- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Serious medical diagnostic errors lead to adverse patient outcomes and increased healthcare costs. The use of virtual online consultation platforms may lead to better-informed
physicians and reduce the incidence of diagnostic errors. Our aim was to assess the usage characteristics of an online, physician-to-physician, no-cost, medical consultation platform,
Medscape Consult, from November 2015 through October 2017. Physicians creating original content were noted as “presenters” and those following up as “responders”. During the study period,
37,706 physician users generated a combined 117,346 presentations and responses. The physicians had an average age of 56 years and were from 171 countries on every continent. Over 90% of all
presentations received responses with the median time to first response of 1.5 h. Overall, computer- and device-based medical consultation has the capacity to rapidly reach a global medical
community and may play a role in the reduction of diagnostic errors. SIMILAR CONTENT BEING VIEWED BY OTHERS DIGITAL CONSULTS IN HEART FAILURE CARE: A RANDOMIZED CONTROLLED TRIAL Article
Open access 31 August 2024 ENHANCING TRANSLATIONAL MEDICAL RESEARCH THROUGH PROOF-OF-CONCEPT SERVICES: CLINICIANS’ PERSPECTIVES Article Open access 28 December 2024 A CROSS-SECTIONAL STUDY
OF POLICIES FROM AMERICAN MEDICAL ORGANIZATIONS ABOUT PUBLIC COMMUNICATIONS FROM PHYSICIANS IN THE DIGITAL AGE Article Open access 28 November 2024 INTRODUCTION Medical diagnostic errors are
not infrequent and are a major cause of adverse outcomes in both the inpatient and outpatient setting.1,2,3 Outpatient diagnostic error rates have been estimated at 5% affecting >12
million individuals per annum, whereas inpatient diagnostic errors range from 6 to 7%.2 In fact, when using expert consultants as the ground truth for diagnosis, >20% of referral
diagnoses in a recent study were vastly different compared with final diagnoses.4 This illustrates the importance of strong physician networks to discuss potential diagnoses and obtain
second opinions on specific cases. Although informal face-to-face consultations, known more commonly as curbside consultations, are frequently inaccurate and incomplete when compared with
formal professional consultations.5,6 However, factors relating to physician confidence, access to specialists, affordability of care, and availability of health informatics resources have
all been recognized as probable barriers preventing a formalized networked approach thus leading to diagnostic errors.3,7 While the library stacks were once a treasure trove of valuable
information to potentially crack difficult cases, the role of medical libraries and librarians has changed immensely over time.8,9 The growth of digital technologies has rapidly changed the
way medical information is exchanged and gathered.10 Currently, online references and mobile applications are increasingly accessed by medical professionals than print journals.11 While
social media and crowdsourcing have been shown to reduce costs and improve speed of information exchange, in research little has been published with regards to contemporary, virtual,
peer-to-peer medical second opinion networks.10,12,13,14 While several healthcare organizations worldwide using electronic consultation (eConsult) services within their electronic health
record or closed system communications to shorten the length of time it takes for patients to be evaluated by medical sub-specialists have shown improved patient and provider satisfaction,
much of the published analysis of eConsult services excludes open, crowdsourced, peer-to-peer networks.15,16 Here, we aimed to capitalize on the global reach of the largest online community
of physicians and healthcare providers (Medscape) to examine the profiles and characteristics of use within a freely available, virtual platform for crowdsourced medical consultation with
over 37,000 active users. RESULTS From the launch of Medscape Consult on 10 November 2015, through 12 October 2017, there were 310,563 individual physicians who accessed the Medscape Consult
platform. Of this user base, 37,706 physicians were active users and created 117,346 posts (7834 original presentations and 109,512 responses). Original presentations (patient cases) are
defined here as primary content sharing either clinical cases or presenting clinical queries while responses are created by users in reply to original presentations. Examples of original
presentations and responses are included as supplementary material (Supplementary Information). The majority of active users interacting on the platform created responses only, 34,046
(90.3%) users, whereas 3660 (9.7%) users created both original presentations and responses. The platform was accessible both by mobile device (Android and iOS) and personal computer. The
majority of activity was created from a mobile device (67.4%) with only 32.5% of all engagements with the platform being done on a personal computer. This held true for both original
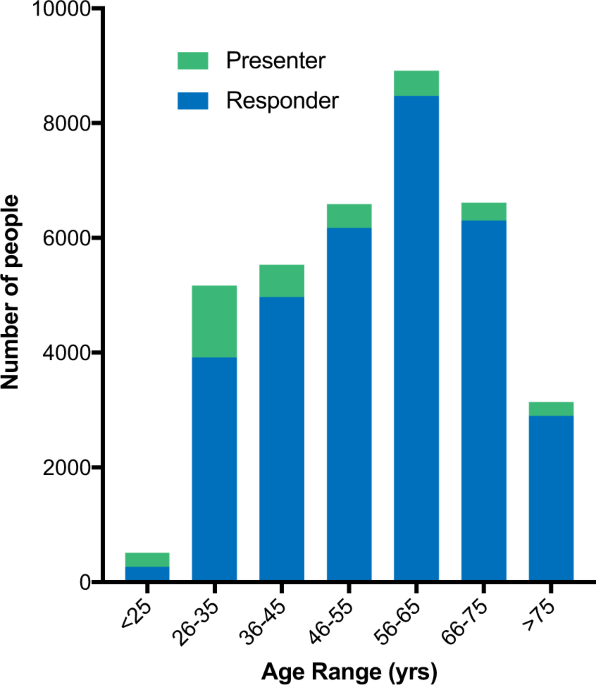
presentations and responses. The mean age of all users on the platform was 54.5 (SD 15.7) years with users who created original presentations being younger, mean age 44.7 (SD 17.7) years, as
compared with users who solely provided responses, mean age 55.5 (SD 15.2) years. This is reflected in Fig. 1 showing that younger users represented a larger proportion of users creating
original presentations than older users. Overall, users identified as having obtained an M.D. (75.3%), non-U.S. M.D. equivalent (7.2%), or Doctor of Osteopathic Medicine (D.O.) (3.0%),
though (14.5%) of users did not specify their highest degree of training. Platform users were registered in 171 separate United Nations defined countries representing every continent. The
majority of users were registered in the United States (33.7% of total users), followed by users in Europe (19.2%), Latin America (14.3%), North Africa and Western Asia (11.2%), and
Central/Eastern Asia (10.8%). However, original presentation activity came from a diverse user base, with users creating original presentations registered in the United States (26.3% of
users who created presentations), North Africa/Western Asia (25.3%), and Central/Eastern Asia (21.6%) representing the top three regions. Over a quarter of the users on the platform who had
either posted original presentations or made responses identified Internal Medicine (26.9%) as their primary medical specialty (Fig. 2a). Pediatrics (8.9%), Cardiology (7.3%), Obstetrics and
Gynecology (6.3%), and Dermatology (4.8%) were the next most populous specialties making up the top five user groups. In terms of overall activity, users from Internal Medicine provided the
most original presentations (31.5%), as well as responses (27.9%) (Fig. 2b). In general, content creation (presentations and responses) on the platform mirrored overall user percentages,
with some exceptions. While Dermatology, accounting for the fifth most popular user group (4.8%), provided the second highest percentage of responses (9.0%), they were seventh (4.3%) in
creation of original presentations. Alternatively, Obstetrics and Gynecology was the fourth most popular user group (6.3%) on the platform but ranked 10th in providing original presentations
(3.1%) though ranking 5th (4.7%) in terms of overall comments. Of the 7834 original presentations and 109,512 responses, the majority of users creating content did so on a single occasion
with 78.2% of the users creating a single original presentation and 62.0% creating a single response (Fig. 3a). However, five users created between 51 and 100 original presentations, and six
users created >100 original presentations each, with 212 posts by a single user being the highest per individual. While users creating responses were more likely than users creating
presentations to do so more than once, the median for each group was 1. And, like users creating original presentations, there were several “super users”, with 16 individuals creating
between 51 and 100 responses and 19 users who created >100 responses, with the highest being 1748 responses by a single user. The 3660 users (9.7% of total platform users) creating
original presentations also created 27.4% of the total responses on the platform during the study period. Additionally, of the entire physician population accessing the platform (310,563
physicians) during the study period, two-thirds returned to the site more than once. Most original presentations generated interest by responders with 65.2% of original presentations
receiving between 1 and 10 responses (Fig. 3b). Although 7.2% of the original presentations received no responses from other users. The median number of responses per original presentation
was 5.4 and the maximum number of responses created in reply to a single presentation was 880. For each presentation initiated on the platform that received a response, the median time to
first response was 1.5 h. The first response to nearly a quarter of these original presentations (22.6%) occurred within 30 min and within at least 15 h for 89.2%. Monthly engagement on the
platform increased during the time period studied (Fig. 4). Linear regression analysis, excluding incomplete months, illustrated statistically significant increases in original presentations
over time (slope 1.34, Pearson _r_ = 0.5909, _p_-value 0.004) and responses (slope 30.48, Pearson _r_ = 0.6053, _p_-value 0.003). We found that while the number of presentations made
remained relatively consistent throughout the week with little variation, response activity was the highest on Sunday. DISCUSSION Smartphones and computers are pervasive in the outpatient
and hospital environment, setting up the potential for virtual medical crowdsourcing and moving from the classic second opinion to the _n_th opinion. Here, we aimed to understand this
growing space by exploring the characteristics of early physician adopters and the usage statistics using a new digital medical app platform, Medscape Consult. We found rapid, voluntary
engagement from physicians of all ages and medical sub-specialties from around the globe. Medscape Consult is not the only platform for providing a real-time portal for virtual
physician-to-physician engagement. Several crowdsourced diagnostic platforms have been evaluated though these studies have been small in size and from limited locations.11,17,18 Similar to
Medscape Consult, many of the popular crowdsourced platforms are open solely to validated clinicians including the Human Diagnosis Project, Sermo, QuantiaMD and Fig. 1, the later having been
touted as the “Instagram for doctors”, focusing on medical image sharing. Other platforms, such as HealthTap and CrowdMed, provide virtual dialogs between both patients and medical
professionals in search for diagnostic answers. eConsult services within closed healthcare systems have been studied extensively. Although not considered crowdsourced platforms, when
physicians were polled about the utility of these services, the eConsult services ranked highly for perceived improvement of patient management,19 providing value to patients and
providers20,21,22 and the vast majority of participating physicians stated that they improved their medical knowledge.23 Collectively, digital online platforms aim to vastly expand resources
and potentially provide for a more formalized and clear discussion of specific cases. Here, we show that Medscape Consult was being utilized by physicians of all ages from around the world.
Interestingly, there was an age offset for presenters and responders. Younger physicians were responsible for creating the majority of original presentations, with one-fifth created by
physicians 26–30 years of age, while users who had presumably been in practice longer were engaged within this community with more responses. This could potentially be the result of better
familiarity with social networking and mobile medical apps for younger physicians having trained in a digital era. However, with the majority (>60%) of all responses coming from physician
users over 60 years of age, it is clear that older physicians feel comfortable with and support this type of virtual engagement. This certainly illustrates the broad appeal of a virtual
medial consultation platform. The opportunity to query the Medcape Consult user base in addition to physicians on Medscape who are not using the Medscape Consult platform on their overall
digital savvy and acceptance of crowdsourced decision-making tools such as this would be an appropriate next step to understand potential barriers. This would also be an important step in
gaining insight on the age discrepancies related to virtual content creation in this cohort. The global reach of the platform was extraordinary with physician users from every continent
creating original content as presentations or responses. As expected for a English language-based platform, the greatest number of users were registered in the United States and Europe,
though users from Asia, Latin America, North Africa/Western Asia, and Central/Eastern Asia each made up at least 10% of the active user base on the platform. This global reach is
increasingly important to physicians given the populations increased access to world travel and spread of diseases that traditionally had been limited geographically. Given that physicians
in Internal Medicine/General Practice and Family Medicine (included in the Internal Medicine classification here) make up the most populous specialty in practice, it was not surprising that
physicians in this category were the highest user population and accounted for the highest percentage of engagement. Activity from Hematology/Oncology, especially the number of responses to
original presentations was higher than their representation as active users. Conversely, engagement activity by Obstetrics/Gynecology was less than would be expected by the number of users
on the platform. Our study had several limitations. Most importantly, we do not have the final diagnoses for each presenter to determine whether peer input improved accuracy. This
information would be vital to connecting improved diagnostic abilities using a crowdsourced virtual consultation platform and reducing diagnostic medical errors. A follow-up survey sent to
users creating original presentations 1 week after going live may be a potential option for the platform to gain this data. Similarly for eConsult services, data pertaining to patient
outcomes has been lacking and poorly reported in prior studies.15 The true reach of the platform is unknown as our analysis did not account for physicians who had access to the platform but
did not engage in content creation. While there was overall growth in the creation of content during the study time, the proportion of users who only engaged once (through either a
presentation or response) remain the majority. This remains an important concept for the success of platforms like this moving forward though outside the scope of this study. The
patient–doctor experience is a personal one and that these “_n_th opinions” took place virtually and only based on potentially biased information provided by the presenter, the responders
are not afforded the opportunity to fully examine the patient. Thus, important aspects of the physical exam, interpersonal discussion, and subtle clues to diagnosis are likely lost in this
digital space, which could potentially increase the risk of diagnostic inaccuracy. Similarly, aspects related to user experience and user interface that may impact long-term retention with
digital tools remain unexplored but may be key factors in this lower than expected number of frequent users. Artificial intelligence has been advocated as the definitive pathway for reducing
misdiagnosis. But our findings suggest the potential for collective human intelligence, which is algorithm-free and performed rapidly on a voluntary basis, to emerge as a competitive or
complementary strategy. While there are certainly more refinements and study of this platform required, we have demonstrated an extraordinary reach and potential for a multispecialty,
crowdsourced, global virtual consultation platform at scale for physicians in search of diagnostic input. METHODS SAMPLE Participants were registered users of Medscape Consult
(https://www.medscape.com/consult), a no-cost, online community where physicians are able to ask and answer clinical questions and discuss clinical challenges. Access to the online community
was available via home computers, web-enabled mobile devices, and a mobile application. The study sample consisted of 37,706 physicians who created content between 10 November 2015 and 12
October 2017. During the time that this platform was studied, users were restricted to individuals who had received a medical degree. Content creation was defined as publishing an original
presentation or response. All participants completed an online account setup process and agreed to terms of service that allowed for data to be analyzed in aggregate. The study was conducted
in accordance with all relevant guidelines and procedures and approved by the Scripps IRB. STATISTICAL ANALYSIS Demographic characteristics of the study sample were described according to
categories of presenters (defined as those who published an original query or case) and responders (defined as those who only ever commented on an existing presentation) using univariate
descriptive statistics (i.e., proportions and means and standard deviations). Univariate descriptive statistics were similarly used to describe the characteristics of the presentations and
responses over time (months and day of the week) and according to medical specialty, geographic region of origin, device of origin, and categories of presenters and responders. Linear
regression was used to examine change in monthly engagement. Original presentations were described by assessing the quantity and the amount of elapsed time between an original presentation
and the first and last corresponding response was assessed using univariate descriptive statistics. All statistical analyses were conducted using STATA 13.0 (StataCorp, College Station, TX,
USA). DATA AVAILABILITY No unique coding or algorithms were utilized for the analysis. De-identified data access will be considered as needed for other researchers. REFERENCES * Khullar, D.,
Jha, A. K. & Jena, A. B. Reducing diagnostic errors--why now? _N. Engl. J. Med._ 373, 2491–2493 (2015). Article Google Scholar * Singh, H., Meyer, A. N. & Thomas, E. J. The
frequency of diagnostic errors in outpatient care: estimations from three large observational studies involving US adult populations. _BMJ Qual. Saf._ 23, 727–731 (2014). Article Google
Scholar * Singh, H., Schiff, G. D., Graber, M. L., Onakpoya, I. & Thompson, M. J. The global burden of diagnostic errors in primary care. _BMJ Qual. Saf._ 26, 484–494 (2017). Article
Google Scholar * Van Such, M., Lohr, R., Beckman, T. & Naessens, J. M. Extent of diagnostic agreement among medical referrals. _J. Eval. Clin. Pract._ 23, 870–874 (2017). Article
Google Scholar * Keating, N. L., Zaslavsky, A. M. & Ayanian, J. Z. Physicians’ experiences and beliefs regarding informal consultation. _JAMA_ 280, 900–904 (1998). Article CAS Google
Scholar * Kuo, D., Gifford, D. R. & Stein, M. D. Curbside consultation practices and attitudes among primary care physicians and medical subspecialists. _JAMA_ 280, 905–909 (1998).
Article CAS Google Scholar * Meyer, A. N., Payne, V. L., Meeks, D. W., Rao, R. & Singh, H. Physicians’ diagnostic accuracy, confidence, and resource requests: a Vignette study. _JAMA
Intern. Med._ 173, 1952–1958 (2013). Article Google Scholar * Sollenberger, J. F. & Holloway, R. G.Jr. The evolving role and value of libraries and librarians in health care. _JAMA_
310, 1231–1232 (2013). Article Google Scholar * McGowan, J., Hogg, W., Campbell, C. & Rowan, M. Just-in-time information improved decision-making in primary care: a randomized
controlled trial. _PLoS ONE._ 3, e3785 (2008). Article Google Scholar * Rumsfeld, J. S. et al. Use of mobile devices, social media, and crowdsourcing as digital strategies to improve
emergency cardiovascular care: a scientific statement from the American Heart Association. _Circulation_ 134, e87–e108 (2016). Article Google Scholar * Sims, M. H., Fagnano, M., Halterman,
J. S. & Halterman, M. W. Provider impressions of the use of a mobile crowdsourcing app in medical practice. _Health Inform. J._ 22, 221–231 (2016). Article Google Scholar * Barreto,
J. E. & Whitehair, C. L. Social media and web presence for patients and professionals: evolving trends and implications for practice. _PM&R_ 9, S98–S102 (2017). Article Google
Scholar * Jutel, A. & Lupton, D. Digitizing diagnosis: a review of mobile applications in the diagnostic process. _Diagnosis (Berl.)_ 2, 89–96 (2015). Google Scholar * Ranard, B. L. et
al. Crowdsourcing--harnessing the masses to advance health and medicine, a systematic review. _J. Gen. Intern. Med._ 29, 187–203 (2014). Article Google Scholar * Liddy, C., Moroz, I.,
Mihan, A., Nawar, N. & Keely, E. A systematic review of asynchronous, provider-to-provider, electronic consultation services to improve access to specialty care available worldwide.
_Telemed. J. E. Health_, https://doi.org/10.1089/tmj.2018.0005 (2018). * Vimalananda, V. G. et al. Electronic consultations (e-consults) to improve access to specialty care: a systematic
review and narrative synthesis. _J. Telemed. Telecare._ 21, 323–330 (2015). Article Google Scholar * Meyer, A. N., Longhurst, C. A. & Singh, H. Crowdsourcing diagnosis for patients
with undiagnosed illnesses: an evaluation of CrowdMed. _J. Med. Internet Res._ 18, e12 (2016). Article Google Scholar * Sims, M. H., Bigham, J., Kautz, H. & Halterman, M. W.
Crowdsourcing medical expertise in near real time. _J. Hosp. Med._ 9, 451–456 (2014). Article Google Scholar * Bonnardot, L. et al. The development of a multilingual tool for facilitating
the primary-specialty care interface in low resource settings: the MSF Tele-Expertise System. _Front. Public Health_ 2, 126 (2014). Article Google Scholar * Liddy, C., Deri Armstrong, C.,
McKellips, F. & Keely, E. A comparison of referral patterns to a multispecialty eConsultation service between nurse practitioners and family physicians: the case for eConsult. _J. Am.
Assoc. Nurse Pract._ 28, 144–150 (2016). PubMed Google Scholar * Liddy, C., Drosinis, P., Joschko, J. & Keely, E. Improving access to specialist care for an aging population.
_Gerontol. Geriatr. Med._ 2, 2333721416677195 (2016). Article Google Scholar * Liddy, C. et al. Improving access to chronic pain services through eConsultation: a cross-sectional study of
the champlain BASE eConsult service. _Pain. Med_. https://doi.org/10.1093/pm/pnw038 (2016). * Thijssing, L. et al. Telepulmonology and telespirometry. _Stud. Health Technol. Inform._ 205,
211–215 (2014). PubMed Google Scholar Download references ACKNOWLEDGEMENTS This study was supported by UL1TR002550 from NCATS/NIH to The Scripps Research Institute. AUTHOR INFORMATION
AUTHORS AND AFFILIATIONS * Scripps Research Translational Institute, The Scripps Research Institute, La Jolla, CA, USA Evan D. Muse, Job G. Godino & Eric J. Topol * Division of
Cardiovascular Disease, Scripps Clinic-Scripps Health, La Jolla, CA, USA Evan D. Muse & Eric J. Topol * University of California San Diego, La Jolla, CA, USA Job G. Godino * Medscape,
WebMD, New York, NY, USA Jessa F. Netting, James F. Alexander & Helen J. Moran Authors * Evan D. Muse View author publications You can also search for this author inPubMed Google Scholar
* Job G. Godino View author publications You can also search for this author inPubMed Google Scholar * Jessa F. Netting View author publications You can also search for this author inPubMed
Google Scholar * James F. Alexander View author publications You can also search for this author inPubMed Google Scholar * Helen J. Moran View author publications You can also search for
this author inPubMed Google Scholar * Eric J. Topol View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS All authors were involved in the design
and planning of the current study. J.F.N., J.F.A., and H.J.M. gathered the user-level data. E.D.M. and J.G.G. independently prepared and analyzed the data. E.D.M., J.G.G., and E.J.T. wrote
the manuscript with all authors providing comments, edits, and approval of the final version. CORRESPONDING AUTHOR Correspondence to Eric J. Topol. ETHICS DECLARATIONS COMPETING INTERESTS
J.F.N., J.F.A., and H.J.M. are employees of WebMD, which hosts the Medscape Consult platform. E.J.T. is a Editor-in-Chief of Medscape/WebMD. The remaining authors declare no competing
interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. ELECTRONIC
SUPPLEMENTARY MATERIAL SUPPLEMENTARY INFORMATION RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits
use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the
Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated
otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds
the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and
permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Muse, E.D., Godino, J.G., Netting, J.F. _et al._ From second to hundredth opinion in medicine: A global consultation platform for physicians.
_npj Digital Med_ 1, 55 (2018). https://doi.org/10.1038/s41746-018-0064-y Download citation * Received: 13 June 2018 * Revised: 17 September 2018 * Accepted: 19 September 2018 * Published:
09 October 2018 * DOI: https://doi.org/10.1038/s41746-018-0064-y SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative