- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT The extent to which self-assessed work ability collected during treatment can predict return-to-work in cancer patients is unknown. In this prospective study, we consecutively
included employed cancer patients who underwent treatment with curative intent at 6 months following the first day of sick leave. Work ability data (scores 0–10), clinical and
sociodemographic data were collected at 6 months, while return-to-work was measured at 6, 12 and 18 months. Most of the 195 patients had been diagnosed with breast cancer (26%), cancer of
the female genitals (22%) or genitourological cancer (22%). Mean current work ability scores improved significantly over time from 4.6 at 6 months to 6.3 and 6.7 at 12 and 18 months,
respectively. Patients with haematological cancers and those who received chemotherapy showed the lowest work ability scores, while patients with cancer of urogenital tract or with
gastrointestinal cancer had the highest scores. Work ability at 6 months strongly predicted return-to-work at 18 months, after correction for the influence of age and treatment (hazard
ratio=1.37, CI 1.27–1.48). We conclude that self-assessed work ability is an important factor in the return-to-work process of cancer patients independent of age and clinical factors.
SIMILAR CONTENT BEING VIEWED BY OTHERS LIFE EXPECTANCY ESTIMATIONS AND DETERMINANTS OF RETURN TO WORK AMONG CANCER SURVIVORS OVER A 7-YEAR PERIOD Article Open access 18 June 2021 PREDICTORS
OF RETURN TO WORK AFTER AUTOLOGOUS STEM CELL TRANSPLANTATION IN PATIENTS WITH MULTIPLE MYELOMA Article 17 August 2021 IMPAIRMENT OF VOCATIONAL ACTIVITIES AND FINANCIAL PROBLEMS ARE FREQUENT
AMONG GERMAN BLOOD CANCER SURVIVORS Article Open access 21 December 2023 MAIN Cancer diagnoses in individuals who are still at the working age are becoming more common, with almost half of
the adult cancer survivors being younger than 65 years (Short et al, 2005). With the sustained improvement in treatment and prognosis of many forms of cancer, an increasing number of
survivors of cancer return-to-work following treatment or continue to work during therapy (Hoffman, 2005). Returning to work is important for both cancer patients themselves and the society.
Patients often regard returning to work as a symbol of complete recovery (Spelten et al, 2002) and regaining a normal life (Kennedy et al, 2007), while from the viewpoint of the society, it
is an economic and social imperative to encourage patients to return-to-work whenever possible. Despite its importance, the impact of cancer and its treatment on work (dis)continuation or
resumption has not been studied frequently (Steiner et al, 2004). However, a number of studies have documented the impact of cancer on employment and they reported that approximately 60% of
the cancer patients return to work within 1–2 years (Spelten et al, 2002; Maunsell et al, 2004; Bradley et al, 2005; Nieuwenhuijsen et al, 2006). The return-to-work in cancer survivors
seems, therefore, to be problematic in some patients but certainly not in all. Hence, it is important to identify those patients with a higher risk of lasting absence from work and to
provide them with the appropriate support and counselling in returning to work. To examine the factors that would influence this return-to-work process, we previously studied a model based
on the assumption that cancer-related symptoms would mediate return-to-work (Spelten et al, 2003). However, results showed that diagnosis and treatment were much stronger predictors of
return-to-work than cancer-related symptoms such as fatigue, depressive symptoms or cognitive problems. In addition, recent empirical studies have indicated the importance of patients’
expectations of recovery as good predictors of return-to-work and rehabilitation independent of diagnosis and treatment (Ekbladh et al, 2004; Verbeek, 2006). Studies in other disorders have
also shown that a patient's own assessment of work ability (Reiso et al, 2003), expectation of job success (Ekbladh et al, 2004) and work recovery expectations (Hogg-Johnson and Cole,
2003; Nieuwenhuijsen et al, 2006; Turner et al, 2006) do predict return-to-work. A theory that could explain these mechanisms is the well-known Leventhal's ‘model of illness
representations’, which states that people's cognitive representations of illness exert an important influence on their strategies for coping, which in turn influence illness outcomes
(Leventhal et al, 1984). It has been shown in other diseases such as multiple sclerosis, rheumatoid arthritis and kidney disease (Vaughan et al, 2003; Carlisle et al, 2005; Fowler and Baas,
2006) that, on the basis of this model, the functional outcome might be worse or better, irrespective of the objective medical seriousness of the illness. This strongly suggests that the
ideas a cancer patient has about the disabilities that might result from the diagnosis and treatment will encourage or hinder his or her return-to-work. With these new insights, our data
were reanalysed with the focus on the patients’ assessments of work ability as predictor of return-to-work. In our earlier publication on return-to-work of cancer survivors, we did not use
information on the self-assessed ability to work because at the time it was outside the focus of our study (Spelten et al, 2003). The aim of the current study is therefore (1) to examine any
change in work ability scores in cancer patients over time and to study differences among patient groups and (2) to assess the extent to which self-assessed work ability predicts
return-to-work among cancer survivors independent of diagnosis, treatment and cancer-related symptoms. MATERIALS AND METHODS PATIENTS Eligible patients had to be between 18 and 58 years to
have a primary diagnosis of cancer, to be in paid employment at the time of diagnosis, to be within 4–6 months following their first day of sick leave, and to have had treatment with
curative intent. They were consecutively recruited in three hospitals in The Netherlands where the attending physician obtained the patients’ informed consent. The study has been carried out
with the approval of the hospitals’ medical ethical committees. Questionnaires were distributed three times to the patients, at entry into the cohort and 6 and 12 months later, to obtain
information on their return-to-work, diagnosis, treatment, work ability and cancer-related symptoms. Details of the design and material of this prospective cohort study have been reported
earlier (Spelten et al, 2003). The data were collected between 1998 and 2002. For the current study, data on return-to-work and work ability were collected at study entry and 6 and 12 months
later. Data on work load, work stress, cancer-related factors and sociodemographic factors had been collected at baseline. All questionnaires were mailed to the patients’ homes. MEASURES
RETURN-TO-WORK Data on return-to-work were measured on the basis of two measures: time to return-to-work after sick leave and rate of return-to-work at a specific point in time. All patients
in The Netherlands typically have access to sick leave. Time to return-to-work at 18 months after the first day of sick leave was calculated as the number of days between the first date of
sick leave and the first day the patient returned to work. Any kind of work resumption qualified as a return-to-work, irrespective of the number of hours that the patients worked prior to
their diagnosis. In addition, patients were asked to indicate if they were still on sick leave (yes/no) at 6, 12 and 18 months following their first day of sick leave. WORK ABILITY, WORK
LOAD AND WORK STRESS Current work ability was measured with the first three items from the Work Ability Index (WAI) (Ilmarinen and Tuomi, 1993, p 142; Tuomi et al, 1998), which is a reliable
and valid measure of work ability (Ilmarinen and Tuomi, 1993, p 142; de Zwart et al, 2002). First, current work ability was assessed by asking the patients to estimate their current work
ability compared with their lifetime best (0=cannot work at all to 10=best ever). In addition, we asked the cancer patients to rate both their current physical and mental work ability in
relation to job demands (0=very low to 5=very high). Physical workload was measured with a seven-item scale and work stress with an 11-item scale from the Dutch Questionnaire on Experience
and Judgement of Work (VBBA) (van Veldhoven et al, 2002). Patients were asked to assess their levels of workload and work stress for the work situation prior to diagnosis. The scores range
from 0 to 100, with higher scores indicating a higher level of physical work and more work stress, respectively. CANCER-RELATED AND SOCIODEMOGRAPHIC FACTORS Information about diagnosis and
treatment was reported by the patients. Twenty-two different diagnoses were then grouped according to cancer site into (1) breast cancer, (2) haematological oncology, (3) gastrointestinal
cancer, (4) cancer of the female genitals, (5) genitourological cancer and (6) other types of cancer. Treatments were classified into three categories: (1) surgery, (2) radiotherapy or
radiotherapy plus surgery and (3) chemotherapy or chemotherapy plus radiotherapy and/or surgery. We measured cancer-related complaints with validated questionnaires and converted all scores
to a scale ranging from 0 to 100, with higher scores indicating more complaints (Spelten et al, 2003). The following complaints were measured: physical cancer-related complaints (de Haes et
al, 1990), general fatigue (Smets et al, 1995), sleep quality (Buysse et al, 1989), depressive symptoms (Radloff, 1977), psychological distress (de Haes et al, 1990), cognitive dysfunction
(Broadbent et al, 1982) and global quality of life (de Haes et al, 1990). Further information was enquired concerning marital status (single, married, cohabitating or other), having children
in the household, age, gender, education (lower education, high school, college/university) and work hours per week before the diagnosis of cancer. STATISTICAL ANALYSIS The work ability
scores measured at 6, 12 and 18 months after the first day of sick leave were analysed with the mixed-model procedure based on repeated measurements to examine any change in work ability
scores over time. We also used the mixed-model procedure to analyse any differences over time in work ability scores between several patient groups: age groups (18–27, 28–37, 38–47 and 48–58
years), education groups, men and women, diagnosis groups and treatment groups. Time, group and time*group interaction effects were considered fixed effects and an autoregressive covariance
structure was selected because of correlated work ability scores over time. In case of a statistically significant main effect, _post hoc_ analyses were performed between time points and
between groups with pairwise comparisons based on the use of the mean difference of the estimated marginal means. To examine whether self-assessed work ability can predict return-to-work in
cancer patients a year later, taking the impact of clinical-, work- and subject-related factors into account, we used a two-step procedure. First, univariate analyses using Kaplan–Meier
analyses were performed for the relationship between time taken to return-to-work (in days) at 18 months and each of the predictive factors measured at baseline (on average 6 months after
the first day of sick leave): current work ability, mental work ability, physical work ability, physical work load, work stress, physical complaints, fatigue, sleep impairments, depression,
psychological distress, cognitive dysfunction, age, gender, education and the clinical factors (diagnosis and treatment type). Next, we analysed the impact of work ability in addition to
personal and clinical factors in a multivariate Cox regression analysis. We entered all variables for which the log-rank test returned a _P_-value⩽0.10 into a Cox regression analysis with
forward selection of variables. With this method, the best predictors of future return-to-work are selected (Altman, 1991). Because it was possible for patients to return to work before our
first measurement at 6 months, we repeated both analyses with the exclusion of patients who had returned before 6 months. Since this is a survival analysis, hazard ratios (HRs) usually
indicate the risk of dying, while in our case the event is returning to work. Therefore, an HR higher than one indicates the higher ‘risk’ of return-to-work. Alpha was set at 0.05 unless
stated otherwise and all tests were two-sided. Analyses were conducted with SPSS 13. RESULTS The first questionnaire was completed by 235 of the 264 eligible patients (a response of 89%),
while a total of 29 patients declined participation in this study. The second questionnaire at 6 months follow-up was completed by 221 of the 235 participating patients (a follow-up response
of 94%). At 12 months of follow-up, the questionnaire was returned by 195 patients (an 83% follow-up response and 74% of the initially eligible patients), while 25 patients refused to
return the questionnaire, 13 patients had died and 2 questionnaires got lost in the mail. Table 1 shows sociodemographic and cancer-related characteristics at 6 months after the first day of
sick leave. Half of the patients had either breast cancer (26%) or cancer of the female genitals (22%), while another 22% of the patients had been diagnosed with genitourological cancer.
Before diagnosis and treatment, patients worked an average of 34 h per week, and 6 months after the diagnosis, 46 patients (24%) had already returned to work or had continued working. Data
on work hours per week, children, fatigue, depression, sleep problems, physical complaints, cognitive dysfunction, psychological distress, work load and work stress have been reported
previously (Spelten et al, 2003). Table 2 depicts the mean values of current work ability at 6, 12 and 18 months after the first day of sick leave; the values improved significantly over
time (_P_<0.001) from 4.6 at 6 months to 6.3 at 12 months and to 6.7 at 18 months. _Post hoc_ analyses of work ability scores showed that all three time points were significantly
different from each other (_P_<0.001 to _P_=0.035). All age groups improved over time (_P_<0.001) with the 28- to 37-year-old patients increasing most from 4.8 to 7.5. No differences
in work ability scores were, however, found between age groups (_P_=0.12). Work ability scores of both men and women improved over time (_P_<0.001), but women improved more (_P_=0.002).
Male patients showed higher work ability scores at 6 months (5.8 _vs_ 3.8, _P_<0.0001), but not at 12 months (6.8 _vs_ 6.0, _P_=0.053) or at 18 months (6.9 _vs_ 6.7, _P_=0.52). Higher
educated patients seemed to have higher work ability scores, but the differences were not statistically significant (_P_=0.13). With regard to diagnosis, we found significant differences
between the different diagnosis groups (_P_<0.001). The haematological oncology patients showed the significantly (_P_<0.001) lowest scores of 3.3, 4.5 and 5.0 at 6, 12 and 18 months,
respectively. The patients with genitourological cancer had the highest scores of 6.9 and 7.8 at 6 and 12 months (_P_<0.001), and the patients with gastrointestinal cancer scored the
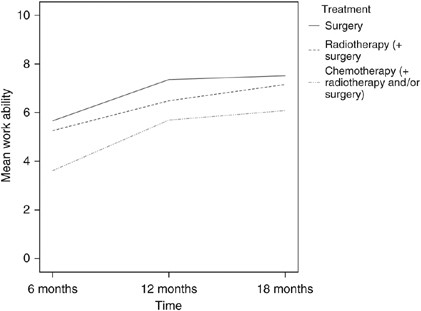
highest work ability of 7.6 at 18 months (_P_<0.001). Patients with cancer of the female genitals and breast cancer patients improved most over time (_P_=0.01). Figure 1 shows the work
ability scores for the three treatment combinations: (1) surgery; (2) chemotherapy or chemotherapy plus radiotherapy and/or surgery; and (3) radiotherapy or radiotherapy plus surgery, over
time. Analyses revealed that scores improved over time for all three groups and that the group of patients that received chemotherapy or chemotherapy plus radiotherapy and/or surgery
consistently showed lower work ability scores than the group that received surgery or radiotherapy (plus surgery) (_P_<0.001). Improvement was not statistically different in the three
groups (_P_=0.45). At 6 months after diagnosis, 24% of patients had returned to work, at 12 months 50%, and at 18 months 64% had returned. Results of univariate analyses using the
Kaplan–Meier analyses showed that the time taken to return-to-work measured at 18 months was related to the following factors measured at 6 months: current work ability, mental work ability,
physical work ability, quality of life, fatigue, physical complaints, cognitive functioning, age, physical work load, work stress, gender, diagnosis and treatment (at the _P_⩽0.10 level).
Sleep impairments, depression, psychological distress and education did not significantly predict return-to-work. Results of the analysis without the 46 patients who had already returned to
work at 6 months showed the same factors except for gender, which did not significantly predict return-to-work. The factors that were predictive for return-to-work at 18 months were entered
in the Cox regression with a forward selection to identify the strongest predictors of return-to-work. Results in Table 3 show that in the final model, age, current work ability and
treatment are still significant. Current work ability, physical work ability and mental work ability were highly correlated and, therefore, only current work ability remained in the model.
Likewise, treatment and diagnosis were highly correlated, and only treatment was selected for the final model. Patients treated with surgery alone had the highest chance of returning to work
quickly. Those who were treated with radiotherapy or radiotherapy plus surgery had an HR of 0.63 (95% CI: 0.39–1.0), corrected for age and work ability, of returning to work and were thus
1.6 times more likely to stay off work than patients with surgery alone. Patients treated with chemotherapy, either alone or in combination with other treatment modalities, had an HR of 0.41
(95% CI: 0.25–0.69) and their risk of staying off work was therefore 2.4 times higher than patients treated with surgery alone, corrected for age and work ability. For current work ability
itself, every 1 point increase on the 11-point scale meant a 1.37 higher chance of returning to work earlier, after correction for the influence of age and treatment. Figure 2 shows the plot
of the work ability scores in relation to return-to-work after adjustment for age and treatment. The plot shows that of the patients with the lowest work ability scores (0–5) at 6 months
after the first day of sick leave, the majority (55–80%) did not return to work in the first year after diagnosis. Patients with very high work ability scores (8, 9, 10) did usually return
to work within half a year, while virtually all of these high-scoring patients were back at work after the first year. Results of the analysis without the 46 patients who had already
returned to work at 6 months showed that in this model the strongest predictors of return-to-work were not only work ability (HR=1.23; CI, 1.12–1.36), treatment (chemotherapy HR=0.33; CI,
0.18–0.60; radiotherapy HR=0.52; CI, 0.29–0.95) and age (HR=0.67; CI, 0.53–0.86) but also mental work ability (HR=1.41; CI, 1.05–1.89) and cognitive dysfunction (HR=1.03; CI, 1.01–1.05).
DISCUSSION The aim of our study was to examine changes in work ability scores in cancer patients over time and to study differences between patient groups and, furthermore, to assess the
extent to which self-assessed work ability predicts return-to-work among cancer survivors independent of diagnosis, treatment and cancer-related symptoms. We found that the cancer patients’
work ability scores at 6, 12 and 18 months after the first day of sick leave improved significantly over time. Men scored higher on work ability than women but no differences were found
between age or education groups. Furthermore, the haematological oncology patients and the patients who received chemotherapy or chemotherapy plus radiotherapy and/or surgery consistently
showed lower work ability scores. Finally, self-assessed work ability 6 months after the first day of sick leave proved to be a strong predictor of later return-to-work in cancer survivors
independent of age and therapy. This is the first longitudinal study in which the impact of work ability on return-to-work has been established in a systematic way. The cohort has been
followed for a considerable amount of time, the number of patients lost to follow up was relatively small and all factors have been measured with validated instruments. In our study, the
mean current work ability scores at 6, 12 and 18 months after the first day of sick leave were 4.6, 6.3 and 6.7, respectively. Although we found a significant improvement of current work
ability, these scores are lower than the average current work ability score of 7.9 found by Pohjonen (2001) in a sample of female home care workers in the age group 40–44 years old with an
average of two diagnosed benign diseases. It might be possible that work ability scores in cancer patients will improve still further 2 years after the diagnosis or that their work ability
scores might deteriorate because cancer has a larger impact on work ability than other diseases. Research on the effect of cancer diagnosis and treatment on work ability is scarce; however,
studies have shown recently that most patients are employed but that both physical and mental work ability can deteriorate owing to cancer (Gudbergsson et al, 2006; Steinbach et al, 2006;
Kennedy et al, 2007; Taskila et al, 2007). Patients in the recent study of Kennedy et al (2007), who were 1–10 years after diagnosis, reported that they had difficulties in coping and
concentrating, and they worried about their reduced capability. In the comparative study of Gudbergsson et al (2006), it was found that cancer patients 2–6 years after diagnosis, who had
returned to work after curative treatment, reported significantly poorer physical and mental work capacity compared to employed matched controls from the general population. Most survivors
of glioblastoma in the study of Steinbach et al (2006) also thought that their work ability was impaired. According to Taskila et al (2007), 26% of cancer survivors reported that their
physical work ability had deteriorated and 19% that their mental work ability had deteriorated owing to cancer diagnosis and treatment. However, the work ability as measured with the WAI of
these cancer survivors did not differ from that of a group of healthy referent persons. This is probably also caused by the fact that all their survivors with breast cancer, lymphoma and
prostate cancer had already returned to work and that they were long-term survivors who had been diagnosed with cancer 2–6 years before the time of the questionnaire. This could also explain
the differences in mean work ability scores between their study and the patients in our study. For men in their study, the work ability scores were 8.0 (for prostate cancer) to 8.9 (for
testicular cancer) compared to 6.9 for the men in our study 18 months after the first day of sick leave. Our female patients scored 6.7 at the end of follow-up compared to 8.2 (for breast
cancer) and 8.5 (for lymphoma) in the Finnish study by Taskila et al (2007). Our study also showed that men initially showed higher scores of work ability, while women improved faster and no
differences were found after 1 year. It might be possible that women, who were mainly diagnosed with breast cancer, received more chemotherapy, which would have prolonged the treatment
period. Another explanation might be that women could have more household activities than men and that they take these into account when judging their work ability. Our study indicated work
ability as an independent predictor for return-to-work, while quality of life was only found to be predictive of time until return-to-work in the univariate analyses. The same result was
found earlier for Norwegian patients with back disorders who had been certified as sick (Reiso et al, 2003). The authors of that study suggested that work ability questions may be related
more to function in a setting of sickness certification than a global quality of life question and therefore be more predictive. In an earlier analysis (Spelten et al, 2003), we found that
fatigue at 6 months predicted a longer sick leave with an HR of 0.71, adjusted for diagnosis, treatment, age and gender. Our present study indicated that fatigue was only a predictive factor
of return-to-work in the univariate analyses but not in the multivariate analyses, which included work ability. Because work ability and fatigue were correlated, only work ability remained
in the model as the better predictor of return-to-work. Other studies have also found that fatigue influenced conditions of employment and productiveness (Hofman et al, 2007). Results of the
univariate analyses without the 46 patients who had already returned to work at 6 months showed that gender was not a significant factor anymore. This might be caused by the fact that most
of these returned patients were men (65%) and were diagnosed with testes or prostate cancer (48%). In the model of best predictors of return-to-work without those patients who had returned
early, the factors mental work ability and cognitive dysfunction were included. This could imply that for patients who do not return early, the mental and psychological factors become more
dominant in relation to return-to-work. Leventhal's ‘model of illness representations’ states that people's cognitive representations of illness play an important role in
influencing their strategies for coping, which in turn influence illness outcomes (Leventhal et al, 1984). On the basis of this model, the functional outcome might be worse or better,
irrespective of the objective medical seriousness of the illness. Our results are congruent with this model. Irrespective of age, diagnosis, treatment, quality of life, fatigue, and physical
or psychological complaints, self-assessed work ability strongly predicted future return-to-work. This indicates that the ideas a cancer patient has about his or her work disabilities that
result from the diagnosis and treatment of cancer are a reflection of the true work capabilities. Therefore, the self-reported work ability could be important in encouraging or hindering his
or her return-to-work. Employment outcomes can be improved with innovations in treatment and with clinical and supportive services aimed at better management of symptoms, rehabilitation and
accommodation of disabilities (Steiner et al, 2004). A recent study of Bouknight et al (2006) showed that a high percentage of employed breast cancer patients returned to work after
treatment and that workplace accommodations played an important role in their return. Therefore, interventions should be developed to enable cancer survivors to return to work or to succeed
in other appropriate employment, because no such interventions aimed at work do exist at the present. These interventions should aim especially at patients who indicate that their work
ability is diminished, at older patients and at those treated with chemotherapy, since they are at the greatest risk of prolonged work absence. Clinicians could play an important role in
detecting those patients at risk because our study has shown that the indication of patients with possible return-to-work problems can be assessed very early in the treatment process when
they have diminished self-reported work ability. Physicians could help patients in the return-to-work process and therefore help in improving their quality of life by asking patients if they
have returned to work or are experiencing problems in the return-to-work process. If so, referral to occupational specialists could be considered. In conclusion, the work ability of cancer
patients who work at the time of their diagnosis is severely impaired in the first months after the first day of sick leave, but it does improve significantly in the months afterwards.
Self-assessed work ability 6 months after the first day of sick leave proved to be a strong predictor of later return-to-work in cancer survivors independent of age and therapy. CHANGE
HISTORY * _ 16 NOVEMBER 2011 This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication _ REFERENCES * Altman DG (1991)
_Practical Statistics for Medical Research_. Chapman and Hall: London Google Scholar * Bouknight RR, Bradley CJ, Luo Z (2006) Correlates of return to work for breast cancer survivors. _J
Clin Oncol_ 24 (3): 345–353 Article Google Scholar * Bradley CJ, Neumark D, Luo Z, Bednarek H, Schenk M (2005) Employment outcomes of men treated for prostate cancer. _J Natl Cancer Inst_
97: 958–965 Article Google Scholar * Broadbent DE, Cooper PF, Fitzgerald P, Parkes KR (1982) The Cognitive Failures Questionnaire (CFQ) and its correlates. _Br J Clin Psychol_ 21: 1–16
Article Google Scholar * Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index (PSQI): a new instrument for psychiatric practice and research.
_Psychiatric Res_ 28: 193–213 Article CAS Google Scholar * Carlisle AC, John AM, Fife-Schaw C, Lloyd M (2005) The self-regulatory model in women with rheumatoid arthritis: relationships
between illness representations, coping strategies, and illness outcome. _Br J Health Psychol_ 10: 571–587 Article Google Scholar * Ekbladh E, Haglund L, Thorell LH (2004) The worker role
interview – preliminary data on the predictive validity of return to work of clients after an insurance medicine investigation. _J Occup Rehabil_ 14: 131–141 Article Google Scholar *
Fowler C, Baas LS (2006) Illness representations in patients with chronic kidney disease on maintenance hemodialysis. _Nephrol Nurs J_ 33: 173–174, 179–186 PubMed Google Scholar *
Gudbergsson SB, Fossa SD, Borgeraas E, Dahl AA (2006) A comparative study of living conditions in cancer patients who have returned to work after curative treatment. _Support Care Cancer_
14: 1020–1029 Article Google Scholar * de Haes JCJM, van Knippenberg FCE, Neyt JP (1990) Measuring psychological and physical distress in cancer patients: structure and application of the
RSCL. _Br J Cancer_ 62: 1034–1038 Article CAS Google Scholar * Hoffman B (2005) Cancer survivors at work: a generation of progress. _CA Cancer J Clin_ 55: 271–280 Article Google Scholar
* Hofman M, Ryan JL, Figueroa-Moseley CD, Jean-Pierre P, Morrow GR (2007) Cancer-related fatigue: the scale of the problem. _Oncologist_ 12 (Suppl 1): 4–10 Article Google Scholar *
Hogg-Johnson S, Cole DC (2003) Early prognostic factors for duration on temporary total benefits in the first year among workers with compensated occupational soft tissue injuries. _Occup
Environ Med_ 60: 244–253 Article CAS Google Scholar * Ilmarinen J, Tuomi K (1993) _Work Ability Index for Aging Workers_. Finnish Institute of Occupational Health: Helsinki Google Scholar
* Kennedy F, Haslam C, Munir F, Pryce J (2007) Returning to work following cancer: a qualitative exploratory study into the experience of returning to work following cancer. _Eur J Cancer
Care_ 16: 17–25 Article CAS Google Scholar * Leventhal H, Nerenz DR, Steele DJ (1984) Illness representations and coping with health threats. In _Handbook of Psychology and Health_, Baum
A, Taylor SE, Singer JE (eds), Vol. 4, pp 219–252. Erlbaum: London Google Scholar * Maunsell E, Drolet M, Brisson J, Brisson C, Mâsse B, Deschênes L (2004) Work situation after breast
cancer: results from a population-based study. _J Natl Cancer Inst_ 96: 1813–1822 Article Google Scholar * Nieuwenhuijsen K, Bos-Ransdorp B, Uitterhoeve LL, Sprangers MA, Verbeek JH (2006)
Enhanced provider communication and patient education regarding return to work in cancer survivors following curative treatment: a pilot study. _J Occup Rehabil_ 16: 647–657 Article Google
Scholar * Pohjonen T (2001) Perceived work ability of home care workers in relation to individual and work-related factors in different age groups. _Occup Med (London)_ 51: 209–217 Article
CAS Google Scholar * Radloff LS (1977) The CES-D Scale, a self-report depression scale for research in the general population. _Appl Psych Meas_ 3: 385–401 Article Google Scholar *
Reiso H, Nygard JF, Jorgensen GS, Holanger R, Soldal D, Bruusgaard D (2003) Back to work: predictors of return to work among patients with back disorders certified as sick: a two-year
follow-up study. _Spine_ 28: 1468–1473 PubMed Google Scholar * Short P, Vasey JJ, Tuncelli K (2005) Employment pathways in a large cohort of adult cancer survivors. _Cancer_ 103: 1292–1301
Article Google Scholar * Smets E, Garssen G, Bonke B, de Haes JCJM (1995) The Multidimensional Fatigue Inventory, psychometric qualities of an instrument to assess fatigue. _J
Psychometric Res_ 39: 315–325 Article CAS Google Scholar * Spelten ER, Sprangers MAG, Verbeek JH (2002) Factors reported to influence the return to work of cancer survivors: a literature
review. _Psychooncoloy_ 11: 124–131 Article Google Scholar * Spelten ER, Verbeek JH, Uitterhoeve AL, Ansink AC, van der Lelie J, de Reijke TM, Kammeijer M, de Haes JC, Sprangers MA (2003)
Cancer, fatigue and the return of patients to work-a prospective cohort study. _Eur J Cancer_ 39: 1562–1567 Article CAS Google Scholar * Steinbach JP, Blaicher HP, Herrlinger U, Wick W,
Nagele T, Meyermann R, Tatagiba M, Bamberg M, Dichgans J, Karnath HO, Weller M (2006) Surviving glioblastoma for more than 5 years: the patient's perspective. _Neurology_ 66: 239–242
Article CAS Google Scholar * Steiner JF, Cavender TA, Main DS, Bradley CJ (2004) Assessing the impact of cancer on work outcomes. _Cancer_ 101: 1703–1711 Article Google Scholar *
Taskila T, Martikainen R, Hietanen P, Lindbohm ML (2007) Comparative study of work ability between cancer survivors and their referents. _Eur J Cancer_ 43: 914–920 Article Google Scholar *
Tuomi K, Ilmarinen J, Jahkola A (1998) _Work Ability Index_, 2nd revised edn. Finnish Institute of Occupational Health: Helsinki Google Scholar * Turner JA, Franklin G, Fulton-Kehoe D,
Sheppard L, Wickizer TM, Wu R, Gluck JV, Egan K (2006) Worker recovery expectations and fear-avoidance predict work disability in a population-based workers’ compensation back pain sample.
_Spine_ 31: 682–689 Article Google Scholar * Vaughan R, Morrison L, Miller E (2003) The illness representations of multiple sclerosis and their relations to outcome. _Br J Health Psychol_
8: 287–301 Article Google Scholar * Verbeek JH (2006) How can doctors help their patients to return to work? _PLoS Med_ 3: e88 Article Google Scholar * van Veldhoven M, de Jonge J,
Broersen S, Kompier M, Meijman T (2002) Specific relationships between psychosocial job conditions and job-related stress: a three-level analytic approach. _Work Stress_ 16: 207–228 Article
Google Scholar * de Zwart BC, Frings-Dresen MH, van Duivenbooden JC (2002) Test-retest reliability of the Work Ability Index questionnaire. _Occup Med (London)_ 52: 177–181 Article CAS
Google Scholar Download references ACKNOWLEDGEMENTS This study was supported by a grant from the Dutch Cancer Society (AMC 97-1385). We thank Dr J van der Lelie for his contribution to this
study. We are grateful to all of the patients for their participation in this study. AUTHOR INFORMATION Author notes * A C Ansink Present address: Current address: Erasmus MC, Daniel den
Hoed Oncology Center, Rotterdam, The Netherlands., AUTHORS AND AFFILIATIONS * Coronel Institute for Occupational Heath, Academic Medical Center, University of Amsterdam, Amsterdam, The
Netherlands A G E M de Boer, J H A M Verbeek, E R Spelten, M Kammeijer & F J H van Dijk * Cochrane Collaboration Occupational Health Field, Kuopio, Finland J H A M Verbeek * NPVO,
Amsterdam, The Netherlands E R Spelten * Department of Radiotherapy, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands A L J Uitterhoeve * Department of
Gynaecology and Obstetrics, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands A C Ansink * Department of Urology, Academic Medical Center, University of Amsterdam,
Amsterdam, The Netherlands T M de Reijke * Jan van Breemen Institute, Amsterdam, The Netherlands M Kammeijer * Department of Medical Psychology, Academic Medical Center, University of
Amsterdam, Amsterdam, The Netherlands M A G Sprangers Authors * A G E M de Boer View author publications You can also search for this author inPubMed Google Scholar * J H A M Verbeek View
author publications You can also search for this author inPubMed Google Scholar * E R Spelten View author publications You can also search for this author inPubMed Google Scholar * A L J
Uitterhoeve View author publications You can also search for this author inPubMed Google Scholar * A C Ansink View author publications You can also search for this author inPubMed Google
Scholar * T M de Reijke View author publications You can also search for this author inPubMed Google Scholar * M Kammeijer View author publications You can also search for this author
inPubMed Google Scholar * M A G Sprangers View author publications You can also search for this author inPubMed Google Scholar * F J H van Dijk View author publications You can also search
for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to A G E M de Boer. RIGHTS AND PERMISSIONS From twelve months after its original publication, this work is
licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE de Boer, A., Verbeek, J., Spelten, E. _et al._ Work ability and return-to-work in cancer patients. _Br J Cancer_ 98, 1342–1347
(2008). https://doi.org/10.1038/sj.bjc.6604302 Download citation * Received: 06 November 2007 * Revised: 07 February 2008 * Accepted: 11 February 2008 * Published: 18 March 2008 * Issue
Date: 22 April 2008 * DOI: https://doi.org/10.1038/sj.bjc.6604302 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * employment * work ability *
return-to-work * longitudinal studies * prospective studies