- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
Support for the statewide broadcast of the state of Ohio comes from medical mutual, providing more than one point four million Ohioans peace of mind with a selection of health insurance
plans online at Medda Mutual dot slash Ohio by the law offices of PorterWright Morris and Arthur LLP. Now, with eight locations across the country, PorterWright is a legal partner with a new
perspective to the business community, Morad PorterWright Dotcom and from the Ohio Education Association, representing 100 24000 members who work to inspire their students to think
creatively and experience the joy of learning online at O H E A dot org. The twenty twenty two US Senate race is on in Ohio, with the first candidate officially launching a campaign. The
state launches a promotion to bring business to Ohio, but some people are pushing back. And a sudden announcement aimed at the largest part of the state budget may have saved the rainy day
fund all this weekend, the state of Ohio. Welcome to the state of Ohio, I'm Karen Kasler Ohio Republicans have their first official candidate for the twenty twenty two US Senate race.
Josh Mandel has run for U.S. Senate twice before and it filed paperwork suggesting he planned to run for Congress in twenty twenty. But the former state treasurer says it's former
President Donald Trump's impeachment that put him in the race. That incumbent Senator Rob Portman announced on January twenty fourth that he would not enter. It seems likely Mandel will
face a primary against Jane Timkin, whose resignation as chair of the Ohio Republican Party included references to the America first agenda and similar pro Trump language, as Mandela's
announcement did. But he is confident he is the Trump candidate. You know, my phone has been ringing off the hook with conservative activists and Trump activists encouraging me to run. And
I'm confident with that support we're going to win this primary and then we're going to go beat Amy Akin in the general election. Akton, the popular former Ohio Department of
Health director who quit after protests and death threats related to the state's covid shutdown policies, has left her job at a Columbus nonprofit and is considering a run as a
Democrat. Mandele blasts often for those policies, which potentially puts him in an awkward position with her Republican former boss, Gov. Mike DeWine, who likely will be on that same twenty
twenty two Republican ticket running for reelection. Mandel promotes his ties to Trump, but he actually backed Florida Senator Marco Rubio early in the 2016 campaign, as most Ohio elected
officials were supporting former Gov. John Kasich and lost a Democratic U.S. Senator, Sherrod Brown, twenty twelve and wanted a rematch in twenty eighteen, but abruptly quit that race,
citing the serious illness of his wife. Since then, Mandel got divorced, has erased most of his tweets and recovered from covid late last year. Gov. Mike DeWine sparked curiosity and
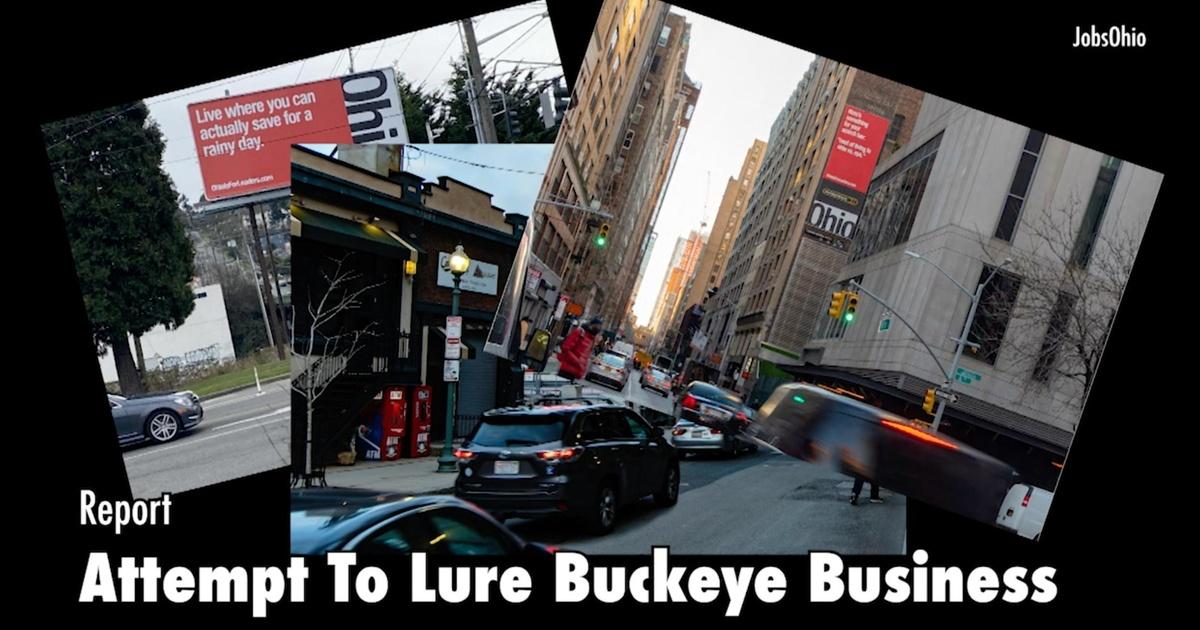
controversy with his plan in the budget to spend 50 million dollars on a promotional campaign to bring former Ohioans back or to keep people from leaving the state. It turns out Ohio's
private nonprofit Jobs Development Corporation is doing something similar with businesses. But a statehouse correspondent, Jo Ingles, reports part of the overall strategy is raising eyebrows
and questions. In rainy Seattle, there's a billboard that reads live where you can actually save for a rainy day. Outside Fenway Park in Boston, a billboard reads zero percent state
corporate income tax. That's the ticket. And high over Times Square in New York City. There are signs that say things like your buildings are taller, our taxes are smaller. Those edgy
ads are just part of an overall strategy by jobs Ohio to lure business owners away from high tech cities to Ohio, where there's no corporate business tax and where housing is more
affordable. The Ohio is for leaders campaign also includes TV and digital ads, which were produced in Brooklyn and personalized emails to business leaders such as Tom Goodman, the president,
CEO and owner of Goodman Media International, based in New York City. He's received emails, phone calls and voicemails to try to get him to relocate his business to central Ohio, where
he attended college at Ohio Wesleyan University in the 70s. So I was kind of fascinated by it, thought it was interesting. And I was very respectful and declined about, I guess, six months
ago when I first heard from him. But then I started getting voice mails and emails again was like, wow, they won't stop. So, you know, I think it's know, fascinating more than
anything else to me. But Jobs Ohio is hoping lower taxes and affordability will prompt business leaders to give Ohio a second look. We wanted to be a little bold and take take some risks.
We've been Midwest modest, if you will, up to this point in time and trying to get the Ohio story out there and running. Scott says now is the perfect time to get out there because the
pandemic has many business owners thinking about moving away from those high tax cities. The media talks constantly about migration from the coasts, both in people, capital and financial
investments. And we see where they're going. And we want to make sure Ohio's in the consideration said we want to make sure that we're not forgotten about. We don't want
to look back in a couple of years and look to see where businesses moved. It would be irresponsible if we weren't making sure that Ohio is top of mind. Pandemic related shutdowns have
led many businesses to discover they don't need an actual brick and mortar office as much as once thought. Goodman says he and his employees have been working remotely since March 12th.
We do not envision being back in the office any time soon and maybe never in terms of full time every day, and we haven't seen our work drop off one bit. But Goodman says that
doesn't mean he's looking to relocate and he says taxes have no effect on where he chooses to live and work. The high visibility campaign started in September and was fully rolled
out this month, and it's provided fodder for hundreds of comments on social media from current and former Ohioans who say it's not taxes turning them off, but the state's
political climate. Many lambasted lawmakers for policies that they say hurt working Ohioans, women and minorities. But Governor Mike DeWine rejected that in a widely reported comment in a
recent press conference. Ohio is a welcoming place. I don't care who you are. We want you to come to Ohio. You know, it's a progressive state. Ohio is one of six states with no
corporate income tax, which was replaced in 2005 with the commercial activity tax. The liberal leaning think tank Policy Matters Ohio suggests seventy eight point five percent corporate
income tax were put in place. That could generate nearly 500 million dollars a year and state revenue. But Republicans have long rejected new taxes, and they say they're looking for
more ways to cut them. Jo Ingles Statehouse News Bureau this week brought the end of a late night curfew instituted in November as hospitalization stayed below twenty five hundred for more
than a week. It's quite a drop from the record on December 15th, when there were five thousand three hundred eight people in Ohio hospitals with covid. At that point, one in three
patients were covered positive. Now it's one in ten. But the Ohio Department of Health is warning the state to brace for a huge increase in the death toll. It says it will soon add in
as many as 4000 deaths from November and December, which will increase the total by a third. The state has blamed the discrepancy between its numbers and those reported by the CDC on, quote,
process issues affecting the reconciliation and reporting of these deaths that it says began in October. The announcement came after the Department of Health testified on its budget before
the House Finance Committee. The pandemic could have blown a hole in the new two year state budget just with increased caseloads in Medicaid. But there's a two point four billion dollar
infusion of federal money from the continuation of a temporary pandemic related increase in federal Medicaid assistance program funding that saved the state from having to use most of the
rainy day fund to fill that hole. But there is a condition on this money and it's not permanent. And Medicaid caseloads are expected to hit a peak of just under three point four million
a year from now and not forecast to go down to pre pandemic levels in this two year budget cycle. This week, I talked to Ohio Medicaid director Maureen Corcoran at an appropriate social
distance with a pain of Plexiglas between us. We have had already more than three hundred and thirty thousand Ohioans who have needed Medicaid assistance, some for the first time in their
lives. You know what the economy's looking like? People lose their health care. So exactly as you say, the federal government, as part of one of their early Korona relief bills, put in
an additional kind of enhanced Medicaid match. And exactly as you suggest that the deal, though, is that they'll give the extra money. But what they want in return or what the bill
calls for in return is that we not terminate anyone from Medicaid during the pandemic. And of course, the logic is that even if they don't return their paperwork or something like that,
they probably still are a person who needs the health care coverage. That's kind of the logic. So once the pandemic is over, we'll have to return to kind of a normal way of doing
business. And we know that that money, that federal money is going to stop at the end of the quarter when the pandemic. And so it is kind of an abrupt, you know, stopping of the money. And
then we'll still need some time to come back to normal because caseloads do lag behind unemployment numbers. And so you are, as you say in your testimony, going to need a little bit of
time to recover from that. But the federal funding could stop with just a 60 day notice. So this could be very abrupt. Yeah. So they the the as you know, the pandemic, the federal authority
has to be reauthorized every 90 days. So during the beginning days of the pandemic, sometimes they would renew it with only a day or two. Now, the good news in the guidance that we've
just gotten recently from the secretary is that they expect that there it's very likely, as they say, that the pandemic will be continued through the end of the year, this calendar
year. And that they will give us at least 60 days notice so that that gives us much more. I mean, they still must reauthorise by 90 day increments. That's what the the pandemic, the
statute governing the pandemic requires. But that'll give us the ability to begin to look out toward the end of the year and do some planning. And even with that, you know, there could
be a decision made to continue it even beyond that. But one of the things that the new administration was hearing quite a bit is we need some kind of planning runway. And so this really does
help a great deal. Fewer people have been going into nursing homes during this pandemic. Is that saving the state money? And also the death toll has hit nursing homes very hard. What has
been the effect of Medicaid and its relationship to nursing homes with both of those things? Well, you know you know, and I think, Kiran, we talked once before about we have nursing home
options and we have community options, waivers, passport, individual options, things like that, so that individuals have some choice about whether they want to stay at home, can stay at home
or not. And for many years, states across the country have been trying to increase the community services so that there can be a true choice between those. So, you know, you're
you're exactly right. The the pandemic is is really brought to light, especially some of the concerns about nursing homes, for example. Most often they are multiple occupancy rooms,
very common. Well, that becomes kind of the biggest, most immediate problem. We confronted with the virus because almost everybody is in a multi occupancy room. So the governor that combined
with a variety of other things that are important in terms of helping that industry kind of make the transition, get to the other side of this, continue to provide good quality care. The
governor has put forth a five or six point plan that encompasses the Department of Medicaid, Department of Health and the Department of Aging and really tries to bring together some
incentives, some encouragement, some training, some regulatory changes, all in an effort to support the industry, but also to really provide some some incentive for us to really take another
step towards better care in nursing homes. For instance, you've got 50 million dollars in this budget that would allow you to buy 11000 unused beds to cut down on those shared rooms.
There's also a provision that would allow for the Department of Health to have more authority to shut down nursing homes deemed unsafe. That's something the Department of Health
already has the authority to do through the court system. But these things you feel is the goal to not just protect people in nursing homes, but also potentially to save the state some money
over time? Well, honestly, the objective is not been to save the state money. It's really been to try to bring together carrots and sticks and regulations and training and quality
focus. This one of these this idea about buying back or bed reduction is voluntary. And as you say, with 50 million dollars in the budget intended to provide that funding for nursing home
operators who may want to transition their their facility to be a little bit smaller and so will through this program, which will still need to do the design work with the stakeholders and
with the industry. But then people can give up the beds and have some additional money to make single occupancy rooms, do some renovation around their spaces, things like that, which, you
know, everybody's always working to to find the next thing that consumers want anyway. So it's all consistent with that. In your testimony, the House Finance Committee, you talked
about multisystem kids as well, which you say are the most expensive people in the Medicaid system because they have lots of needs and quite often they need to be sent out of state to get
the care that they need. The high rise program was announced last fall. How does this program prevent custody relinquishment where parents had to give up custody of their kids to try to deal
with this? And what does the budget do for kids, these these very kids that need a lot of help? Yeah, yeah. In the last budget, the General Assembly put in about 12 million dollars that
we're the across all of the child serving agencies. We work together as a team with the governor's Office of Children's Initiatives and Family and Children First Council. And
so we administer the money in such a way that any of the family and children first councils from around the state, if they find if they have a situation like. You're describing they can
and often it will be a child who can be can be very expensive. They can apply to the state for assistance. Now, we've we've even had more than one hundred families who just needed
that. The county or the local community just needed additional technical assistance from the state. So sometimes it wasn't even the money, it was just some additional technical
assistance. But the tragedy of this is exactly as you suggest, families who, through absolutely no fault of their own, may have a child who just has extraordinary needs. And the cost of that
care is very, very expensive, even for, you know, middle income and upper middle income families and individuals. So the point here is to really try to put some additional community
services in place, intensive community services that can work with families and in the home and prevent or support the family to not then have to give up custody of their child. So it's
how to how to help the family learn to work with the child to provide additional kind of in the home treatment for the child, the young person, depending on how old they are, in the hopes
that then they won't have to give over custody of their child to the state, which I can't imagine anything more heartbreaking. You talked earlier about some of the conditions on
this federal money. One of those things is that you can't institute work requirements, which had been a topic of discussion for quite a while. There had been no implementation of that.
But there is a voluntary work program that you're starting to work on here. Do you know of any bills in the legislature, though, that would run afoul of that, that would try to force
Medicaid into some sort of work requirements program? I'm thinking specifically of one Senate bill that would eliminate Medicaid's ability to rely on self self testing,
essentially, and would require a medical certificate for intensive physical illness or serious mental illness. And then it also appears that it could affect pregnant women and would put work
requirements on them. Are you concerned about those kind of things? Well, there is. You know, Medicaid is extraordinarily complicated. So we are we're going through the bill and and
are looking at it really with two eyes. One is what they're there may be some provisions in there that under no circumstance will we be allowed to implement. And then, of course, you
know, with the pandemic, there may be things that are allowed, but not now. So we're trying to go through it with a thoughtful eye about that. You know, we'll we'll look
forward to discussion with the sponsor. You know, I think sometimes it helps when we can look at what it what it would require for a county. The county jobs and family service organizations
are the ones who administer all this kind of testing and gathering documents, not only for Medicaid, but for SNAP and TANF. So they've got an enormous amount of work right now. And so
you kind of have to weigh the cost and the benefit of it. But we'll work through that with the sponsor, I'm sure. On the note of mothers and babies, infant mortality, maternal
health, over half the birth is in Ohio, are covered by Medicaid. So I want to ask you, what about postpartum coverage for new moms? Will all women have access to this? Or is this just
something that women who have been diagnosed with a substance abuse order have access to? Yeah, that's a great question. We know that particularly after a mom delivers their baby, that
her health and the health of the baby is better if we can be sure that she has continuing health care coverage. And so we are looking at what's called postpartum up to 12 months
postpartum coverage. It would be limited to those women who have a substance use disorder. And we've we had done some work on it, got a little bit hung up with the pandemic, but
we're continuing to move forward with that. The state has picked a single pharmacy benefits manager, PBM, as it's known, that was from the last budget. But you've actually
picked this person or this entity gain? Well, not a multibillion dollar corporation like CVS Caremark, which the state was working with. How will a single PBM actually save the state money?
Yeah, that's a great question. So, for example, the you know, the Department of Medicaid back in twenty eighteen did a study and then it was further verified, very similar numbers
verified by the auditor that the Department of Medicaid was paying managed care plans, pharmacy related payments that equaled about two hundred and twenty four million dollars. Yea, that
really could not be explained. Now, some of that would be a legitimate payment, but it clearly was far in excess of what would be considered a reasonable payment for their their services. So
with this new PBM that we've chosen, the contract that we have with them is for up to seven years and it averages about 20 million dollars per year. So two hundred and twenty four
versus 20. Now, you will have to hire some other people, though, potentially to provide all the services that some of these other PBM will provide. Yes, we we are hiring some additional
pharmacists, for example, who would work for us and work with the program. So we've done a complete fiscal analysis to look at what what what's the full cost of all these changes,
including whether it's state administrative cost or whatever it is. And we've found that from the combination of our entire procurement, about thirty, thirty two billion dollars,
that it'll be cost neutral. Same cost is what we're doing today, plus or minus maybe a half a percent. So, you know, we've been prudent about what's in these are fees.
We're choosing excellent partners. And at the same time, we're able to take some of the money that was really administrative payments and be able to put it into more services.
Well, this is pandemic's over and you're still at these higher caseloads. Are you concerned about how your department is going to handle all the things that you have to do to make
sure that people are still qualified? I mean, without losing people falling off because you just don't have the number of people you're going to need to process three million
people every time, three million caseloads every time. I mean, isn't it an overload potentially for your agency? Yes, it's and remember that, as I mentioned, it's the county
departments who process all, again, not only Medicaid, but SNAP and TANF where combined eligibility state. And so that is one of the topics that we've talked about with Medicaid
directors around the country and with our federal partners, because as we come out of this, it is going to be important that we create a smooth pathway because we still have people will
still have new people coming in. And so you don't you know, you don't want to be in a position where, you know, you're kind of managing the old, but you also have to be able
to take care of the new. So that is one of the things that we're really very actively talking with CMS about is how what kind of leniency or what kind of changes could be made in terms
of how kind of normal things happen to assist us to get back to a little more stable operational level. And finally, a year ago, you wrote a memo that blasted the Kasich administration for
leaving a lot of unfinished business. For instance, you talked about the move, the move to of people, to providers of addiction and mental health services treatment, low income people in the
Medicaid managed care system, you called it. The implementation was the worst I've seen in my professional career of more than 30 years. You had other words of you weren't happy
with what you had inherited. And of course, the case of administration differs with your perspective. Of course, they they pushed back on that. But do you feel your agency was ready with all
of that and then the pandemic right on top of all that? That's a great question. We from the moment that the governor took office, he was very clear with myself and with Laurie Crist,
Director Chris. And you know how important the behavioral health work is to the governor as well as to, you know, lots and lots of the people on the Medicaid program. So we hit the ground
running. We worked very hard for more than a year with the stakeholders. We we continue with the stakeholder work group that includes consumers of services as well as professionals and have
really it's not perfect yet. I don't think anybody in the behavioral health system would tell you it's perfect. But the progress has been enormous. We've been able to
stabilize the system a little bit and thank God given going into the pandemic. So, you know, we've we've managed actually extraordinarily well to keep going on the things that are
important. And that is it for this week. Please check out the Ohio Public Radio and Television State House News Bureaus website at statenews.org. And you can follow us and the show on
Facebook and Twitter. And please join us again next time for the state of Ohio. Support for the statewide broadcast of the state of Ohio comes from medical mutual, providing more than one
point four million Ohioans peace of mind with a selection of health insurance plans online at Medd Mutual dotcom slash Ohio by the law offices of PorterWright Morris and Arthur LLP. Now with
eight locations across the country, PorterWright is a legal partner with a new perspective to the business community. More at PorterWright Dotcom and from the Ohio Education Association,
representing 100 24000 members who work to inspire their students to think creatively and experience the joy of learning online at O H E A dot org.