law. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Balbinot, G., Li, G., Gauthier, C.
_et al._ Functional electrical stimulation therapy for upper extremity rehabilitation following spinal cord injury: a pilot study. _Spinal Cord Ser Cases_ 9, 11 (2023).
https://doi.org/10.1038/s41394-023-00568-4 Download citation * Received: 27 April 2022 * Revised: 14 March 2023 * Accepted: 16 March 2023 * Published: 01 April 2023 * DOI:
https://doi.org/10.1038/s41394-023-00568-4 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative