- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT DESIGN Systematic review and meta-analysis. BACKGROUND AND PURPOSE Traditional forms of upper-body moderate intensity exercise consistently provide little cardiovascular benefits
for persons with spinal cord injury (PwSCI). Explorations of new training methods are vital to improve cardiovascular fitness among PwSCI. This study sought to evaluate the effectiveness of
vigorous training on cardiorespiratory fitness in PwSCI. METHODS Database search through PubMed, Web of Science, Scopus, SportDiscus, and Cumulative Index of Nursing and Allied Health
Literature (CINAHL) was conducted from the databases’ inception to November 2020 to identify relevant exercise studies with PwSCI. Two independent reviewers screened articles for inclusion.
Data were extracted from included studies and methodological quality evaluated. RESULTS Sixteen trials (eight pre-post trials and eight controlled trials [CTs]) with a total of 145
participants were analyzed. Results from pre-post studies revealed significant improvements in cardiorespiratory fitness following high-intensity interval training (HIIT) (Peak Oxygen Uptake
[VO2peak], standardized mean difference [SMD] = 0.81; 95% CI 0.23–1.39; _P_ < 0.01 and Peak Power Output [PPO], SMD = 0.91; 95% CI 0.32–1.5; _P_ < 0.01) and circuit resistance
training (CRT) (VO2peak, MD = 0.38; 95% CI 0.19–0.57; _P_ < 0.01 and PPO, MD = 20.17; 95% CI 8.26–32.08; _P_ < 0.01). Meta-analysis of CTs did not demonstrate significant improvements
in cardiorespiratory fitness following vigorous training interventions in comparison to lower intensity training interventions. CONCLUSION Evidence from HIIT and CRT interventions suggest
benefits for cardiovascular functions; however, vigorous training was not more beneficial than other forms of endurance training. More CTs are needed to better understand the effectiveness
of vigorous training on cardiorespiratory fitness in PwSCI. You have full access to this article via your institution. Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS VIABILITY OF HIGH
INTENSITY INTERVAL TRAINING IN PERSONS WITH SPINAL CORD INJURY—A PERSPECTIVE REVIEW Article 01 June 2020 RETHINKING AEROBIC EXERCISE INTENSITY PRESCRIPTION IN ADULTS WITH SPINAL CORD INJURY:
TIME TO END THE USE OF “MODERATE TO VIGOROUS” INTENSITY? Article Open access 08 December 2021 HIGH INTENSITY FUNCTIONAL TRAINING FOR PEOPLE WITH SPINAL CORD INJURY & THEIR CARE PARTNERS
Article Open access 22 March 2024 INTRODUCTION As nearly 18,000 new traumatic spinal cord injury (SCI) cases occur each year in the United States in predominantly young adults, the overall
population of persons with chronic SCI (PwSCI) continues to grow and currently exceeds 300,000 [1]. Unfortunately, as the prevalence of SCI grows, so do rates of cardiovascular disease (CVD)
[2]. Complications related to CVD (i.e., heart attack, stroke, and heart failure) has recently emerged as the focal cause of premature death in PwSCI [2], becoming a worldwide epidemic and
health concern. Even with the development and revision of physical activity guidelines for PwSCI (PAG-SCI) to combat the grim cardiopulmonary outcomes related to SCI [2], guidelines have not
appeared to sufficiently improve this population’s cardiovascular heath [3]. Several reasons could explain the dismal improvements associated with the PAG-SCI [3]. First, the PAG-SCI
recommend a minimum of 30 min of moderate intensity aerobic exercise three times per week (90 min/week), roughly 66% lower than recommendations by the American College of Sport Medicine
(ACSM) for the general population [4]. ACSM recommendations are also built around lower body exercises (i.e., running, swimming, and biking), while PAG-SCI targets the upper body. As the
legs elicit a greater cardiovascular response than the arms during exercise [5], it seems unlikely that the PAG-SCI—which recommend reduced volumes for less efficient exercises—would elicit
positive outcomes. Many PwSCI are also limited in overall cardiac output capacity [6], making prolonged exercise unsustainable and central cardiovascular adaptations unlikely. As the PAG-SCI
prescribes an extensive amount of prolonged exercise, it makes sense that minimal cardiovascular improvements accompany these guidelines [3]. Attention must be shifted to exercise modes
calibrated to the unique physiology of persons with SCI to maximize health benefits [5, 6]. Specifically, we must adjust upper limb-based exercise to efficiently stimulate the cardiovascular
system without increasing upper limb injury risk. As vigorous exercise typically requires less time and incorporates more periods of recovery than traditional forms of aerobic training,
this exercise method may offer a solution. Rest/recovery periods built within several vigorous protocols may also reduce injury risk by allowing active soft tissue to recover in between
periods of physical exertion [7, 8], enabling individuals to reach higher workloads compared to those of prolonged, continuous movement. Exercise at a vigorous intensity can be defined as
activity which elicits a training response >70% Peak Heart Rate (HRpeak), 60% Heart Rate Reserve, 64% Peak Oxygen Uptake (VO2peak), or 14 Rate of Perceived Exertion (RPE) [4, 9]. In the
general population, vigorous training has exhibited comparable benefits to moderate intensity exercise in just half the time [9, 10]. Vigorous intensity exercise provokes peripheral
mitochondrial adaptations, which may compensate for the central cardiovascular inefficiencies of upper extremity exercise in PwSCI [5, 6]. Recently, several researchers have examined various
types of vigorous training protocols like circuit resistance training (CRT) [11]—resistance training broken up with low intensity arm ergometry—and high-intensity interval training
(HIIT)—explosive anaerobic bursts broken up with low intensity exercise [12]—exhibiting superior cardiovascular benefits to moderate intensity exercise [11, 12]. Vigorous intensity exercise
presents a potentially promising alternative to traditional forms of endurance exercise in PwSCI. Systematic reviews in the able-bodied population show superior cardioprotective benefits
following vigorous intensity exercise versus moderate intensity exercise [13, 14]. However, in PwSCI, recent systematic reviews have grouped moderate and vigorous intensity exercise together
to explore PAG-SCI efficacies [2, 15]. Therefore, this will be the first systematic review evaluating the effectiveness of vigorous intensity training compared to moderate intensity
training in PwSCI. We predict that vigorous intensity protocols such as HIIT will lead to the greatest improvements in VO2peak and peak power output (PPO) as the incorporation of recovery
periods will enable PwSCI to maximize exercise bursts within training sessions. METHODS PROTOCOL AND REGISTRATION The Cochrane Handbook [16] was followed to conduct the systematic review and
meta-analysis and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis [17] checklist was used to guide the reporting. The study protocol was registered with the
International Prospective Registry of Systematic Reviews (PROSPERO): CRD 42020171181. DATA SOURCES AND SEARCH STRATEGY The databases search on PubMed, Web of Science, Scopus, SportDiscus and
Cumulative Index to Nursing and Allied Health Literature (CINAHL) was conducted from their inception to April 2020 and updated in November 2020 to identify relevant exercise studies in
PwSCI. In the PubMed database, we used MeSH terms combined with keywords including spinal cord injuries, paraplegia, tetraplegia, cardiorespiratory fitness, CVDs, cardiovascular, physical
capacity and oxygen consumption, HIIT, circuit training, training intensity, high-intensity hybrid training, high-intensity virtual reality, physical education, and training. Search
strategies were adjusted for each database. Filters were implemented to exclude animal studies and reviews. See Supplementary Appendix I for full search strategies. Two review authors (KD
and JP) independently screened relevant titles and abstracts to tag potential articles in which PwSCI were engaged in vigorous intensity interventions and cardiovascular fitness markers such
as VO2, heart rate, and power output were measured. If articles fulfilled these initial criteria, the full text of the article was obtained. Then, two review authors (AA and JP)
independently screened articles using the preestablished eligibility criteria to identify the trials analyzed in this review. Ancestor and descendant searching were utilized to find other
relevant studies which qualified for inclusion. Any discordance was resolved through discussion with a third author (LA). ELIGIBILITY CRITERIA Inclusion and exclusion criteria were based on
the Participants, Interventions, Comparators, Outcomes, and Study designs framework. PARTICIPANTS We included studies involving adults (≥18 years old) with SCI, regardless of time since
injury, level, and completeness of injury. We excluded studies involving individuals with other neurological or cardiometabolic disease. INTERVENTIONS We included studies examining various
forms of vigorous, aerobic and resistance training. This included training modes such as HIIT, sprint interval training (SIT), CRT, respiratory muscular endurance training (RMET) and
vigorous continuous training (VICT). HIIT protocols consisted of explosive anaerobic bursts broken up with periods of low intensity exercise. SIT consisted of maximal exercise broken up with
rest. CRT consisted of resistance training broken up with low intensity arm ergometry. RMET consisted of a 30 min continuous bout of exercise to exhaustion. VICT consisted of a continuous
bout of high-intensity exercise. We excluded studies which only examined the effects of moderate and light forms of exercise, defined by ACSM as 30–59% Heart Rate Reserve, 37–63% VO2peak,
57–76% HRmax, and 9–13 RPE [4]. COMPARATORS We included studies comparing: * Vigorous intensity training modes versus control (light-to-moderate intensity training or routine training
patterns). * Pre-post vigorous intensity training modes with no control group. We considered conventional moderate intensity continuous training (MICT) to be continuous exercise in
