- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT PURPOSE To report the visual and anatomic outcomes in eyes with macular oedema (MO) secondary to central retinal vein occlusion (CRVO) that were switched from either intravitreal
bevacizumab or ranibizumab to intravitreal aflibercept. METHODS Two-center retrospective chart review. Eyes with MO secondary to CRVO that received a minimum of three intravitreal injections
of bevacizumab or ranibizumab and were switched to intravitreal aflibercept for persistent or recurrent MO not responding to either bevacizumab and/or ranibizumab. RESULTS In all 42 eyes of
42 patients were included in the study. The median visual acuity before the switch was 20/126, 1 month after the first injection of aflibercept 20/89 (_P_=0.0191), and at the end of the
follow-up 20/100 (_P_=0.2724). The median CRT before the switch was 536 μm, 1 month after the first injection of aflibercept 293.5 μm (_P_=0.0038), and at the end of the follow-up 279 μm
(_P_=0.0013 compared to before the switch). The median number of weeks between injections before the switch was 5.6 and after the switch was 7.6 (_P_<0.0001). CONCLUSION Converting eyes
with refractory MO due to CRVO to aflibercept can result in stabilization of the vision, improved macular anatomy, and extension of the injection interval. SIMILAR CONTENT BEING VIEWED BY
OTHERS PREDICTORS OF TREATMENT OUTCOMES FOLLOWING TREAT-AND-EXTEND REGIMEN WITH AFLIBERCEPT FOR BRANCH RETINAL VEIN OCCLUSION: POST-HOC ANALYSIS OF THE PLATON TRIAL Article Open access 20
July 2023 THE RANDOMIZED ZIPANGU TRIAL OF RANIBIZUMAB AND ADJUNCT LASER FOR MACULAR EDEMA FOLLOWING BRANCH RETINAL VEIN OCCLUSION IN TREATMENT-NAÏVE PATIENTS Article Open access 12 January
2021 ANTI-VASCULAR ENDOTHELIAL GROWTH FACTOR DOSING FREQUENCY AND VISUAL OUTCOMES IN MACULAR OEDEMA FOLLOWING BRANCH RETINAL VEIN OCCLUSION Article Open access 08 May 2023 INTRODUCTION
Recent advances in the pharmacologic treatment of macular oedema (MO) from central retinal vein occlusion (CRVO) has resulted in a dramatic improvement in visual prognosis. Therapeutic
options were historically limited, as the Central Retinal Vein Occlusion Study (CVOS) failed to demonstrate the benefit of macular grid laser for MO.1 During the last 5 years, new treatments
have demonstrated efficacy and safety in several multicenter randomized controlled clinical trials. These treatments include intravitreally delivered corticosteroids, as shown in the SCORE
trial2 and the GENEVA trial,3 and intravitreal injections of agents against vascular endothelial growth factor (VEGF). Ranibizumab, a humanized, affinity-matured antibody fragment against
all isoforms of VEGF-A, has been shown in the CRUISE trial4 to provide rapid improvement in visual acuity (VA) and MO after CRVO. Studies have also demonstrated positive results with the use
of bevacizumab,5, 6 the parent molecule of ranibizumab, which has been used off-label as a cost-effective alternative to ranibizumab. Anti-VEGF agents are associated with a more favorable
safety profile compared with intravitreal steroids with respect to intraocular pressure and cataract, and thus are first-line treatment for MO due to CRVO by most retina specialists. The
eyes enrolled in the CRUISE study experienced significant improvement in their VA with an average gain of 14.9 letters at 6 months4 and 13.9 letters at 12 months.7 However, 23.1% of eyes had
persistent oedema (defined as central retinal thickness (CRT) greater than 250 _μ_m) at 6 months4 and 22.3% at 12 months.7 Bhisitkul _et al_8 reported that eyes that responded early to
treatment with ranibizumab in the CRUISE study (CRT at month 3 of 250 _μ_m or less) tended to have better visual gains over 6 and 12 months compared with eyes that exhibited a late or
incomplete response. More recently, aflibercept, a decoy fusion receptor protein comprising key domains of human VEGF receptors 1 and 2 with immunoglobulin-G Fc9 has been added to our
armamentarium for eyes with MO after CRVO. It binds all isoforms of VEGF-A, VEGF-B, and placental growth factor (PIGF), and its efficacy and safety have been established in the GALILEO10 and
COPERNICUS11 trials. Aflibercept was approved by the FDA for use in CRVO with MO in 2012. Since then, retina specialists have been offering it as a treatment option in patients with MO as
first-line treatment or in those who did not respond to treatment with ranibizumab or bevacizumab.12 The purpose of this study was to examine the visual and anatomic outcomes in eyes with
CRVO and MO that was refractory to treatment with ranibizumab or bevacizumab and were switched to aflibercept. MATERIALS AND METHODS This is a retrospective, interventional, non-comparative
case series from an academic retina practice (Massachusetts Eye and Ear Infirmary) and a private practice (Harvard Vanguard Medical Associates). All the patients received treatment at the
Retina Service of Massachusetts Eye and Ear Infirmary (DW, LHY, IKK, DGV, DDE, DH, DE, and LAK) and at the Harvard Vanguard Medical Associates (CMA). The study protocol was approved by the
Institutional Review Board of Massachusetts Eye and Ear Infirmary (IRB protocol #14-135H) and Harvard Vanguard Medical Associates (IRB protocol # 696993-1). The study adheres to the
Declarations of Helsinki and all Massachusetts and US laws. Eyes that were included in the study had prior treatment for MO secondary to CRVO with a minimum of three intravitreal injections
of either bevacizumab (1.25 mg/0.05 ml) or ranibizumab (0.5 mg/0.05 ml) and then switched to intravitreal aflibercept (2 mg/0.05 ml). The eyes were switched to aflibercept for persistent MO
or if they had recurrent oedema that initially resolved after treatment with bevacizumab and/or ranibizumab and later on did not respond to repeated injections of the same agents. The
identification of eligible eyes was done through billing records at Massachusetts Eye and Ear Infirmary and Harvard Vanguard Medical Associates with the ICD-9 code for CRVO as the search
criterion (362.35) for patients seen from September 2012 (date aflibercept received FDA approval for MO in CRVO) up to September 2014. Treatment schedules, injection intervals, and injection
techniques were at the discretion of each retina specialist. The parameters measured at each visit were non-standardized Snellen VA and CRT with optical coherence tomography (OCT). The VA
before the switch was the acuity measured the day that the patient had the first injection of aflibercept. All Snellen VA values were converted to logMAR for statistical analysis. The CRT
was measured from the thickness map of a spectral domain OCT platform. The two platforms utilized were the Cirrus OCT by Zeiss (Carl Zeiss Meditec, Dublin, CA, USA) and the Spectralis OCT by
Heidelberg (Heidelberg Engineering, Heidelberg, Germany). Patients were imaged with the same imaging modality on every follow-up visit. Regarding the injection interval data, the mean
injection interval before and after the switch was calculated for each patient and these values were used for the subsequent statistical analysis. Statistical analysis was performed with the
Prism software by GraphPad (La Jolla, CA, USA). All values were checked for normal distribution with the D’Agostino and Pearson omnibus normality test. Median values with range are reported
in data distributed in a non-Gaussian manner, and mean values with 1 standard deviation are reported in normally distributed datasets. The Wilcoxon paired signed ranked test was used for
the comparisons of injection intervals. VA data were analyzed with the Friedman test and the Dunn’s _post hoc_ test to correct for multiple comparisons. OCT data were analyzed with the
Kruskal-Wallis test and the Dunn’s _post hoc_ test to correct for multiple comparisons. Categorical data were analyzed with Fisher’s exact test. Missing values were not imputed. The level of
statistical significance was set at 0.05. RESULTS DEMOGRAPHICS AND BASELINE CHARACTERISTICS Forty-two eyes of 42 patients were included in the study. Sixteen (38%) patients were female and
26 were male (62%). The mean age of the patients was 69.8 years (+/− 13.8). Forty-one eyes had a CRVO and one eye had a hemiretinal vein occlusion. Fourteen (33%) patients had diabetes and
six (14%) of them had concurrent mild non-proliferative diabetic retinopathy. The median duration of symptoms before the patients had any treatment was 1.25 months (0.23–12). The data are
summarized in Table 1. TREATMENTS PRIOR TO THE SWITCH TO AFLIBERCEPT The median number of intravitreal injections prior to the switch to aflibercept with either bevacizumab or ranibizumab
was 7 (3–26). Sixty-six percent of the injections before the switch were bevacizumab and 34% ranibizumab. Thirty patients (71.5%) had partial response of the MO after bevacizumab and/or
ranibizumab (11 patients received only bevacizumab, 4 patients received only ranibizumab, and the remaining 15 patients received both agents, median number of injections 6.5), while 4
patients (9.5%) exhibited no response at all (2 patients received only bevacizumab, 1 patient received only ranibizumab, and 1 patient received both agents, median number of injections 4.5).
In eight patients (19%), the MO initially resolved but later recurred and did not respond to repeated injections of the same agent (five patients received only bevacizumab, one patient
received only ranibizumab, and two patients received both agents, median number of injections 11). Ten eyes (24%) had prior panretinal photocoagulation for capillary non-perfusion (3 eyes,
7%) or retinal and/or iris neovascularization (7 eyes, 17%). Three eyes (7%) had prior intravitreal triamcinolone injection(s) or intravitreal dexamethasone implant(s) (Ozurdex, Allergan,
Irvine, CA, USA). The median duration of follow-up after the first injection of bevacizumab or ranibizumab before the switch to aflibercept was 12 months (3–53.5). AFTER THE SWITCH TO
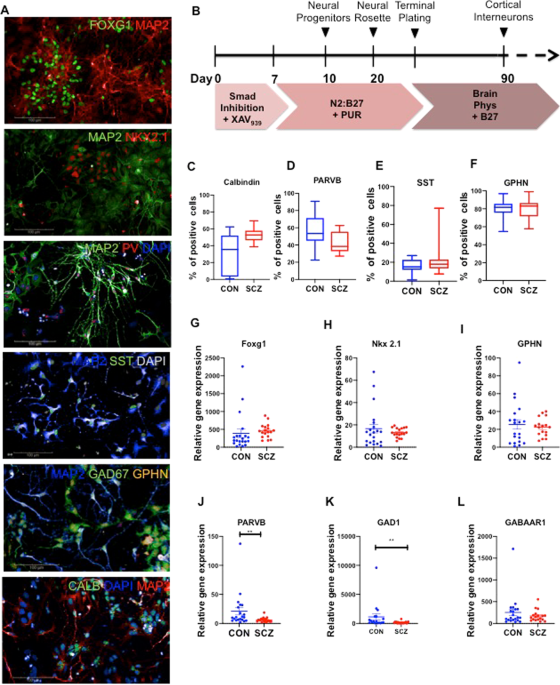
AFLIBERCEPT The mean number of aflibercept injections was 7.4 (+/− 4.7). The median follow-up after the first aflibercept injection was 14 months (3–22.2). INJECTION INTERVAL The median
interval between injections before the switch to aflibercept was 5.6 weeks (4–18) and after the switch was 7.6 weeks (4–23) (_P_<0.0001, Figure 1). No eye after the conversion to
aflibercept required more frequent injections than before the conversion. COMPLICATIONS One eye had a vitreous hemorrhage 2 days after a bevacizumab injection that resolved without
additional treatment. No patient had any other adverse event associated with the injection procedure or the treatment medication. VISUAL OUTCOMES The median VA before the switch was 20/126
(logMAR 0.8, range 0.3–1.6), 1 month after the first injection of aflibercept 20/89 (logMAR 0.65, range 0–1.6, _P_=0.0191) and at the end of the follow-up 20/100 (logMAR 0.84, range 0–1.6,
_P_=0.2724 compared with before the switch). The eyes achieved statistically significant better VA after one injection of aflibercept that was not sustained at the end of the follow-up
(Figure 2a). At 1 month after the first injection of aflibercept, 6 eyes (14%) had worse VA than before the switch, 14 eyes (33%) had the same VA, and 22 eyes (53%) experienced an
improvement. Similar rates of acuity change were seen at the final follow-up visit. Eight eyes (19%) had worse VA compared with before the switch, 16 eyes (38%) remained stable, and 18 eyes
(43%) had better VA (Figure 2b, _P_=0.66). ANATOMIC OUTCOMES The median CRT before the switch was 536 _μ_m (246–1003), 1 month after the first injection of aflibercept was 293.5 _μ_m
(185–713) (_P_=0.0038), and at the end of the follow-up was 279 _μ_m (171–927) (_P_=0.0013 compared with before the switch). The median thickness at the end of the follow-up was not
statistically significantly different than the thickness after one injection of aflibercept (_P_>0.99) (Figure 3). Nineteen eyes (45%) had persistent intraretinal and/or subretinal fluid
at the end of the follow-up. Fifteen of 23 (65%) eyes without oedema at the end of the follow-up had attenuation of the ellipsoid zone on the OCT. Seven of 23 eyes (30%) also had significant
thinning of the retina (CRT less than 200 _μ_m). DISCUSSION Aflibercept has recently been added to our treatment options for patients with MO after CRVO. Eyes enrolled in the COPERNICUS
trial13 gained 17.3 letters at 6 months after six monthly injections of aflibercept, and similar results were reported in the GALILEO study.14 These effects were maintained after additional
as needed dosing at 1 year15 and 18 months,16 respectively. Aflibercept has higher binding affinity for VEGF compared with ranibizumab or bevacizumab,9 which is an attractive feature for
eyes that do not respond to treatment with ranibizumab or bevacizumab. Bhisitkul _et al_8 demonstrated that eyes with MO and CRVO can display different patterns of anatomic response to the
treatment with intravitreal ranibizumab. They defined as early responders the patients with CRT 250 _μ_m or less at 3 months after the initiation of treatment in the CRUISE study. Late or
non-responders had reduced visual outcomes at 6 and 12 months compared with the early responders. More specifically, the late or non-responders had a gain of 11.9 letters at 6 months
compared with 15.9 letters for the early responders and a similar trend was noted at 12 months (10.1 _vs_ 15 letters). The importance of these findings is highlighted when considering that
approximately one out of four eyes with MO in CRVO will have persistent oedema at 6 and 12 months based on the CRUISE study results. In our study, the patients had on average a good anatomic
response after the first injection of aflibercept, which was maintained until the end of the follow-up (Figure 4). Despite the decrease in CRT, our eyes in this study did not experience an
improvement in VA, but rather a stabilization of their VA at the end of the follow-up. Our patients had statistically significant better VA after one injection of aflibercept, but this was
not sustained until the end of the follow-up. Plausible explanations for this phenomenon include foveal damage secondary to the long-standing oedema or retinal capillary nonperfusion in the
fovea. These could be true, as 65% of the patients without oedema had attenuation or loss of the ellipsoid zone in the oveal area at the end of the follow-up. In addition, chronic VEGF
inhibition has been suggested to lead to retinal degeneration.17 Similar results with restoration of macular anatomy and no difference in VA were seen in patients with wet AMD who were
switched from bevacizumab or ranibizumab to aflibercept for refractory oedema.18, 19, 20 Eadie _et al_12 reported their findings on six patients with MO after CRVO who had persistent oedema
after repeated injections with bevacizumab or ranibizumab. Their patients had on average more injections pre-aflibercept than in our study (17.8 _vs_ 6). Three out of the six patients had
modest visual gains and had improvement in the macular anatomy. The mean follow-up was 7 months. Our patients received on average six injections of either bevacizumab or ranibizumab before
the switch to aflibercept. There were 14 patients who received less than six total injections before the switch. Although the time for clinically significant VA gain in the CRUISE study was
5.2 months,21 we decided to include patients in this study with a minimum of three prior injections of bevacizumab or ranibizumab based on the poor visual outcome of the early non-responders
reported by Bhisitkul _et al._8 The limitations of this study include the lack of standardized VA measurement, the lack of masking for the VA and OCT measurements, and the relatively small
size of the study population. Its retrospective design naturally excludes a controlled environment for this cohort of patients as well as standardization of the treatment protocol. In
addition, the CRT measurements are subject to automated segmentation errors as they were extracted from the retinal thickness profile maps of the two OCT platforms utilized. Although the
improvement in the VA was statistically significant after one injection of aflibercept, that effect was not sustained at the end of the follow-up. A possible reason could be under-powering
as a result of small sample size, as this precludes a more detailed subgroup analysis based on initial treatment, history of panretinal photocoagulation, and/or history of prior intravitreal
steroid therapy. In summary, aflibercept can lead to improvement in macular anatomy with VA stabilization in eyes with MO after CRVO that are not responsive to ranibizumab or bevacizumab.
Further larger randomized trials are needed to determine the efficacy of aflibercept in this subset of patients with CRVO. REFERENCES * Evaluation of grid pattern photocoagulation for
macular edema in central vein occlusion. The Central Vein Occlusion Study Group M report. _Ophthalmology_ 1995; 102: 1425–1433. * Ip MS, Scott IU, VanVeldhuisen PC, Oden NL, Blodi BA, Fisher
M _et al_. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with observation to treat vision loss associated with macular edema secondary to central
retinal vein occlusion: the Standard Care _vs_ Corticosteroid for Retinal Vein Occlusion (SCORE) Study Report 5. _Arch Ophthalmol_ 2009; 127: 1101. Article Google Scholar * Haller JA,
Bandello F, Belfort R, Blumenkranz MS, Gillies M, Heier J _et al_. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion
twelve-month study results. _Ophthalmology_ 2011; 118: 2453–2460. Article Google Scholar * Brown DM, Campochiaro PA, Singh RP, Li Z, Gray S, Saroj N _et al_. Ranibizumab for macular edema
following central retinal vein occlusion: six-month primary end point results of a phase III study. _Ophthalmology_ 2010; 117: 1124–1133.e1. Article Google Scholar * Prager F, Michels S,
Kriechbaum K, Georgopoulos M, Funk M, Geitzenauer W _et al_. Intravitreal bevacizumab (Avastin) for macular oedema secondary to retinal vein occlusion: 12-month results of a prospective
clinical trial. _Br J Ophthalmol_ 2009; 93: 452–456. Article CAS Google Scholar * Zhang H, Liu Z-L, Sun P, Gu F . Intravitreal bevacizumab for treatment of macular edema secondary to
central retinal vein occlusion: eighteen-month results of a prospective trial. _J Ocul Pharmacol Ther_ 2011; 27: 615–621. Article CAS Google Scholar * Campochiaro PA, Brown DM, Awh CC,
Lee SY, Gray S, Saroj N _et al_. Sustained benefits from ranibizumab for macular edema following central retinal vein occlusion: twelve-month outcomes of a phase III study. _Ophthalmology_
2011; 118: 2041–2049. Article Google Scholar * Bhisitkul RB, Campochiaro PA, Shapiro H, Rubio RG . Predictive value in retinal vein occlusions of early _vs_ late or incomplete ranibizumab
response defined by optical coherence tomography. _Ophthalmology_ 2013; 120: 1057–1063. Article Google Scholar * Papadopoulos N, Martin J, Ruan Q, Rafique A, Rosconi MP, Shi E _et al_.
Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF Trap, ranibizumab and bevacizumab. _Angiogenesis_ 2012; 15: 171–185. Article CAS Google
Scholar * Korobelnik J-F, Holz FG, Roider J, Ogura Y, Simader C, Schmidt-Erfurth U _et al_. Intravitreal aflibercept injection for macular edema resulting from central retinal vein
occlusion: one-year results of the Phase 3 GALILEO Study. _Ophthalmology_ 2014; 121: 202–208. Article Google Scholar * Heier JS, Clark WL, Boyer DS, Brown DM, Vitti R, Berliner AJ _et al_.
Intravitreal aflibercept injection for macular edema due to central retinal vein occlusion: two-year results from the COPERNICUS study. _Ophthalmology_ 2014; 121: 1414–1420.e1. Article
Google Scholar * Eadie JA, Ip MS, Kulkarni AD . Response to aflibercept as secondary therapy in patients with persistent retinal edema due to central retinal vein occlusion initially
treated with bevacizumab or ranibizumab. _Retina (Philadelphia, Pa)_ 2014; 34: 2439–2443. Article CAS Google Scholar * Boyer D, Heier J, Brown DM, Clark WL, Vitti R, Berliner AJ _et al_.
Vascular endothelial growth factor Trap-Eye for macular edema secondary to central retinal vein occlusion: six-month results of the phase 3 COPERNICUS study. _Ophthalmology_ 2012; 119:
1024–1032. Article Google Scholar * Holz FG, Roider J, Ogura Y, Korobelnik JF, Simader C, Groetzbach G _et al_. VEGF Trap-Eye for macular oedema secondary to central retinal vein
occlusion: 6-month results of the phase III GALILEO study. _Br J Ophthalmol_ 2013; 97: 278–284. Article Google Scholar * Brown DM, Heier JS, Clark WL, Boyer DS, Vitti R, Berliner AJ _et
al_. Intravitreal aflibercept injection for macular edema secondary to central retinal vein occlusion: 1-year results from the phase 3 COPERNICUS study. _Am J Ophthalmol_ 2013; 155:
429–437.e7. Article CAS Google Scholar * Ogura Y, Roider J, Korobelnik J-F, Holz FG, Simader C, Schmidt-Erfurth U _et al_. Intravitreal aflibercept for macular edema secondary to central
retinal vein occlusion: 18-month results of the Phase 3 GALILEO Study. _Am J Ophthalmol_ 2014; 158: 1032–1038.e2. Article CAS Google Scholar * Saint-Geniez M, Maharaj AS, Walshe TE,
Tucker BA, Sekiyama E, Kurihara T _et al_. Endogenous VEGF is required for visual function: evidence for a survival role on müller cells and photoreceptors. _PLoS ONE_ 2008; 3: e3554.
Article Google Scholar * Yonekawa Y, Andreoli C, Miller JB, Loewenstein JI, Sobrin L, Eliott D _et al_. Conversion to aflibercept for chronic refractory or recurrent neovascular
age-related macular degeneration. _Am J Ophthalmol_ 2013; 156: 29–35.e2. Article CAS Google Scholar * Bakall B, Folk JC, Boldt HC, Sohn EH, Stone EM, Russell SR _et al_. Aflibercept
therapy for exudative age-related macular degeneration resistant to bevacizumab and ranibizumab. _Am J Ophthalmol_ 2013; 156: 15–22.e1. Article CAS Google Scholar * Ho VY, Yeh S, Olsen
TW, Bergstrom CS, Yan J, Cribbs BE _et al_. Short-term outcomes of aflibercept for neovascular age-related macular degeneration in eyes previously treated with other vascular endothelial
growth factor inhibitors. _Am J Ophthalmol_ 2013; 156: 23–28.e2. Article CAS Google Scholar * Thach AB, Yau L, Hoang C, Tuomi L . Time to clinically significant visual acuity gains after
ranibizumab treatment for retinal vein occlusion: BRAVO and CRUISE trials. _Ophthalmology_ 2014; 121: 1059–1066. Article Google Scholar Download references AUTHOR INFORMATION AUTHORS AND
AFFILIATIONS * Retina Service, Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston, MA, USA T D Papakostas, L Lim, T van Zyl, J B Miller, B S Modjtahedi, D Wu, L H Young, I K
Kim, D G Vavvas, D Husain, D Eliott & L A Kim * Harvard Vanguard Medical Associates, Boston, MA, USA C M Andreoli * Retina-Vitreous Associates Medical Group, Los Angeles, CA, USA D D
Esmaili Authors * T D Papakostas View author publications You can also search for this author inPubMed Google Scholar * L Lim View author publications You can also search for this author
inPubMed Google Scholar * T van Zyl View author publications You can also search for this author inPubMed Google Scholar * J B Miller View author publications You can also search for this
author inPubMed Google Scholar * B S Modjtahedi View author publications You can also search for this author inPubMed Google Scholar * C M Andreoli View author publications You can also
search for this author inPubMed Google Scholar * D Wu View author publications You can also search for this author inPubMed Google Scholar * L H Young View author publications You can also
search for this author inPubMed Google Scholar * I K Kim View author publications You can also search for this author inPubMed Google Scholar * D G Vavvas View author publications You can
also search for this author inPubMed Google Scholar * D D Esmaili View author publications You can also search for this author inPubMed Google Scholar * D Husain View author publications You
can also search for this author inPubMed Google Scholar * D Eliott View author publications You can also search for this author inPubMed Google Scholar * L A Kim View author publications
You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHORS Correspondence to D Eliott or L A Kim. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no
conflict of interest. ADDITIONAL INFORMATION This work was presented at the 2015 ARVO meeting in Denver, Colorado, USA and the 2015 ASRS meeting in Vienna, Austria RIGHTS AND PERMISSIONS
Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Papakostas, T., Lim, L., van Zyl, T. _et al._ Intravitreal aflibercept for macular oedema secondary to central retinal vein
occlusion in patients with prior treatment with bevacizumab or ranibizumab. _Eye_ 30, 79–84 (2016). https://doi.org/10.1038/eye.2015.175 Download citation * Received: 20 May 2015 * Accepted:
12 July 2015 * Published: 09 October 2015 * Issue Date: January 2016 * DOI: https://doi.org/10.1038/eye.2015.175 SHARE THIS ARTICLE Anyone you share the following link with will be able to
read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing
initiative