- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
Tuberculosis is now a significant public health issue, and nurses need to know its signs and symptoms and which groups at increased risk of infection ABSTRACT Tuberculosis has re-emerged as
a significant public health issue in the UK. Early diagnosis is essential to improving patients’ outcomes and reducing the time they are infectious. Nurses in all areas of healthcare are
well positioned to facilitate earlier diagnosis of the disease. This article looks at barriers and possible solutions. CITATION: MURPHY S (2015) How nurses can support early diagnosis of
tuberculosis. _Nursing Times_; 111: 13, 12-14. AUTHOR: Sarah Murphy is tuberculosis nurse specialist at London TB Extended Contact Tracing Team, Public Health England. * This article has
been double-blind peer reviewed * Scroll down to read the article or download a print-friendly PDF here INTRODUCTION Having declined throughout most of the last century, tuberculosis (TB)
has re-emerged as a significant public health problem. The UK is experiencing some of the highest rates of TB infection in western Europe, prompting Public Health England to identify it as a
key priority (PHE, 2014a). The World Health Organization (2014a) has identified TB, a serious but treatable disease caused by _Mycobacterium tuberculosis_, as one of the world’s most
significant infectious causes of illness and death. Although TB is primarily a disease of the lungs (pulmonary TB), it can infect other parts of the body (extrapulmonary TB), including the
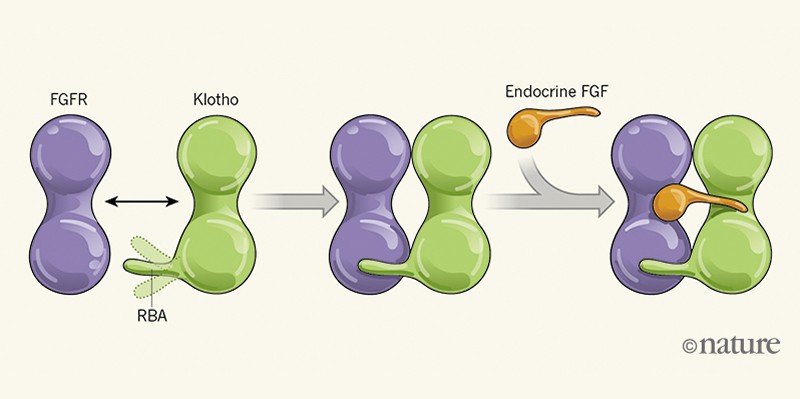
lymph nodes, bones and central nervous system. The infection is spread through airborne transmission and only cases in the lungs, larynx or tonsils are considered infectious. HOW TB IS
TRANSMITTED When a person with infectious TB coughs or sneezes, bacteria are expelled into the air in respiratory droplets (Fig 1, attached). These can be inhaled by others and drawn into
the alveoli of their lungs, which initiates an immune system response. If the immune system kills the bacteria, they are cleared from the body but, if not, the body becomes infected with TB.
The body’s immune response is often able to contain and inactivate TB bacteria; the person is then said to have latent TB infection (LTBI). This is asymptomatic and not infectious, so it
cannot be passed on; however, there is a 10% lifetime chance that the bacteria can reactivate and cause TB disease. Activated LTBI is most likely to occur in the first two years of
infection, or in patients who are immunocompromised by other illness or old age (Williams, 2008). If the immune system is unable to kill or contain the bacteria, they can continue to grow
and multiply, causing sickness. This is called active TB disease. SIGNS AND SYMPTOMS OF TB Symptoms of active TB disease can develop weeks or even years after infection. They vary depending
on the site of the disease - for example, prolonged cough is associated with pulmonary TB, while localised swelling is associated with lymph node TB. Box 1 lists the most common signs and
symptoms; TB should be considered if any of these have been present for more than three weeks. BOX 1. SIGNS AND SYMPTOMS OF TB * Cough * Haemoptysis * Fatigue * Fever * Night sweats * Loss
of appetite * Unintentional weight loss DIAGNOSIS AND TREATMENT Investigations used to diagnose active pulmonary TB include chest X-ray, multiple sputum samples checking for acid-fast
bacilli, and Mycobacterium culture. Sputum samples are crucial to confirm diagnosis, assess infectiousness, determine drug sensitivities and inform public health action. Sputum samples can
be produced spontaneously or by induced sputum or gastric washing (National Institute for Health and Care Excellence, 2011). In extrapulmonary TB, biopsy and needle aspiration should be
considered and a chest X-ray should be performed to exclude respiratory involvement. However, if there are clinical symptoms consistent with TB, NICE (2011) recommends treatment is started
without waiting for culture results. TB is treatable and, after two weeks of medication, most patients are no longer infectious. However, where there is drug resistance, this can take longer
and require closer monitoring of sputum samples. A TB case manager - often a nurse specialist - supports the patient to adhere to a combination of medications for a minimum of six months.
ROLE OF NURSES IN CONTROLLING TB To control the spread of TB and ultimately eliminate the infection, control programmes must be focused on: * Prompt identification of new cases; * Timely
start and support for patients to complete treatment; * Prevention of new cases. Early diagnosis is pivotal, as it not only improves patient outcomes but also reduces the possibility of
onward transmission to others who are in close and regular contact with the patient. In the UK, between 2004 and 2013, more than a quarter of patients with pulmonary TB started treatment
more than four months after the onset of symptoms, and the proportion of cases with this delay has risen slightly in the past three years (PHE, 2014b). Drug resistance is a growing problem
and is linked to failures to diagnose, prevent and adequately treat TB. A new five-year TB strategy for England aims to address this and sets a target of 80% of people with pulmonary TB
starting treatment within three months, and 100% within six months of the onset of symptoms (PHE and NHS England, 2015). Nurses are essential to TB control and elimination. While some
specialist nurses care solely for TB patients, the vast majority work in other areas and encounter patients for a wide variety of reasons. These nurses are in an ideal position to identify
possible cases of undiagnosed TB and refer these patients to TB services to achieve earlier diagnosis. It is therefore important that all nurses are aware of the signs and symptoms of TB
(Box 1), especially those who work with high-risk populations, such as migrants, substance users, homeless people and patients who are HIV positive. TB DIAGNOSIS PATHWAYS The WHO (2011)
describes two pathways to TB diagnosis: the “patient-initiated” pathway; and the “screening” pathway. The patient-initiated pathway is often called passive case finding as it depends on
patients presenting themselves to healthcare services, whereas the screening pathway is called active case finding as it involves targeting and screening high-risk populations. The
patient-initiated pathway includes five steps, each of which can present a potential barrier to early diagnosis: * Recognition of symptoms by the sick individual or carer; * Accessing an
appropriate healthcare provider; * Identification of patients with suspected TB by healthcare workers; * Accessing correct diagnostic tests; * Referral to specialist services. Understanding
and addressing these barriers could increase early diagnosis. WHY DO PATIENTS PRESENT LATE? TB does not respect socioeconomic or geographical boundaries, and anyone with significant exposure
can be infected; however, within many developed countries, TB is concentrated in “hard to find” and “hard to reach” populations (van Hest et al, 2014). The vast majority of cases of TB are
concentrated in large urban areas, with London accounting for the highest proportion of cases in the UK (PHE, 2014b). Zenner et al (2013) said risk factors for TB were often linked with:
migration from an area with a high incidence of TB; lifestyle (such as homelessness or substance misuse); or imprisonment. Access to healthcare can be problematic for these vulnerable
groups, who are typically less engaged with services than the general population (Zenner et al, 2013). Even when a service is deemed universal and there are no direct costs to patients,
other important barriers can hinder access (WHO, 2014b). These include marginalisation, language, stigma and discrimination. Factors such as unemployment, lack of knowledge of health
services, homelessness and concerns regarding immigration status have been associated with delayed access to care in developed countries (French et al, 2009). The WHO (2014) suggests that
improving access to high-quality TB services to ensure optimal TB management includes: outreach, community screening clinics and providing patient-centred, culturally sensitive and holistic
care. NICE (2012) has issued guidance for accessing hard-to-reach populations and national charity TB Alert coordinates community awareness activities that engage and use peer educators.
DELAYS BEFORE DIAGNOSIS Even once a patient has presented to healthcare services, TB might not be diagnosed promptly. Patients can present at a variety of settings, most commonly primary
care or accident and emergency departments. Delays can occur if there are low levels of TB awareness and clinical suspicion among health professionals, delays in collecting appropriate
diagnostic samples and complicated referral procedures to specialist services. Public Health England (2013) found that patients with extra-pulmonary disease were more likely to experience a
longer delay than pulmonary cases. This could be due to the slower onset and wider range of symptoms, which health professionals might not associate with TB. There can also be difficulties
in obtaining microbiological samples; in 2013, only 59% of all new TB diagnoses were confirmed by laboratory culture (PHE, 2014b). Abubakar et al (2012) suggested that, until there are high
levels of awareness for TB in all patient groups, early diagnosis will not be achieved. An essential part of a TB nurse specialist’s role is to promote awareness among health and social care
professionals, in particular, those who work with high-risk communities (Royal College of Nursing, 2012). Griffiths et al (2007) found evidence that a primary care educational intervention
to promote screening could improve early identification of both active and latent TB infection. MORE PROACTIVE APPROACHES It is not necessary, practical or cost effective to screen everyone
within the UK for TB. However, potential groups for active case finding are: * High-risk populations; * Those in high-risk occupational settings, such as staff in health, elderly and
psychiatric care settings; * Patients with comorbidities - for example, those who are HIV positive (Zenner et al, 2013). Van Hest et al (2014) highlighted that high population densities
create specific opportunities for TB transmission, but also enable specific interventions that would not be efficient or effective in a general population. Initiatives such as the find and
treat team’s mobile X-ray unit, which aims to access hard-to-reach groups by visiting homeless hostels and soup kitchens across London, have been found to be effective (Story et al, 2012).
Within the UK, close contact (often in the household or workplace) is the dominant cause of TB transmission (Begun et al, 2013). The aim of contact tracing is to identify and screen people
who have had regular and prolonged exposure to infectious TB. Unpublished data from PHE’s London TB Extended Contact Tracing Team shows that on-site screening in community and institutional
settings (such as schools and workplaces) is effective at detecting both active and latent infection. In about two-thirds of TB patients who were born outside the UK, the disease is not due
to recent transmission, but reactivation of infection acquired abroad (Abubakar et al, 2012). Screening and treating latent infection in new migrant populations is an important public health
action as it could reduce a significant proportion of TB cases. However, in the UK, Pareek et al (2011) found screening for latent TB infection was highly variable, deviated from national
guidance and was inversely related to regional TB burden. CONCLUSION A delay in TB diagnosis causes poorer outcomes and increases opportunities for transmission. Control of the spread of TB
requires early diagnosis and support for patients to ensure they complete treatment to reduce the time they are infectious. Examining and addressing the barriers of the patient-initiated
pathway will assist in achieving earlier diagnosis (Box 2). This requires multiple actions including promoting the awareness of TB, increasing clinical suspicion, early collection of
diagnostic samples (for example sputum) and simple referral pathways. In addition, active case-finding initiatives are necessary to identify people who are at a higher risk of TB infection
but might not have started the patient-initiated pathway. With improved surveillance data, barriers to early diagnosis can be identified and used to inform better-targeted interventions.
Ultimately, TB control in the UK also depends on global programmes, and requires collaborative working and sharing evidence-based approaches. Nurses in all areas of healthcare are essential
to TB care and control. BOX 2. ACTIONS FOR PROMOTING EARLIER DIAGNOSIS OF TB * Promoting awareness of TB * Increasing clinical suspicion of TB * Early collection of diagnostic samples (such
as sputum) * Simple referral pathways * Active case finding in high-risk populations KEY POINTS * The UK has some of the highest tuberculosis infection rates in Western Europe * 10-30% of
people exposed to TB will become infected * More than one in four patients with pulmonary TB start treatment more than four months after the onset of symptoms * As well as the lungs, TB
affects many other organs * A proactive approach may be needed to find TB cases ABUBAKAR I ET AL (2012) Controversies and unresolved issues in tuberculosis prevention and control: a
low-burden-country perspective._ Journal of Infectious Diseases_; 205: S293-300. BEGUN M ET AL (2013) Contact tracing of tuberculosis: a systematic review of transmission modelling studies.
_PLoS One_; 8: e72470. FRENCH CE ET AL (2009) The influence of socio-economic deprivation on tuberculosis treatment delays in England, 2000-2005. _Epidemiology and Infection_; 137: 591-596.
GRIFFITHS C ET AL (2007) Educational outreach to promote screening for TB in primary care: a cluster randomized controlled trial. _Lancet_; 369: 1,528-1,534. NATIONAL INSTITUTE FOR HEALTH
AND CARE EXCELLENCE (2011) _Tuberculosis: Clinical Diagnosis and Management of Tuberculosis, and Measures for its Prevention and Control_. NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE
(2012) _Identifying and Managing Tuberculosis Among Hard-to-Reach Groups_. PAREEK M ET AL (2011) Tuberculosis screening of migrants to low-burden nations: insights from evaluation of UK
practice. _European Respiratory Journal_; 37: 1,175-1,182. PUBLIC HEALTH ENGLAND (2013)_ Tuberculosis in the UK: 2013 Report_. PUBLIC HEALTH ENGLAND (2014a) _From Evidence into Action:
Opportunities to Protect and Improve the Nation’s Health_. PUBLIC HEALTH ENGLAND (2014b) _Tuberculosis in the UK: 2014 Report_. PUBLIC HEALTH ENGLAND, NHS ENGLAND (2015)_ Collaborative
Tuberculosis Strategy for England 2015-2020_. ROYAL COLLEGE OF NURSING (2012) Tuberculosis Case Management and Cohort Review. STORY A ET AL (2012) Active case finding for pulmonary
tuberculosis using mobile digital chest radiography: an observational study. _International Journal of Tuberculosis and Lung Disease_; 16: 1461-1467. VAN HEST NA ET AL (2014) Tuberculosis
control in big cities and urban risk groups in the European Union: a consensus statement. _Eurosurveillance_; 19: 9, pii=20728 WILLIAMS G (2008) _TB Guidelines for Nurses in the Care and
Control of Tuberculosis and Multi-Drug Resistant Tuberculosis_. WORLD HEALTH ORGANIZATION (2011) _Early Detection of Tuberculosis: an Overview of Approaches, Guidelines and Tools_. WORLD
HEALTH ORGANIZATION (2014a) _Global Tuberculosis Report 2014_. WORLD HEALTH ORGANIZATION (2014b) Framework Towards Tuberculosis Elimination in Low-Incidence Countries. ZENNER D ET AL (2103)
Active case finding for tuberculosis among high-risk groups in low-incidence countries. _International Journal of Tuberculosis and Lung Disease_; 17: 573-82.