accordance with ACSM and American Heart Association guidelines [4, 9], which describes moderate intensity as exercise within 40–59% Heart Rate Reserve, 64–70% HRmax, 46–63% VO2max, or RPE
12–13. OUTCOMES We chose to evaluate training adaptations to VO2peak, PPO, and peak minute ventilation (VEpeak). These outcome measures are common measurements of maximal exercise capacity
and can be used to predict an individual’s CVD risk [4]. VO2peak is the peak oxygen uptake response during a graded exercise test upon volitional fatigue and test termination. PPO is the
maximum workload sustained during the graded exercise test when VO2peak occurs. VEpeak is the maximum volume of air expired during the VO2peak assessment. Studies were included if they
clearly stated that VO2peak, PPO, or VEpeak were measured during a maximal exercise test. STUDY DESIGNS Both randomized and nonrandomized (i.e., pre-post trials) clinical trials were
included in this review. We excluded case study reports and preliminary reports. All studies were required to be published in English, French, Spanish, or Portuguese. JP and KD identified if
studies’ participants, interventions, comparators, and study designs met these criteria, with discordances resolved by LA. JP and AS identified the relevant outcomes, with discordances
resolved by LA. DATA EXTRACTION Data extracted independently by two reviewers (KD and JP) were consolidated into an Excel spreadsheet table, tailored for this review. Discrepancies were
resolved through discussion with a third author (LA). Data extraction included: study ID, study design, intervention comparison (i.e., experimental vs. control conditions), dosage (duration
and frequency), participant characteristics (sample size, age, gender, AIS score, injury level), outcome measures related to cardiorespiratory fitness and a summary of the study’s main
findings related to cardiovascular fitness. QUALITY ASSESSMENT The Cochrane Risk of Bias Tool was used to assess the selection bias, performance bias, detection bias, attrition bias,
reporting bias, and other biases of the included controlled trials (CT). Each study was rated as “high”, “low”, or “unclear” risk of bias [16]. The Quality Assessment Tool for Before-After
(pre-post) Studies with no Control Group was used to assess the pre-post trials [18]. This tool rates the quality of 12 items related to the: (1) study question, (2) eligibility criteria and
study population, (3) population of interest representation, (4) eligibility of participants, (5) sample size, (6) intervention clarity, (7) outcome measure clarity, (8) blinding of
researchers, (9) follow-up rates, (10) statistical analysis, (11) repeating of outcome measurements, and (12) group-level interventions and individual-level outcome efforts. All 12 items
were scored as “yes”, “no”, “cannot determine” (CD), “not applicable” (NA), or “not reported” (NR). Overall scientific quality of the pre-post trials was further assessed as good, fair, or
poor. AA and JP independently assessed all included studies, with consensus reached through discussion with LA. STATISTICAL ANALYSIS Meta-analysis was performed to pool studies with similar
comparisons while also accounting for study differences in training design, dosage, and participant characteristics. All data analysis was conducted using Review Manager version 5.3.5
(Cochrane, London, UK). Changes in mean scores and standard deviation (SD) were extracted from all CTs to estimate the mean effect and 95% CI. In case SD was not reported, it was estimated
according to the Cochrane handbook [16]. _I_2 was used to determine statistical heterogeneity between studies [16]. Because of low heterogeneity (_I_2 = 0%), the fixed effect model (FEM) was
used for meta-analysis of CT. When less optimal outcomes were reflected in higher scores, the data were transformed to have a consistent direction indicating optimal clinical outcomes. For
pre-post studies included in the meta-analysis, baseline data was compared to post-intervention data. Because of low heterogeneity (_I_2 = 0%), FEM analysis was conducted [16]. Mean
difference (MD) was used to estimate the effect size when only one outcome measure (e.g., VO2peak) was pooled in a meta-analysis and standardized mean difference (SMD) was used when
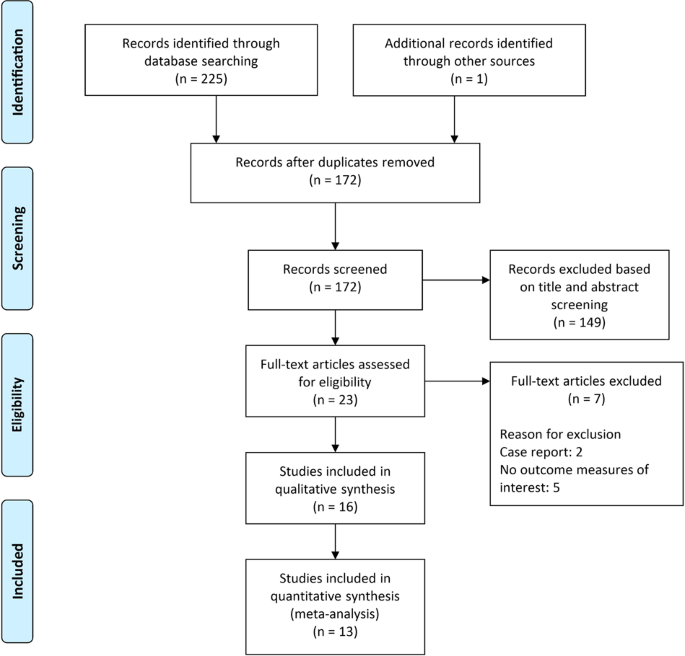
different outcome measures (e.g., VO2peak and PPO) were pooled together in the same meta-analysis [16]. RESULTS SEARCH PROCESS The search retrieved 225 articles. One article was found
through ancestor and descendant searching. Following the removal of duplicates and screening of titles and abstracts, 23 articles were assessed for eligibility. After further analysis, 16
studies were deemed fully eligible for systematic review inclusion with 13 of these articles included in the meta-analysis. Three CTs by McLeod et al., Fischer et al., and Kressler et al.
were not included in the meta-analysis due to incomplete data, unique outcome measures, or study design differences [19,20,21]. Figure 1 illustrates the stages of study selection.
CHARACTERISTICS OF INCLUDED STUDIES Data from the 16 eligible studies are included in Table 1. Eight studies were pre-post trials and the other eight studies were CTs [11, 12,
22,23,24,25,26,27]. A total of 145 participants with lesion levels from C2-L5 and American Spinal Injury Association Impairment Scale (AIS) A, B, C, and D were studied. Participants were
mostly males (83%). Eight studies utilized HIIT [12, 22,23,24, 27,28,29,30], four utilized CRT [11, 21, 25, 26], two VICT [31, 32], one SIT [19], and one RMET [20]. Two HIIT-based studies
incorporated the use of functional electric stimulation of the lower extremities with one of these studies also incorporating virtual reality into the training protocol [23, 24]. The main
outcome measures analyzing cardiorespiratory fitness were derived from incremental exercise tests to exhaustion. The cardiorespiratory measures of VO2peak, VEpeak, and PPO were analyzed in
the meta-analysis. QUALITY OF STUDIES Results for the risk of bias assessment for CTs can be found in Table 2. Four of the eight CTs presented with a low risk of bias [19, 20, 31, 32]. Of
these studies, two were included in the meta-analysis [31, 32]. McLeod et al.’s and Fischer et al.’s studies were excluded from meta-analysis due to design differences [19, 20]. The most
common biases in the CTs were selective reporting bias and “other biases”. Results of the quality assessment for the pre-post studies with no control group can be found in Table 3. Overall,
three of the eight pre-post studies were rated as having good quality [11, 25, 26], while the other five were rated as having fair quality [12, 22,23,24, 27]. EFFECT OF VIGOROUS INTENSITY
EXERCISE INTERVENTIONS HIGH-INTENSITY INTERVAL TRAINING Figure 2a includes five pre-post design studies examining the effect of HIIT interventions on cardiorespiratory fitness [12, 22,23,24,
27]. The five studies were rated as having fair overall methodological quality. They were pooled in three meta-analyses (FEM) analyzing VO2peak, VEpeak, PPO, and with results expressed as
SMD and MD. The analysis of VO2peak revealed a significant difference before and after HIIT (SMD = 0.81; 95% CI 0.23–1.39; _P_ < 0.01). Similarly, the analysis of PPO revealed a
significant difference before and after HIIT (SMD = 0.91; 95% CI 0.32–1.5; _P_ < 0.01). In contrast, VEpeak did not show a significant difference. However, the combination of these three
meta-analyses showed a statistically significant pre- and post-training difference (SMD = 0.69; 95% CI 0.35–1.04; _P_ < 0.01). Figure 2b includes three CTs that examined the effect of a
HIIT intervention compared to MICT or low intensity interval training [28,29,30]. All three studies presented with a unclear risk of bias. The three were pooled in two meta-analyses
analyzing VO2peak and PPO with the results expressed as SMD. The meta-analysis did not show a significant between-group difference for VO2peak (SMD = 0.14; 95% CI −0.73–1.01; _P_ > 0.05)
or PPO (SMD = 0.09; 95% CI −0.94–1.12; _P_ > 0.05). CIRCUIT RESISTANCE TRAINING Figure 3a includes three pre-post studies examining the effect of a CRT intervention on VO2peak [11, 25,
26]. The three studies were rated as having good overall methodological quality. They were pooled in two meta-analyses with results expressed as MD. VO2peak was statistically different
following the CRT intervention (MD = 0.38; 95% CI 0.19–0.57; _P_ < 0.01). Figure 3a includes two pre-post studies examining PPO. Results also revealed statistically significant mean
changes (MD = 20.17; 95% CI 8.26–32.08; _P_ < 0.01). VIGOROUS INTENSITY CONTINUOUS TRAINING Figure 3b includes two CTs that examined the effects of VICT compared to MICT or resistance
training (RT) [31, 32]. Both studies showed a low risk of bias. They were pooled in a meta-analysis with the results expressed as SMD. The meta-analysis of VICT did not show a significant
between-group difference for VO2peak (SMD = −0.03; 95% CI −0.76–0.70; _P_ > 0.05). TRIALS NOT INCLUDED IN META-ANALYSIS The reasons these studies were excluded from meta-analysis were
missing data, grouping differences, or design differences. The CT by Fischer et al. did not reveal significant improvements related to VO2peak or PPO, however, 4 weeks of RMET significantly
improved VEpeak [20]. Similarly, the double-blind CT by Kressler et al. revealed statistically significant improvements in VO2peak following a 6-month CRT protocol [21]. Further, individuals
who ingested protein immediately following training significantly improved VO2peak compared to individuals who did not. The CT by Mcleod et al. revealed significant PPO improvements
following a 5-week SIT protocol compared to MICT [19]. DISCUSSION As the need to discover more effective modes of achieving cardiovascular fitness in PwSCI becomes essential, the purpose of
this systematic review and meta-analysis was to investigate the literature related to the effectiveness of vigorous training interventions on cardiorespiratory fitness of PwSCI. Our
meta-analysis of pre-post studies indicates significant differences of VO2peak and PPO after HIIT and CRT. The differences were also clinically significant as all increments in VO2peak after
HIIT and CRT exceed 6%. Every 6% increase in VO2peak has been related to reduced cardiovascular complications including reduced cardiovascular mortality [33]. No significant differences
were observed when vigorous intensity exercises were compared to low and moderate intensity exercises. The first of our meta-analyses revealed the effectiveness of HIIT. HIIT resulted in
significant improvements in VO2peak and PPO over time. These findings are in accordance with Nightingale’s position that HIIT is both an optimal and viable exercise option for PwSCI [10].
After HIIT, VO2peak, and PPO significantly improved with no adverse consequences reported by participants, and low evidence of musculoskeletal injury or autonomic dysreflexia complications.
Brurok et al. reported latent shoulder dysfunction in two participants during the HIIT intervention, but following rest and therapy, they were able to safely complete the intervention [23].
Overall, our findings are in agreement with the review by Batacan et al. [34] that showed similar improvements in VO2peak among able-bodied adults following HIIT. As these pre-post
experiments did not utilize a control group, results should be interpreted with caution, and it is difficult to conclude whether cardiovascular improvements were due solely to the
intervention. The meta-analysis comparing HIIT with low-to-moderate intensity exercise did not reveal significant differences in cardiorespiratory adaptations. SMD in VO2peak and PPO was not
different across exercise modes. We must note that sample sizes were small across studies as many experimental groups did not consist of more than three participants. Further examination of
these studies also indicates a high risk of bias as differences in group pre-training fitness levels appear to exist. For example, in Graham et al.’s study on HIIT versus MICT,
pre-intervention fitness levels were higher in the HIIT group than the MICT group [30]. Low-fitness groups typically experience the greatest improvements from exercise interventions [35].
Further examination of the various HIIT interventions also suggests that exercise volumes may have influenced HIIT’s efficacy. For example, the most demanding HIIT protocol, by de Groot et
al. elicited the largest VO2peak improvement (50%) [28], while the least demanding HIIT protocol, by Graham et al. elicited minimal improvements (7%) [30]. In Graham et al.’s study, exercise
protocols were 225% greater in duration for the MICT group (90 min/week) than the HIIT group (40 min/week), which may also explain why greater improvements were observed in the MICT group.
While the PAG-SCI recommend at least 90 min per week of moderate intensity aerobic exercise, the guideline prescribes just 40 min of moderate intensity aerobic exercise if two strength
sessions are incorporated into the weekly exercise program [2]. As 40 min of vigorous intensity exercise revealed minimal improvements, it seems logical that moderate intensity aerobic
exercise of the same duration would also be ineffective [3]. According to Collins et al. when vigorous and moderate handcycling efforts are matched for time, vigorous intensity workloads are
~40% greater [36]. Therefore, if only 40 min/week of aerobic exercise is going to be prescribed, future recommendations must emphasize a need to raise overall exercise intensities to reach
adequate exercise volumes [10]. The meta-analysis also revealed significant improvements in VO2peak and PPO after exposure to CRT. Unlike HIIT, CRT has not revealed clear benefits for
improving cardiorespiratory fitness in able-bodied individuals. For example, Myers et al. revealed significant improvements in both VO2peak and PPO following a 5-week CRT [37], but Maiorana
et al. [38] did not observe any cardiorespiratory improvements following a 10-week CRT intervention. However, Myers et al. [37] studied CRT in able-bodied females only, while Maiorana et al.
studied it in able-bodied males only [38]. Our meta-analysis only included pre-post CRT studies among males with SCI [11, 25, 26], highlighting the need for more robust work examining CRT
in both genders with SCI. No differences in cardiorespiratory adaptations emerged when VICT was compared to moderate continuous or RT. Although differences were low, across studies, it must
be noted that Hooker and Wells’ study was unusual and utilized three out of six participants in both the vigorous and moderate intensity protocols by separating their interventions with an
8-week detraining period [31]. While this technique increases the overall sample size, detraining periods may be insufficient in preventing carry-over effects as trained groups present
better fitness and regain adaptations much easier than untrained groups [39]. Additionally, aerobic adaptations may be less affected by detraining [40]. Therefore, the use of detraining
strategies makes their findings difficult to interpret. It also seems plausible that VICT and RT elicited similar results due to the peripheral adaptations associated with both RT and
vigorous endurance training. The rest periods of RT also enable participants to tolerate greater loads which over time stimulates peripheral muscle and mitochondrial growth [6]. In the
meta-analysis, no specific mode of vigorous training was more effective than low-to-moderate modes of training. These findings do not support our hypothesis that HIIT and other vigorous
modes that incorporate recovery periods better optimize cardiorespiratory fitness in PwSCI. Moving forward, more work with broader demographics and sample sizes is needed to validate the
current results. The three studies which were left out of the meta-analysis showed meaningful cardioprotective benefits. According to Kressler et al. VO2peak significantly improved following
a 6-month CRT intervention, with greatest improvements in those who ingested protein immediately post workout [21]. As adequately timed protein supplementation enhances muscle anabolism in
able-bodied populations [41], this finding further supports the idea that peripheral adaptations enhance cardiovascular fitness in PwSCI. McLeod et al. observed greater improvements in PPO
following a 5-week SIT intervention in patients with acute SCI [19]. However, due to the acute nature of the SCI, it is difficult to determine if improvements in PPO were due to the training
intervention or the typical rehabilitation and recovery processes which follow SCI. Lastly, Fischer et al. observed significant improvements in VEpeak following RMET [20]. The unique RMET
protocol used prevented inclusion of this study in the meta-analysis. It should also be noted that all participants in this study were competitive hand-cyclists. Due to the ceiling effects
of chronic training, improvements in VEpeak support RMET as a potential effective option for the general populations of PwSCI. LIMITATIONS There are several limitations in this systematic
review and meta-analysis. First, individuals of various injury levels and AIS classifications were included. Due to the complex nature of a SCI, an individual with a complete high-thoracic
level injury and tetraplegia will likely have different cardiovascular responses to exercise than someone an incomplete and/or lower-level injury and full torso and autonomic (i.e., heart
rate, respiratory rate, etc.) function [42]. Therefore, results should be interpreted with caution as response to exercise will vary depending on level of injury and/or AIS classification
[43]. Next, only five CTs were eligible for meta-analysis. This low number reduces generalization of the findings. Further, the protocols and durations between similar training styles
differed across studies. For example, both Gauthier et al. and de Groot et al. used HIIT in their protocols, however, Gauthier et al. conducted HIIT utilizing manual wheelchair propulsion
for 6 weeks [29], while de Groot et al. conducted HIIT on an upper-body cycle ergometer for 8 weeks [28]. Another important limitation of this review is the inclusion of pre-post
interventions. We cannot fully determine the true effect of vigorous intensity training based on pre-post studies. CONCLUSION This systematic review and meta-analysis revealed significant
improvements in cardiorespiratory fitness in PwSCI after engaging in HIIT and CRT. As nearly all vigorous intensity interventions appeared to produce clinically significant improvements in
cardiorespiratory fitness, PwSCI may benefit from incorporating vigorous intensity exercises into their weekly physical activity regimes. However, no statistically significant differences
were found when comparing these strenuous exercise modalities to standard moderate intensity training. Many of the reviewed CTs included small sample and participants with low fitness,
highlighting the need for higher quality study designs examining the effect of different exercise intensities on fitness. Future randomized CTs should focus on increasing sample sizes and
recruiting active PwSCI. Nonetheless, this systematic review and meta-analysis highlights the importance of physical activity in improving cardiorespiratory fitness in PwSCI. REFERENCES *
National Spinal Cord Injury Statistical Center. Spinal cord injury facts and figures at a glance. Birmingham: University of Alabama at Birmingham; 2016. * Martin Ginis KA, van der Scheer JW,
Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord.
2018;56:308–21. Article Google Scholar * Totosy de Zepetnek JO, Pelletier CA, Hicks AL, MacDonald MJ. Following the physical activity guidelines for adults with spinal cord injury for 16
weeks does not improve vascular health: a randomized controlled trial. Arch Phys Med Rehabil. 2015;96:1566–75. Article Google Scholar * American College of Sports Medicine. ACSM’s exercise
testing and prescription. Philadelphia: Lippincott Williams & Wilkins; 2017. * Theisen D. Cardiovascular determinants of exercise capacity in the Paralympic athlete with spinal cord
injury. Exp Physiol. 2012;97:319–24. Article Google Scholar * Devillard X, Rimaud D, Roche F, Calmels P. Effects of training programs for spinal cord injury. Ann Readapt Med Phys.
2007;50:490–8. 480–9 Article CAS Google Scholar * Donatelli RA. Physical therapy of the shoulder. 5th ed. London: Churchill Livingstone; 2011.
https://www.elsevier.com/books/physical-therapy-of-the-shoulder/donatelli/978-1-4377-0740-3. * Maffulli N, Renström P, Leadbetter WB. Tendon injuries. New York City: Springer; 2005. *
American Heart Association. Know your target heart rates for exercise, losing weight and health. 2015. https://www.heart.org. * Nightingale TE, Metcalfe RS, Vollaard NB, Bilzon JL. Exercise
guidelines to promote cardiometabolic health in spinal cord injured humans: time to raise the intensity? Arch Phys Med Rehabil. 2017;98:1693–704. Article Google Scholar * Jacobs PL, Nash
MS, Rusinowski JW. Circuit training provides cardiorespiratory and strength benefits in persons with paraplegia. Med Sci Sports Exerc. 2001;33:711–7. Article CAS Google Scholar * Le
Foll-de Moro D, Tordi N, Lonsdorfer E, Lonsdorfer J. Ventilation efficiency and pulmonary function after a wheelchair interval-training program in subjects with recent spinal cord injury.
Arch Phys Med Rehabil. 2005;86:1582–6. Article Google Scholar * Viana RB, Naves JPA, Coswig VS, de Lira CAB, Steele J, Fisher JP, et al. Is interval training the magic bullet for fat loss?
A systematic review and meta-analysis comparing moderate-intensity continuous training with high-intensity interval training (HIIT). Br J Sports Med. 2019;53:655. Article Google Scholar *
Swain DP, Franklin BA. Comparison of cardioprotective benefits of vigorous versus moderate intensity aerobic exercise. Am J Cardiol. 2006;97:141–7. Article Google Scholar * van der Scheer
JW, Martin Ginis KA, Ditor DS, Goosey-Tolfrey VL, Hicks AL, West CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury. Neurology. 2017;89:736. Article
Google Scholar * Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. Version 6.1.0. London: The Cochrane
Collaboration; 2020. www.training.cochrane.org/handbook. * Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma G. Preferred reporting items for systematic reviews and meta-analyses: the
PRISMA statement. PLoS med. 2009;6. * National Institute of Health. Study quality assessment tools [web page]. 2017. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. *
McLeod JC, Diana H, Hicks AL. Sprint interval training versus moderate-intensity continuous training during inpatient rehabilitation after spinal cord injury: a randomized trial. Spinal
Cord. 2020;58:106–15. Article Google Scholar * Fischer G, Tarperi C, George K, Ardigò LP. An exploratory study of respiratory muscle endurance training in high lesion level paraplegic
handbike athletes. Clin J Sport Med. 2014;24:69–75. Article Google Scholar * Kressler J, Burns PA, Betancourt L, Nash MS. Circuit training and protein supplementation in persons with
chronic tetraplegia. Med Sci Sports Exerc. 2014;46:1277–84. Article CAS Google Scholar * Bougenot MP, Tordi N, Betik AC, Martin X, Le Foll D, Parratte B, et al. Effects of a wheelchair
ergometer training programme on spinal-cord injured persons. Spinal Cord. 2003;41:451–6. Article Google Scholar * Brurok B, Helgerud J, Karlsen T, Leivseth G, Hoff J. Effect of aerobic
high-intensity hybrid training on stroke volume and peak oxygen consumption in men with spinal cord injury. Am J Phys Med Rehabil. 2011;90:407–14. Article Google Scholar * Hasnan N,
Engkasan JP, Husain R, Davis GM. High-intensity virtual-reality arm plus FES-leg interval training in individuals with spinal cord injury. Biomed Tech. 2013;58. * Nash MS, van de Ven I, van
Elk N, Johnson BM. Effects of circuit resistance training on fitness attributes and upper-extremity pain in middle-aged men with paraplegia. Arch Phys Med Rehabil. 2007;88:70–5. Article
Google Scholar * Nash MS, Jacobs PL, Mendez AJ, Goldberg RB. Circuit resistance training improves the atherogenic lipid profiles of persons with chronic paraplegia. J Spinal Cord Med.
2001;24:2–9. Article CAS Google Scholar * Tordi N, Dugue B, Klupzinski D, Rasseneur L, Rouillon JD, Lonsdorfer J. Interval training program on a wheelchair ergometer for paraplegic
subjects. Spinal Cord. 2001;39:532–7. Article CAS Google Scholar * de Groot PC, Hjeltnes N, Heijboer AC, Stal W, Birkeland K. Effect of training intensity on physical capacity, lipid
profile and insulin sensitivity in early rehabilitation of spinal cord injured individuals. Spinal Cord. 2003;41:673–9. Article Google Scholar * Gauthier C, Brosseau R, Hicks AL, Gagnon
DH. Feasibility, safety, and preliminary effectiveness of a home-based self-managed high-intensity interval training program offered to long-term manual wheelchair users. Rehabili Res Pract.
2018:8209360. * Graham K, Yarar-Fisher C, Li J, McCully K, Rimmer J, Powell D, et al. Effects of high-intensity interval training versus moderate-intensity training on cardiometabolic
health markers in individuals with spinal cord injury: a Pilot Study. Top Spinal Cord Inj Rehabil. 2019;25:248–59. Article Google Scholar * Hooker SP, Wells CL. Effects of low- and
moderate-intensity training in spinal cord-injured persons. Med Sci Sports Exerc. 1989;21:18–22. Article CAS Google Scholar * Jacobs PL. Effects of resistance and endurance training in
persons with paraplegia. Med Sci Sports Exerc. 2009;41:992–7. Article Google Scholar * Swank AM, Horton J, Fleg JL, Fonarow GC, Keteyian S, Goldberg L, et al. Modest increase in peak VO2
is related to better clinical outcomes in chronic heart failure patients: results from heart failure and a controlled trial to investigate outcomes of execise training. Circ Heart Fail.
2012;5:579–85. Article Google Scholar * Batacan RB, Duncan MJ, Dalbo VJ, Tucker PS, Fenning AS. Effects of high-intensity interval training on cardiometabolic health: a systematic review
and meta-analysis of intervention studies. Br J Sports Med. 2017;51:494. Article Google Scholar * Ahtiainen JP, Pakarinen A, Alen M, Kraemer WJ, Häkkinen K. Muscle hypertrophy, hormonal
adaptations and strength development during strength training in strength-trained and untrained men. Eur J Appl Physiol. 2003;89:555–63. Article CAS Google Scholar * Collins EG, Gater D,
Kiratli J, Butler J, Hanson K, Langbein WE. Energy cost of physical activities in persons with spinal cord injury. Med Sci Sports Exer. 2010;42:691–700. Article Google Scholar * Myers TR,
Schneider MG, Schmale MS, Hazell TJ. Whole-body aerobic resistance training circuit improves aerobic fitness and muscle strength in sedentary young females. J Strength Cond Res.
2015;29:1592–600. Article Google Scholar * Maiorana AJ, Briffa TG, Goodman C, Hung J. A controlled trial of circuit weight training on aerobic capacity and myocardial oxygen demand in men
after coronary artery bypass surgery. J Cardiopulm Rehabil Prev. 1997;17:239–47. Article CAS Google Scholar * Douda H, Kosmidou K, Smilios I, Volaklis K, Tokmakidis S. Community-based
training-detraining intervention in older women: a five-year follow-up study. J Aging Phys. 2014;23:496–512. Google Scholar * Carvalho MJ, Marques E, Mota J. Training and detraining effects
on functional fitness after a multicomponent training in older women. Gerontology. 2009;55:41–8. Article CAS Google Scholar * Andersen LL, Tufekovic G, Zebis MK, Crameri RM, Verlaan G,
Kjær M, et al. The effect of resistance training combined with timed ingestion of protein on muscle fiber size and muscle strength. Metabolism. 2005;54:151–6. Article CAS Google Scholar *
Holmlund T, Ekblom-Bak E, Franzén E, Hultling C, Wahman K. Energy expenditure after spinal cord injury in people with motor-complete tetraplegia or motor-complete paraplegia. Spinal Cord.
2018;56:274–83. Article Google Scholar * Holmlund, T, Ekblom-Bak, E, Franzen, E, Hutling, C, Wahman, K. Intensity of physical activity as a percentage of peak oxygen uptake, heart rate and
Borg RPE in motor-complete para- and tetraplegia. Plos ONE. 2019;14:e0222542. Article CAS Google Scholar Download references ACKNOWLEDGEMENTS We would like to thank the library services
at the University of Illinois at Urbana-Champaign for providing us with the databases and search strategies to conduct this research. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department
of Kinesiology and Community Health, College of Applied Health Sciences, University of Illinois at Urbana-Champaign, Urbana, IL, USA Joseph Peters, Libak Abou, Laura A. Rice, Kady
Dandeneau, Aditya Alluri, Amadeo Felix Salvador & Ian Rice Authors * Joseph Peters View author publications You can also search for this author inPubMed Google Scholar * Libak Abou View
author publications You can also search for this author inPubMed Google Scholar * Laura A. Rice View author publications You can also search for this author inPubMed Google Scholar * Kady
Dandeneau View author publications You can also search for this author inPubMed Google Scholar * Aditya Alluri View author publications You can also search for this author inPubMed Google
Scholar * Amadeo Felix Salvador View author publications You can also search for this author inPubMed Google Scholar * Ian Rice View author publications You can also search for this author
inPubMed Google Scholar CONTRIBUTIONS JP was responsible for screening the potentially eligible studies, data extraction, assessing the quality of the included studies, interpreting studies,
and writing the initial paper. LA was responsible for designing the initial review protocol, registering the protocol, conducting the search, mediating any data extraction discrepancies,
interpreting results, reviewing data extraction, and providing feedback on the paper. LR contributed to the study idea and provided feedback on the initial review protocol, results
interpretation, and paper. KD was responsible for screening the potentially eligible studies, data extraction, and writing the initial paper. AA was responsible for performing the quality
assessment for the included studies. AS was responsible for identifying key data outcomes, assisting with eligible studies, interpreting results, and providing feedback on the paper. IR
contributed to the study idea and provided feedback on the results interpretation and paper. CORRESPONDING AUTHOR Correspondence to Joseph Peters. ETHICS DECLARATIONS COMPETING INTERESTS The
authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional
affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY MATERIAL RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Peters, J., Abou, L., Rice, L.A. _et al._
The effectiveness of vigorous training on cardiorespiratory fitness in persons with spinal cord injury: a systematic review and meta-analysis. _Spinal Cord_ 59, 1035–1044 (2021).
https://doi.org/10.1038/s41393-021-00669-7 Download citation * Received: 05 September 2020 * Revised: 01 July 2021 * Accepted: 02 July 2021 * Published: 17 July 2021 * Issue Date: October
2021 * DOI: https://doi.org/10.1038/s41393-021-00669-7 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable
link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative