- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT OBJECTIVE The global obesity epidemic remains a significant threat to public health and the economy. Age-period-cohort (APC) analysis is one method to model the trajectory of
obesity. However, there is scarce published evidence of such analyses among the South East Asian population. This study aims to explore the sex and ethnic variations of BMI and waist
circumference trajectories over time among non-institutionalized Malaysian adults aged 18 to 80 years. METHODS Data from four population-based National Health and Morbidity Surveys conducted
in 1996, 2006, 2010, and 2015 were pooled. Hierarchical Age-Period-Cohort (HAPC) analysis explored the trajectories of BMI and waist circumference across the life course and birth cohorts
by sex and ethnicity. These models assumed no period effect. RESULTS Generally, BMI and waist circumference trajectories increased across age and birth cohorts. These trajectories varied by
sex and ethnicity. Females have more profound increasing BMI and waist circumference trajectories than their male counterparts as they age and as cohort recency increases. Chinese have less
profound BMI and waist circumference increases across the life course and birth cohorts than other ethnic groups. CONCLUSIONS The profound increasing cohort trajectories of obesity,
regardless of sex and ethnicity, are alarming. Future studies should focus on identifying factors associated with the less profound cohort effect among the Chinese to reduce the magnitude of
trajectories in obesity, particularly among future generations. SIMILAR CONTENT BEING VIEWED BY OTHERS SECULAR CHANGES IN MID-ADULTHOOD BODY MASS INDEX, WAIST CIRCUMFERENCE, AND LOW HDL
CHOLESTEROL BETWEEN 1990, 2003, AND 2018 IN GREAT BRITAIN Article 16 September 2020 LONGITUDINAL TRAJECTORIES OF ADIPOSITY-RELATED MEASURES FROM AGE 2–5 YEARS IN A POPULATION OF LOW-INCOME
HISPANIC CHILDREN Article Open access 04 August 2020 TRAJECTORIES AND DETERMINANTS OF WEIGHT GAIN IN TWO COHORTS OF YOUNG ADULT WOMEN BORN 16 YEARS APART Article 03 May 2021 INTRODUCTION
Obesity is a significant public health threat. It is a major risk factor for noncommunicable diseases such as cardiovascular diseases, diabetes, and certain cancers [1]. Obesity also
increases the risk of COVID-19 morbidity and mortality [2]. Globally, obesity was associated with an estimated 160 million disability-adjusted life years (DALYs) and 5.0 million premature
deaths per annum in 2019 [3]. Obesity has been increasingly prevalent in Malaysia since 1996 [4] and has become more common among younger age groups [5]. However, previous trend analyses
compared point estimates from different surveys without considering the mixed effects of age, period, and cohort (APC). Ignoring these three effects may introduce confounding. For instance,
the positive age-BMI associations reported in cross-sectional studies may be confounded by intrapersonal ageing-related changes (age effect), secular changes that affect everyone regardless
of age and birth year (period effect), or sociodemographic changes in the population due to unique differences in environmental, societal and historical exposure between people born in
different cohorts (cohort effect). More recent cohorts may have increasingly obesogenic environments due to increased consumption of energy-densel and nutrient-dilute diets. Changes in the
built environment and reduced active transportation over time may also decrease physical activity. It is thus important to account for inter-cohort (i.e., cohort effects) and intra-cohort
variations due to sex and ethnic differences when modeling BMI and waist circumference trajectories, particularly in a rapidly evolving, multi-ethnic country like Malaysia. Evidence on the
associations between sex and BMI and waist circumference trajectories has not been conclusive, with some reporting apparent sex differences across the life course [6] and birth cohorts [7,
8] and others reporting none [6, 8,9,10,11,12]. There is also a lack of published findings exploring ethnic differences in Asian populations. Therefore, this study explores the sex and
ethnic variations in trajectories of body mass index and waist circumference among non-institutionalized Malaysian adults from 1996 to 2015 using a multilevel model. This model can fully
utilize data from multiple waves of population-based cross-sectional studies to study changes in health status over time. METHODS STUDY SAMPLE A total of 94,537 nationally representative
respondents aged 18–80 years were pooled from four serial population-based cross-sectional National Health and Morbidity Surveys (NHMS). These surveys were conducted in 1996 (_n_ = 22,631),
2006 (_n_ = 34,184), 2011 (_n_ = 18,017), and 2015 (_n_ = 19,705). The NHMS ’s samples were selected via a complex, two-stage stratified, probability-proportional-to-size sampling method
[4]. The first-stage stratification was performed by states, and the second-stage was by urban/rural localities. These NHMSs covered both urban and rural areas across 13 states (Penang,
Perlis, Kedah, Perak, Selangor, Negeri Sembilan, Melaka, Johor, Kelantan, Terengganu, Pahang, Sabah, Sarawak) and 2 Federal Territories (Kuala Lumpur and Putrajaya) in Malaysia. Data
collection was conducted from March to July of each survey year. These series of NHMSs had high response rates ranging from 93.0% to 96.9%. BMI AND WAIST CIRCUMFERENCE Body weight was
measured in light indoor clothing without shoes using a Tanita digital lithium weighing scale (Tanita 318, Japan in NHMS 1996 & 2006; Tanita HD319 in NHMS 2011 & 2015) to the nearest
0.1 kg. Standing height was measured without shoes using a SECA portable body meter (SECA 206, Germany in NHMS 1996, 2006 & 2011; SECA 213 in NHMS 2015) to the nearest 0.1 cm. Both
weight and height measurements were measured twice in NHMS 2006, 2011, and 2015 and averaged values were used for analyses. Data on waist circumference was only available in three of the
NHMSs (2006, 2011, and 2015). Waist circumferences were taken midway between the inferior margin of the last rib and the crest of the ilium in a horizontal plane with the respondent’s feet
25 to 30 cm apart. Measurements were taken twice and averaged. AGE, PERIOD, AND COHORT The respondent’s age was derived by subtracting the date of birth recorded in the respondent’s
nationality identity card from the interview date. Period refers to the NHMS survey year. The year of birth (birth cohort) was derived using the formula Cohort (years) = Period - Age.
STATISTICAL ANALYSIS General and abdominal obesity were reported as weighted prevalence (%, 95% confidence interval) after adjusting for post-stratification weights. Body mass index (kg/m2)
and waist circumference (cm) were summarized as mean (95% confidence interval). All analyses were stratified by survey years. The extended hierarchical age-period-cohort (HAPC) analysis was
used to model the BMI and waist circumference trajectories. This model operationalizes period and cohort as cross-classified contextual settings in which individual characteristics such as
age reside [13]. The fixed part of the model incorporated the age and cohort effects based on the strong biological basis for an age effect and the progressively obesogenic environment over
subsequent birth cohorts. The study period effect was excluded from the fixed part of the model to avoid mathematical dependency between APC. We assumed no major contemporaneous events
occurred in the Malaysian population between 1996 and 2015. However, period effects were incorporated as random effects into the APC models to address secular changes (such as changes in
health policies and health promotion programs) for valid inferences of age and cohort trajectories. Model fit for the fixed part of the BMI and waist circumference models was assessed based
on the significance of the likelihood ratio (LR) tests when covariates (age, cohort, ethnicity, polynomial terms for age and cohort, and the respective interaction terms between ethnicity
and age, and, ethnicity and cohort) were added, one at a time, into the models. Models for waist circumference were further adjusted for weight and height. All models were stratified by sex
and fitted using the _mixed_ program in STATA version 14 (StataCorp., College Station, TX, USA) and adjusted for post-stratification sampling weights. An additional geographical identifier,
state-by-locality (i.e., state stratified by rural and urban locality), was added to all models, respectively, thereby extending the model to a four-level cross-classified model (Appendix
I). SENSITIVITY ANALYSIS Sensitivity analyses of BMI and waist circumference trajectories across ages were performed based on the alternative assumption of no linear cohort effects
(age-period model). These analyses examined the possible presence of period effect such that the obesogenic environments could have affected the entire population at the times they existed,
independent of their age and cohort. RESULTS The prevalence of both general and abdominal obesity has been increasing from 1996–2015 (Appendix II). Generally, Malaysian adults’ mean BMI
(Appendix III) and waist circumference (Appendix V) have increased from 1996–2015 in both sexes and across ethnicities, age groups, cohort groups, and localities. Results from the
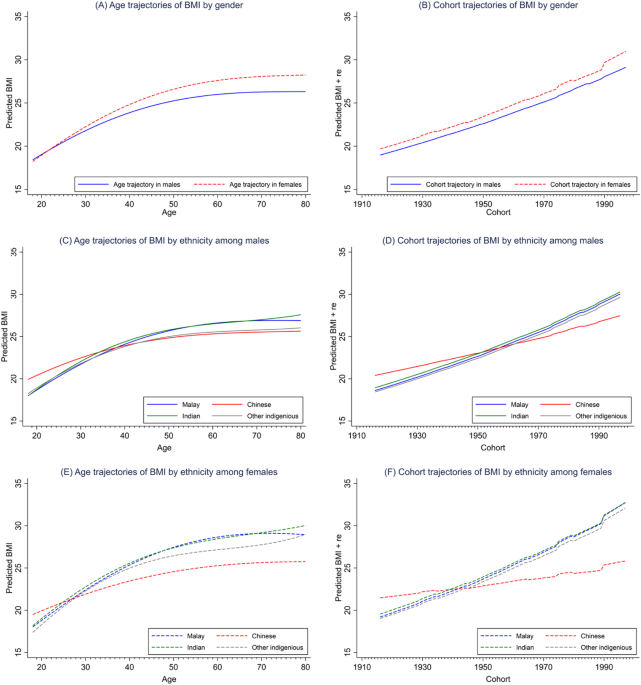
sex-stratified APC analysis revealed that the BMI of Malaysian adults (both males and females) increased steeply from age 18 to 60 and then plateaued (Fig. 1A). Waist circumference, on the
other hand, increased monotonically across the life course (Fig. 2A). Females have more profound BMI and waist circumference increases than their male counterparts across the life course
(Figs. 1A and 2A) and birth cohorts (Figs. 1B and 2B). The age and cohort trajectories of BMI and waist circumference also varied by ethnicity. The Chinese, compared to the other ethnic
groups, had the least profound increasing trajectories of BMI and waist circumference across age (Fig. 1C,E for BMI; Fig. 2C,E for waist circumference) and birth cohorts (Fig. 1D,F for BMI;
Fig. 2D,F for waist circumference) in both sexes. Such ethnic differences widened as people aged and cohort recency increased and were more pronounced among the females (Fig. 1E,F for BMI;
Fig. 2E,F for waist circumference) than their male counterparts. Sensitivity analysis revealed that alternative models assuming no cohort effect have poorer model fit than the primary models
assuming no period effect (data not shown). We observed U-shaped age trajectories with sharp drops in BMI in both sexes at about age 50. For waist circumference, the estimated waist
circumferences in males across the life course were below the cut-off point for abdominal obesity (Appendix XI). DISCUSSION In this study, the age trajectory of BMI increased steeply during
adulthood and plateaued after age 60. The increasing trajectory in early adulthood was similar to previous APC studies on obesity [12] and mean BMI [9,10,11, 14,15,16,17]. However, their
trajectories varied in the older age groups. A few studies reported a decreasing [8,9,10,11,12], whereas others reported a plateauing trend [14,15,16]. Our findings are consistent with the
existing knowledge of decreased BMI among older people due to loss of skeletal muscle mass [18], reduced appetite, and malnourishment/poor nutrient intake [19]. In contrast, monotonic
increasing age trajectories of waist circumference, which concurred with findings from a Norwegian study [20], were observed in both sexes. These increasing age trajectories can be
attributed to the age-related increase in body fat, as studies have shown that the percentage of body fat increases with age until 80 years old [21] by about 1% per decade [22]. The
monotonic increasing cohort trajectories of BMI and waist circumference observed in the present study were consistent with most studies reported elsewhere [6, 8, 9, 12, 14, 16, 23]. Cohort
effects refer to inter-generational differences in experiences, exposures, behaviors, and socioeconomic factors between individuals of different birth cohorts. These differential exposures
could have affected the habits and health behaviors in their formative years and persisted throughout their life course, thus leading to divergent health outcomes between different
generations. For instance, older cohorts born before the industrialization (the 1970s) and globalization era (1980s–1990s) may have experienced higher food scarcity, more labor-intensive
occupations, and more physically active modes of transportation [24]. Therefore, they were less likely to be exposed to obesogenic risk factors such as uptake of energy-dense food, physical
inactivity and sedentarism. In contrast, the progressively obesogenic environment may have predisposed the younger generations (particularly the Millennials or Generation Y born between
1981–1996) [8] to higher BMI and waist circumference than their counterparts in preceding cohorts. Possible reasons include increased availability, accessibility, and affordability of
energy-dense nutrient-dilute foods, shift from labor- to capital-intensive occupations, increased screen time, and reduced active commute. In the present study, a more profound increasing
age trajectory of BMI [14] was observed among women, particularly as they age. This finding concurred with those reported in a cohort study among the rural population of The Netherlands.
Evidence from a series of cross-sectional surveys in England demonstrated a more pronounced inverse association between BMI and height in older adults and women than in men, with little
change over time [25]. Therefore, this increasing sexual dimorphism in the BMI–height associations could have led to the observed sex divergence of BMI trajectories over the life course,
particularly during late adulthood. On the other hand, other studies in high-income and upper-middle-income countries did not observe differences in age trajectories by sex for mean BMI [10,
11, 15] and prevalence of obesity [12]. These findings were in keeping with those observed from the Global Health Observatory, where equitable obesity rates between men and women were
observed among most developed nations [26]. According to Grantham & Henneberg’s estrogen hypothesis, the preponderance of men’s exposure to environmental estrogen-like substances, such
as xenoestrogen in soy products and polyvinyl chloride, that are related to the superfluous nature of developed nations, could have “feminized” the men, resulting in equitable obesity rates
between men and women [27], particularly among those born in more recent cohorts. We also observed sex variations in age and cohort trajectories of BMI and waist circumference: sex
divergences in age and cohort trajectories of BMI but sex convergences in age and cohort trajectories of waist circumference. Sex dimorphism in fat distribution [28, 29] and physiological
differences [30] may explain these variations. Since women tend to accrue more weight after menopause, they may be more likely to have higher BMI than men, thus explaining the increasing sex
divergences in BMI trajectories as they age. On the contrary, men tend to store fat in visceral adipose tissue (VAT) in the deep abdominal region, compared to premenopausal women who
preferentially keep excess fat in the subcutaneous adipose tissue (SAT) depots surrounding low extremities such as hips and thighs [31], thus predisposing men to greater waist circumference
than premenopausal women. However, as age advances, SAT decreases, and VAT increases with age [22], with women having almost double increases in mean waist circumference than men [32].
Therefore, sex differences in VAT diminished as they age, resulting in the sex convergence in waist circumference over the life course. The present study revealed that the age and cohort
trajectories of BMI and waist circumference varied by ethnicity. Chinese had the least pronounced increasing trajectories of BMI. A recent APC study using four national longitudinal cohort
studies also observed persistent ethnic differences in BMI trajectories across the life course between the Black, Hispanic and White [9]. Another APC study among the New Zealand population
found ethnic differences in BMI trajectories between the Maori and non-Maori populations, with an increasing cohort trajectory only observed among the Maori [11]. For waist circumference,
despite an almost similar magnitude of trajectories between Chinese and Indians, Indians had the highest overall waist circumference. This finding concurred with that reported in a local
study where Indians have a greater likelihood of abdominal obesity than other ethnic groups across the life course [33]. Ethnic heterogeneities across the life course and birth cohorts can
be attributable to the well-established ethnic variations in total body fat (TBF) percentage [34] and SAT and VAT fat depots [35]. Besides, the unique dietary habits among ethnic groups
could also be the contributing factors. A greater preference for healthy-based over the Western-based (high in fat, sugar, and salts) food pattern among Chinese adolescents than their Malay
counterparts [36] may likely explain healthier BMI and waist circumference trajectories among the Chinese, particularly those born more recently. In contrast, higher content of
carbohydrates, saturated fatty acids, and trans fatty acids in the Indian diet may contribute to higher waist circumference across ages and cohorts [35]. Besides, genetic predisposition to
certain diseases could also contribute to ethnic differences. Several ethnic-specific single nucleotide polymorphisms (SNPs) or single gene mutations associated with obesity have been
identified [37]. In addition, racial/ethnic differentials in C-reactive protein (CRP) levels, a known risk factor of abdominal obesity [38], could be at play. Studies among the multi-ethnic
US and Canadian populations had unequivocally reported that the Chinese had the lowest mean CRP level compared to other ethnicities such as Europeans, South Asians, aborigines [39],
Caucasians, African Americans, and Hispanics [40]. These findings likely explain the more favorable obesity trajectories among the Chinese in the present study, who had the least profound
increasing BMI and waist circumference trajectories, particularly among older adults and those born in more recent cohorts. It is worth noting that due to the APC identification problem,
strong assumptions must be made to discern the APC effect. These assumptions or constraints, however, cannot be made on the basis of the data [41]. To determine either cohort or period is
more likely to be the driving temporal factor of obesity, one could compare the age trajectories produced and deduce which seems more plausible [41]. In our case, we would argue that the age
trajectories of BMI and waist circumference predicted from the primary models that assumed no period effect are theoretically plausible compared to those predicted from the alternative
models that assumed no cohort effect. The age trajectories of BMI and waist circumference predicted from the primary models concurred with those reported in previous studies, where mean BMI
[42] and waist circumference [43] increased with age until 60 to 70. Such trajectories are also consistent with ageing-related body composition changes such that body fat develops up to the
eighth decade of life and reduces afterward [44]. On the other hand, the age trajectories of BMI, predicted from the alternative model, resembled the parabolic age trajectory of obesity
among the U.S. adult population in a previous HAPC study that explicitly assumed no cohort effect [45]. As also argued by Bell and Jones [41], while BMI is known to be negatively associated
with advancing age due to sarcopenia and survival bias; however, the relatively sharp and early decline in BMI and waist circumference at age 50, as observed in the alternative model
(Appendix XI), are rather unlikely. Furthermore, the less profound age trajectories from the alternative models depict a much lower predicted mean BMI and waist circumference (in fact, well
below the BMI cut-off point of 25.0 kg/m2 for overweight and waist circumference cut-off of 90 cm for men) among the Malaysian adult population, which is, again, unlikely given the fact that
about 45% of Malaysia adults are overweight (Appendix II). CONCLUSION The present findings add knowledge to the literature on obesity prevention and reducing ethnic disparities by
identifying young adults of the most recent cohorts (the Millennials and Gen-Yers) as the high-risk sub-populations when BMI and waist circumference rapidly increased, and ethnic disparities
emerged. The increasing BMI and waist circumference trajectories with cohort recency, regardless of age and ethnic groups, are alarming and deserve great attention as these trends are
expected to increase in the foreseeable future. The sex and ethnic divergence in BMI trajectories after middle adulthood suggests that the universal BMI cut-off of 25.0 kg/m2 for overweight
and 30 kg/m2 for obesity for adults of all ages and sexes may not be appropriate, especially for females and older Malaysians. Therefore, future studies are needed to examine the
sex-stratified association between BMI and waist circumference with morbidity and mortality among middle-aged and older adults and to propose sex- and, perhaps, ethnic-specific cut-offs for
overweight and obesity for the Malaysian population. Such studies are also pertinent for a healthy ageing population. On the other hand, the less profound uptrends in BMI and waist
circumference among the Chinese late Gen-Xers and Gen-Yers warrant further investigations to identify potential protecting factors for obesity prevention among the Malaysian population. The
main strength of the present study is the use of a pseudo-longitudinal research design by pooling a series of four nationally representative cross-sectional studies and a multilevel model to
illuminate the obesity trajectories across a broad spectrum of developmental stages, encompassing late adolescence, young, middle and late adulthood and a wide span of birth cohorts. In
this era of big data analytics, this study demonstrated the optimum use of readily available nationally representative cross-sectional data in generating results comparable to those in
traditional longitudinal data [46]. This approach is particularly useful in resource-limited countries. Secondly, weight, height, and waist circumference were measured by trained nurses,
thus minimizing self-report and measurement bias. Thirdly, APC analysis was performed to account for the confounding effects of age, period, and cohort for valid inferences of age and cohort
trajectories. Nonetheless, there are also a few limitations. First, the APC analysis is descriptive; therefore, the underlying factors causing the increasing BMI and waist circumference
trajectories across the life course and cohorts remained a topic for future research. Second, due to the inherent multicollinearity between APC, we explicitly assumed no period effect
(instead of age or cohort effect). However, we contend that this assumption, in the context of the obesity epidemic in Malaysia, is physiologically plausible compared to those predicted from
the alternative models that assumed no cohort effect. Nevertheless, cautious attention is warranted for researchers that wish to adopt this model since the assumption made hereto (no period
effect) is not a one-size-fits-all approach and other factors, such as the data structure, research aims, and contextual setting that are unique to each population, must be taken into
account for HAPC model specification. Third, despite the flexibility of using a series of nationally representative, cross-sectional studies in APC studies to model health trajectories, it
must be noted that these trajectories might differ from those generated from a proper longitudinal study where individuals are followed up for a period of time. DATA AVAILABILITY Data
sources and coding were deposited in the National Institutes of Health – Data Repository System (NIH-DaRS) at https://nihdars.nih.gov.my/. However, this information is only available upon
request and is subject to approval by the Director General of Health Malaysia. CHANGE HISTORY * _ 22 DECEMBER 2023 A Correction to this paper has been published:
https://doi.org/10.1038/s41366-023-01447-6 _ REFERENCES * World Health Organisation. Global status report on noncommunicable diseases 2014. Gevena, Switzerland; 2014.
https://iris.who.int/bitstream/handle/10665/148114/9789241564854_eng.pdf?sequence=1. Accessed 27 Sep 2023. * Yang J, Hu J, Zhu C. Obesity aggravates COVID-19: a systematic review and
meta-analysis. J Med Virol. 2021;93:257–61. Article CAS PubMed Google Scholar * Chong B, Jayabaskaran J, Kong G, Chan YH, Chin YH, Goh R, et al. Trends and predictions of malnutrition
and obesity in 204 countries and territories: an analysis of the Global Burden of Disease Study 2019. EClinicalMedicine. 2023;57:101850. Article PubMed PubMed Central Google Scholar *
Institute for Public Health. National Health and Morbidity Survey. Updated August 11, 2022. https://iku.gov.my/nhms. Accessed 25 Feb 2023. * Lim KG. A review of adult obesity research in
Malaysia. Med J Malays. 2016;71:1–19. CAS Google Scholar * Barzin M, Aryannezhad S, Bagheri M, Mahdavi M, Valizadeh M, Azizi F, et al. The association of the age, period, and birth cohort
with 15-year changes in body mass index and waist circumference in adults: Tehran lipid and glucose study (TLGS). BMC Public Health. 2022;22:418. Article CAS PubMed PubMed Central Google
Scholar * Peng Y, Wang Z. Prevalence of three lifestyle factors among Australian adults from 2004 to 2018: an age-period-cohort analysis. Eur J Public Health. 2020;30:827–32. Article
PubMed Google Scholar * Robinson WR, Utz RL, Keyes KM, Martin CL, Yang Y. Birth cohort effects on abdominal obesity in the United States: the Silent Generation, Baby Boomers and Generation
X. Int J Obes. 2013;37:1129–34. Article CAS Google Scholar * Yang YC, Walsh CE, Johnson MP, Belsky DW, Reason M, Curran P, et al. Life-course trajectories of body mass index from
adolescence to old age: racial and educational disparities. Proc Natl Acad Sci USA. 2021;118:e2020167118. Article CAS PubMed PubMed Central Google Scholar * Jiang T, Gilthorpe MS,
Shiely F, Harrington JM, Perry IJ, Kelleher CC, et al. Age-period-cohort analysis for trends in body mass index in Ireland. BMC Public Health. 2013;13:889. Article PubMed PubMed Central
Google Scholar * Wilson R, Abbott JH. Age, period and cohort effects on body mass index in New Zealand, 1997–2038. Aust N Z J Public Health. 2018;42:396–402. Article PubMed Google Scholar
* Taylor AW, Shi Z, Montgomerie A, Dal Grande E, Campostrini S. The use of a chronic disease and risk factor surveillance system to determine the age, period and cohort effects on the
prevalence of obesity and diabetes in South Australian adults-2003-2013. PLoS One. 2015;10:e0125233. Article PubMed PubMed Central Google Scholar * Bell A. Life-course and cohort
trajectories of mental health in the UK, 1991-2008-a multilevel age-period-cohort analysis. Soc Sci Med. 2014;120:21–30. Article PubMed Google Scholar * Jaacks LM, Gordon-Larsen P,
Mayer-Davis EJ, Adair LS, Popkin B. Age, period and cohort effects on adult body mass index and overweight from 1991 to 2009 in China: the China Health and Nutrition Survey. Int J Epidemiol.
2013;42:828–37. Article PubMed PubMed Central Google Scholar * Nooyens ACJ, Visscher TLS, Verschuren WMM, Schuit AJ, Boshuizen HC, van Mechelen W, et al. Age, period and cohort effects
on body weight and body mass index in adults: the Doetinchem Cohort Study. Public Health Nutr. 2009;12:862–70. Article PubMed Google Scholar * Okui T. An age-period-cohort analysis of
biomarkers of lifestyle-related diseases using the National Health and Nutrition Survey in Japan, 1973-2018. Int J Environ Res Public Health. 2020;17:8159. Article CAS PubMed PubMed
Central Google Scholar * Tu Y-K, Chien K-L, Burley V, Gilthorpe MS. Unravelling the effects of age, period and cohort on metabolic syndrome components in a Taiwanese population using
partial least squares regression. BMC Med Res Methodol. 2011;11:82. Article PubMed PubMed Central Google Scholar * Nilwik R, Snijders T, Leenders M, Groen BB, van Kranenburg J, Verdijk
LB, et al. The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp Gerontol. 2013;48:492–8. Article PubMed Google Scholar *
Pilgrim AL, Robinson SM, Sayer AA, Roberts HC. An overview of appetite decline in older people. Nurs Older People. 2015;27:29–35. Article PubMed PubMed Central Google Scholar * Jacobsen
BK, Melhus M, Kvaløy K, Siri SRA, Michalsen VL, Broderstad AR. A descriptive study of ten-year longitudinal changes in weight and waist circumference in the multi-ethnic rural Northern
Norway. The SAMINOR Study, 2003–2014. PLoS One. 2020;15:e0229234. Article CAS PubMed PubMed Central Google Scholar * Ding J, Kritchevsky SB, Newman AB, Taaffe DR, Nicklas BJ, Visser M,
et al. Effects of birth cohort and age on body composition in a sample of community-based elderly. Am J Clin Nutr. 2007;85:405–10. Article CAS PubMed Google Scholar * Kuk JL, Saunders
TJ, Davidson LE, Ross R. Age-related changes in total and regional fat distribution. Ageing Res Rev. 2009;8:339–48. Article PubMed Google Scholar * Lewis CE, Jacobs DR Jr., McCreath H,
Kiefe CI, Schreiner PJ, Smith DE, et al. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Coronary Artery Risk Development in Young Adults.
Am J Epidemiol. 2000;151:1172–81. Article CAS PubMed Google Scholar * Yusoff MB, Hasan FA, Jalil SA. Globalization, economic policy, and equity: the Case of Malaysia. France: Paris;
2000. * Sperrin M, Marshall AD, Higgins V, Renehan AG, Buchan IE. Body mass index relates weight to height differently in women and older adults: serial cross-sectional surveys in England
(1992–2011). J Public Health. 2016;38:607–13. Article Google Scholar * World Health Organisation. The Global Health Observatory: mean BMI (kg/m²) (age-standardized estimate). Updated April
25, 2022. Accessed February 25, 3. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/mean-bmi-(kg-m-)-(age-standardized-estimate. * Grantham JP, Henneberg M. The estrogen
hypothesis of obesity. PloS One. 2014;9:e99776–e. Article PubMed PubMed Central Google Scholar * Chella Krishnan K, Mehrabian M, Lusis AJ. Sex differences in metabolism and
cardiometabolic disorders. Curr Opin Lipidol. 2018;29:404–10. Article CAS PubMed PubMed Central Google Scholar * Pradhan AD. Sex differences in the metabolic syndrome: implications for
cardiovascular health in women. Clin Chem. 2014;60:44–52. Article CAS PubMed Google Scholar * Jung SY, Vitolins MZ, Fenton J, Frazier-Wood AC, Hursting SD, Chang S. Risk profiles for
weight gain among postmenopausal women: a classification and regression tree analysis approach. PloS One. 2015;10:e0121430–e. Article PubMed PubMed Central Google Scholar * Lemieux S,
Prud’homme D, Bouchard C, Tremblay A, Després JP. Sex differences in the relation of visceral adipose tissue accumulation to total body fatness. Am J Clin Nutr. 1993;58:463–7. Article CAS
PubMed Google Scholar * Lahti-Koski M, Harald K, Männistö S, Laatikainen T, Jousilahti P. Fifteen-year changes in body mass index and waist circumference in Finnish adults. Eur J
Cardiovasc Prev Rehabil. 2007;14:398–404. Article PubMed Google Scholar * Rampal S, Mahadeva S, Guallar E, Bulgiba A, Mohamed R, Rahmat R, et al. Ethnic differences in the prevalence of
metabolic syndrome: results from a multi-ethnic population-based survey in Malaysia. PLoS One. 2012;7:e46365. Article CAS PubMed PubMed Central Google Scholar * Deurenberg P, Yap M, van
Staveren WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes. 1998;22:1164–71. Article CAS Google Scholar * Misra A, Khurana L.
Obesity-related noncommunicable diseases: South Asians vs White Caucasians. Int J Obes. 2011;35:167–87. Article CAS Google Scholar * Abdullah NF, Teo PS, Foo LH. Ethnic differences in the
food intake patterns and its associated factors of adolescents in Kelantan, Malaysia. Nutrients. 2016;8:551. Article PubMed PubMed Central Google Scholar * Chalazan B, Palm D, Sridhar
A, Lee C, Argos M, Daviglus M, et al. Common genetic variants associated with obesity in an African-American and Hispanic/Latino population. PLoS One. 2021;16:e0250697. Article CAS PubMed
PubMed Central Google Scholar * Shahdan SZ, Daud S,Md, Isa ML, Mohd Rasani AA, Ibrahim M, Deraman S. Abdominal obesity and high-sensitivity C-reactive protein level among Malay obese
adults in Kuantan, Malaysia. Int Med J Malays. 2018;17:79–86. Google Scholar * Anand SS, Razak F, Yi Q, Davis B, Jacobs R, Vuksan V, et al. C-reactive protein as a screening test for
cardiovascular risk in a multiethnic population. Arterioscler Thromb Vasc Biol. 2004;24:1509–15. Article CAS PubMed Google Scholar * Lakoski SG, Cushman M, Criqui M, Rundek T, Blumenthal
RS, D’Agostino RB, et al. Gender and C-reactive protein: data from the Multiethnic Study of Atherosclerosis (MESA) cohort. Am Heart J. 2006;152:593–8. Article CAS PubMed Google Scholar
* Bell A, Jones K. Don’t birth cohorts matter? A commentary and simulation exercise on Reither, Hauser, and Yang’s (2009) age–period–cohort study of obesity. Soc Sci Med. 2014;101:176–80.
Article PubMed Google Scholar * Caman OK, Calling S, Midlöv P, Sundquist J, Sundquist K, Johansson S-E. Longitudinal age-and cohort trends in body mass index in Sweden—a 24-year follow-up
study. BMC Public Health. 2013;13:893. Article PubMed PubMed Central Google Scholar * Han TS, Tajar A, Lean MEJ. Obesity and weight management in the elderly. Br Med Bull.
2011;97:169–96. Article CAS PubMed Google Scholar * Baumgartner RN. Body composition in healthy aging. Ann N Y Acad Sci. 2000;904:437–48. Article CAS PubMed Google Scholar * Reither
EN, Hauser RM, Yang Y. Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc Sci Med. 2009;69:1439–48. Article PubMed PubMed Central Google
Scholar * Kifer E. Relationships between academic achievement and personality characteristics: a quasi-longitudinal study. Am Educ Res J. 1975;12:191–210. Article Google Scholar Download
references ACKNOWLEDGEMENTS We thank the Director General of Health Malaysia for the permission to publish this paper. We would also like to thank the data collection team and central
coordinators of the Institute for Public Health for their dedicated efforts. This study was registered under the National Medical Research Registry (NMRR-18-3790-44039), and ethical approval
was granted by the Medical Research and Ethics Committee (MREC). The NHMSs were supported by the Research and Development Fund, Ministry of Health Malaysia (P42-251-170000-00500033,
NMRR-10-757-6837, NMRR-14-1064-21877). Informed written consent were obtained from all respondents prior to questionnaire administration. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Centre
for Epidemiology and Evidence-based Practice, Department of Social and Preventive Medicine, Faculty of Medicine, University of Malaya, 50603, Kuala Lumpur, Malaysia Chien Huey Teh &
Sanjay Rampal * Institute for Medical Research, National Institutes of Health, Ministry of Health Malaysia, 40170, Setia Alam, Malaysia Chien Huey Teh & Aris Tahir * Sector for
Biostatistics and Data Repository, National Institutes of Health, Ministry of Health Malaysia, 40170, Setia Alam, Malaysia Chee Cheong Kee & Omar Azahadi Authors * Chien Huey Teh View
author publications You can also search for this author inPubMed Google Scholar * Sanjay Rampal View author publications You can also search for this author inPubMed Google Scholar * Chee
Cheong Kee View author publications You can also search for this author inPubMed Google Scholar * Omar Azahadi View author publications You can also search for this author inPubMed Google
Scholar * Aris Tahir View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS TCH was responsible for writing the manuscript, cleaning and analyzing
data, interpreting results, updating reference lists and creating tables and figures. SR made a substantial contribution to the conception and design of the study and critically reviewed
the manuscript. KCC analyzed data, interpreted the results and critically reviewed the manuscript. AO contributed to data acquisition and cleaning and provided feedback on the manuscript. TA
critically reviewed the manuscript. All authors had given the final approval to publish the submitted manuscript in its present form. CORRESPONDING AUTHOR Correspondence to Sanjay Rampal.
ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional
claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY FIGURE AND TABLE LEGENDS APPENDIX I APPENDIX II APPENDIX III APPENDIX IV APPENDIX V APPENDIX
VI APPENDIX VII APPENDIX VIII APPENDIX IX APPENDIX X APPENDIX XI APPENDIX XII APPENDIX XIII RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution
4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and
the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s
Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not
permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Teh, C.H., Rampal, S., Kee, C.C. _et al._ Body mass index and waist circumference
trajectories across the life course and birth cohorts, 1996–2015 Malaysia: sex and ethnicity matter. _Int J Obes_ 47, 1302–1308 (2023). https://doi.org/10.1038/s41366-023-01391-5 Download
citation * Received: 01 March 2023 * Revised: 19 September 2023 * Accepted: 22 September 2023 * Published: 13 October 2023 * Issue Date: December 2023 * DOI:
https://doi.org/10.1038/s41366-023-01391-5 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative