- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
For SeaJaye Sillasen, 75, of Lakewood, Colorado, her multiple sclerosis (MS) — a progressive disease of the central nervous system — has advanced slowly since her diagnosis more than 50
years ago. “I’m very fortunate,” she says. When she and her partner of 35 years, Robin Paquet, 67, first met, Sillasen “didn’t have any noticeable symptoms,” says Paquet. Leg weakness, the
most troubling symptom, didn’t appear until 2009. That’s when Sillasen began using a walking stick, then a walker, and, for the past six years, a wheelchair at home and a scooter to maneuver
in public. Sillasen and Paquet, former owners of residential facilities for developmentally disabled adults, are now retired. For Jeanne Caputo of Los Angeles, the disease progressed
rapidly. Caputo, a screenwriter, was diagnosed in 1997 on her 37th birthday. Within three years, she was a quadriplegic and eventually moved to a skilled nursing facility, where her husband
Jon Strum, 70, visited her every day. Caputo died in 2020. “She had a particularly vicious case of MS; it is not the norm,” says Strum, who quit his job as a marketing executive to care for
his wife and now hosts a weekly podcast called Real Talk MS. Strum and Paquet refer to themselves as care partners, a term many in the MS community prefer to caregiver. It recognizes that
both people contribute to and benefit from the relationship, says clinical psychologist Rosalind Kalb, the lead senior programs consultant for Can Do MS, a national nonprofit that provides
education, resources, and support. Nearly 1 million people in the United States may be living with MS, researchers estimate, with women outnumbering men by as much as 3 to 1. If you are
helping with the care of someone with MS, here are six steps experts recommend you take. LEARN ABOUT MS Learning about the disease can help you navigate its unpredictable nature, communicate
with the medical team and prevent mistakes, as Strum and Caputo learned early on. “We decided she could relax in a nice, warm bath,” he says. He returned a few minutes later to lift his
wife out of the tub. “To say she was limp would not fully describe it.” Neither realized that heat worsens symptoms for many with MS. Jon Strum and Jeanne Caputo COURTESY STRUM MS occurs
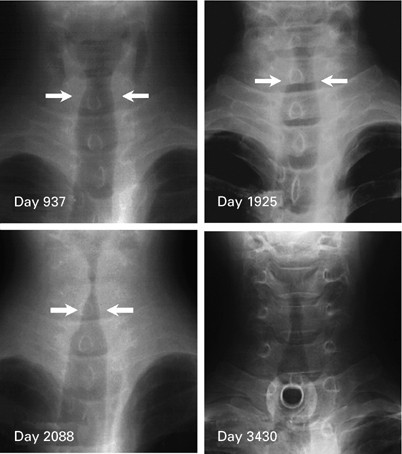
when the body’s immune system mistakenly attacks myelin, the protective coating on nerve fibers that carry communication signals between nerve cells. A doctor can see the damage to myelin on
an MRI (magnetic resonance imaging) of the brain and spinal cord as scar-like lesions. MS also damages the nerve fibers and nerve cells. Symptoms usually begin between the ages of 20 and
40, and often include: * Vision problems * Muscle weakness and stiffness, often in the arms and legs * Tingling, numbness or pain in the arms, legs, trunk or face * Clumsiness * Bladder
control problems * Dizziness MS may also cause: * Mental or physical fatigue * Mood changes such as depression or difficulty controlling emotions * Cognitive changes or memory difficulties A
small number of people with MS will have mild symptoms throughout their lives, but most will experience worsening symptoms over time. Often, symptoms come and go; approximately 85 percent
of people with MS are initially diagnosed with what’s called relapsing-remitting disease. While there is no cure, treatments are available. To shorten a relapse, neurologists usually
recommend a short course of high-dose corticosteroids that lessen inflammation. To reduce the number of relapses and delay disease progression, neurologists may suggest ongoing treatment
with one of more than 20 available medications, either oral, injected or infused.