- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT We aimed to evaluate the impact of fellowship training (FT) for thyroid specialists on the outcomes of patients with thyroid cancer. We reviewed surgeries performed for thyroid
cancer before (non-FT group) and after (FT group) fellowship training and compared several variables, including length of stay of patients, tumor diameter, surgical method, lymph node
dissection, parathyroid implantation, surgical duration, intraoperative blood loss, and postoperative complications. Compared with the non-FT group, the FT group had a shorter hospital stay,
more adequate fine needle aspiration biopsy of the thyroid, less intraoperative blood loss, higher rate of parathyroid implantation, higher lymph node dissection rate, and lower nerve
injury and hypoparathyroidism rates. When the surgical duration was < 200 min and/or only central lymph node dissection was performed, the FT group had a lower incidence of postoperative
complications than the non-FT group. When, the incidence of postoperative complications, including postoperative nerve injury and hypoparathyroidism. In conclusion, FT for thyroid
specialists is beneficial for patients with thyroid cancer and may allow a shorter hospital stay and reduced incidence of postoperative complication. Accordingly, FT may facilitate a more
appropriate surgical approach with a preoperative pathological diagnosis. SIMILAR CONTENT BEING VIEWED BY OTHERS CHANGES IN THYROID SURGERY OVER LAST 25 YEARS Article Open access 25 April
2025 POSTOPERATIVE COMPLICATIONS AND LONG-TERM OUTCOMES AFTER TOTAL AND SUBTOTAL THYROIDECTOMY: A RETROSPECTIVE STUDY Article Open access 29 January 2025 TRANSAXILLARY VS. TRANSSUBCLAVIAN
GASLESS ENDOSCOPIC THYROIDECTOMY APPROACHES FOR PAPILLARY THYROID CANCER Article Open access 02 January 2025 INTRODUCTION The annual incidence of thyroid cancer has been increasing
worldwide1,2, reaching nearly 10.1 per 100,000 women and 3.1 per 100,000 men3. As the tumor size gradually increases, the compression of the surrounding tissue becomes more pronounced,
resulting in symptoms such as dyspnea, dysphagia, hoarseness, and Horner’s syndrome4,5,6. Fellowship training (FT) for specialists is an important aspect of postgraduate medical education
and allows training of qualified clinical specialists7. Micah et al.8 reported that physicians trained through an endourology fellowship had a higher stone-free rate, lower complication and
reoperation rates, and better postoperative follow-up outcomes. Further, Shabnam et al.7 found that trained gynecologists had a lower incidence of ureteral injury during laparoscopic
hysterectomy. Similar conclusions have been reached in studies on orthopedics, with trained orthopedic surgeons showing significantly shorter surgical times, fluoroscopy usage, and traction
times9,10,11. However, the effectiveness of FT in thyroid surgery remains unclear12. Therefore, this retrospective study aimed to compare hospitalization data and postoperative complication
rates in patients who underwent thyroid surgical interventions, in order to determine whether clinicians with FT could improve the prognosis of patients with thyroid cancer. METHODS FT was
conducted at the Thyroid and Breast Surgery Department of the Second Affiliated Hospital of Fujian Medical University, where the annual surgical volume was over 2000 cases. FT began in July
2019, before which no surgeons received FT. Since July 2019, all thyroid surgeons at our department have undergone the two-year FT. Surgeons in the FT and non-FT group have similar level of
education and academic qualifications. DATA SOURCE AND PATIENT SELECTION This was a retrospective study of thyroid cancer surgery in the Second Affiliated Hospital of Fujian Medical
University, including patients who underwent surgeries performed by thyroid surgeons without (January 2018–October 2018) and with (May 2022–September 2022) FT. Baseline patient information,
admission time, discharge time, surgical records, and postoperative complications were collected from the hospital database; moreover, telephone follow-up interviews were conducted. The
collected parameters included patient ID, sex, age, hospital stay length, fine-needle aspiration biopsy (FNA) of the thyroid, selected surgical method, lymph node dissection, parathyroid
implantation, surgical duration, intraoperative blood loss, and postoperative complications. We used the TNM staging system for thyroid cancer developed by the American Joint Committee on
Cancer13 to divide the tumors into ≤ 1, 1–2, 2–4, and > 4 cm categories. Subsequently, we compared the characteristics of thyroid cancer between the FT and non-FT groups. According to the
recommendations of the 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer14, thyroid cancer surgeries were
divided into four categories: (1) unilateral (+ isthmus) thyroidectomy; (2) subtotal or near-total thyroidectomy; (3) total thyroidectomy; and (4) others, including thyroidectomy with
microwave ablation, lymph node dissection, biopsy, and isthmus resection. Lymph node dissection was divided into three categories: (1) no dissection, (2) central lymph node dissection
(CLND), and (3) central and cervical lymph node dissection. ETHICS This study was conducted in accordance with the current version of the Declaration of Helsinki and good clinical practice
guidelines15. This retrospective study was approved by the Medical Ethics Committee of the Second Affiliated Hospital of Fujian Medical University(No. 610, 2023), which waived the
requirement for informed consent. STATISTICAL ANALYSIS Statistical analyses were performed using IBM SPSS Statistics v.26 (IBM Corp., Armonk, NY, USA). Fisher’s exact test and the chi-square
test were used to identify between-group differences in clinical data. Normally distributed quantitative data are expressed as mean ± standard deviation \(\left( {\overline{{\text{x}}} \pm
s} \right)\) and converted into categorical variables for between-group comparison. Qualitative data are described by frequency, with between-group comparisons using the chi-square and
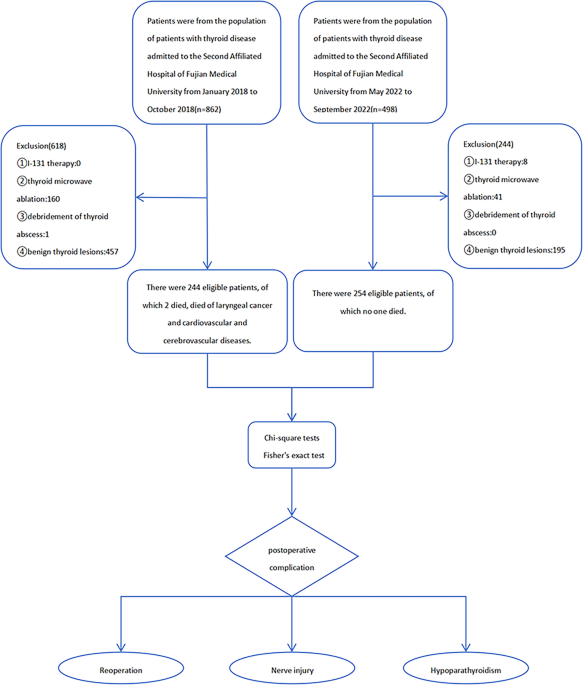
Fisher’s exact tests. Statistical significance was set at _p_ < 0.05. RESULTS Between January 2018 and October 2018 (non-FT group), 862 patients with thyroid disease were admitted to the
Second Affiliated Hospital of Fujian Medical University. Among them, 618 patients were excluded, including 457 with benign thyroid diseases, 160 who underwent thyroid microwave ablation, and
1 with thyroid abscess debridement. Finally, we included 244 patients with thyroid cancer who underwent thyroidectomy. Between May 2022 and September 2022, 498 patients with thyroid
diseases were admitted to the Second Affiliated Hospital of Fujian Medical University (FT group). Among them, 244 patients were excluded, including 195 with benign thyroid diseases, 41 with
thyroid microwave ablation, and 8 with I131 therapy. Finally, we included 254 patients with thyroid cancer who underwent thyroidectomy. Although 17 and 7 patients in the non-FT and FT
groups, respectively, were lost to follow-up, and 2 patients in the non-FT group died from other diseases after discharge, the hospital data for these patients were complete; therefore, they
were included in the analysis. Ultimately, 498 patients with thyroid cancer were eligible for study inclusion (Fig. 1). Table 1 summarizes the clinical characteristics of the patients. All
patients were followed up for ≥ 6 postoperative months. IMPACT OF FT ON HOSPITALIZATION AND SURGICAL DATA As shown in Table 2, compared with the non-FT group, the FT group had a shorter
hospital stay (9.09 ± 5.207 vs. 5.38 ± 2.185 days, _p_ = 0.000) and higher preoperative FNA rate (34.6 vs. 23.8%, _p_ = 0.008). There were no significant between-group differences in the
operating time (129.53 ± 65.960 [non-FT] vs. 117.75 ± 53.109 [FT] min, _p_ = 0.095); however, the amount of intraoperative blood loss was lower in the FT group than in the non-FT group
(20.08 ± 26.565 vs. 36.77 ± 86.097 mL, _p_ = 0.000). Compared with the non-FT group, the FT group had a higher parathyroid implantation rate (66.9 vs. 11.1%, _p_ = 0.000) and proportion of
unilateral thyroidectomies (68.1 vs. 45.1%, _p_ = 0.000). POSTOPERATIVE COMPLICATIONS There were two postoperative bleeding cases (0.8%) in the non-FT group and one (0.4%) in the FT group,
with no significant between-group difference (_p_ = 0.617). Compared with the non-FT group, the FT group had lower risks of postoperative nerve injury (7.3 vs. 16.9%, _p_ = 0.001) and
hypoparathyroidism (12.6 vs. 24.9%, _p_ = 0.001) (Table 2). As shown in Table 3, patients were further stratified according to their operating time. When surgical duration was ≤ 200 min, the
risks of nerve injury (7.0 vs. 16.4%, _p_ = 0.002) and hypoparathyroidism (12.6 vs. 25.4%, _p_ = 0.001) were lower in the FT group than in the non-FT group, with no significant
between-group difference in nerve injury (_p_ = 0.679) and hypoparathyroidism (_p_ = 0.679) when the operation time was > 200 min. Postoperative complications occurred at different ranges
of lymph node dissection between the two groups. In patients with CLND, the incidences of nerve injury (7.1 vs. 13.6%, _p_ = 0.037) and hypoparathyroidism (13.2 vs. 24.1%, _p_ = 0.007) were
lower in the FT group than in the non-FT group, with no significant between-group differences in the incidence of nerve injury (_p_ = 0.150) or hypoparathyroidism (_p_ = 0.310) among
patients without lymph node dissection. In patients who underwent central and cervical lymph node dissection, there were no significant between-group differences in the incidence of nerve
injury (_p_ = 0.418) or hypoparathyroidism (_p_ = 0.098). DISCUSSION Over the past three decades, there has been a gradual increase in the incidence of thyroid cancer, which may be
attributed to its active detection and early diagnosis16,17,18,19. This growth poses a significant challenge for healthcare systems worldwide. Therefore, clinicians are required to actively
improve clinical diagnosis and treatment techniques to delay thyroid cancer progression, and therefore improve patient outcomes14. We have illustrated in Fig. 2 the similarities and
differences in the extent of thyroidectomy, related surgical operations, and major surgical complications between the two groups. In our study, compared with the non-FT group, the FT group
had a shorter hospital stay and less intraoperative blood loss. This indicated that patients in the FT group had less intraoperative injury and a faster postoperative recovery, subsequently
leading to a reduction in hospitalization costs. Preoperative FNA is helpful in the diagnosis of benign and malignant thyroid nodules in order to determine the optimal treatment and whether
lymph node dissection is warranted20. The procedure helps determine the preoperative nature of the thyroid mass in order to allow patients to obtain optimal benefits from the smallest
surgical range21. The preoperative FNA rate was higher in the FT group than in the non-FT group. In this study, 45.1% and 68.1% of patients in the non-FT and FT groups, respectively,
underwent a unilateral thyroidectomy. This could be attributed to trained thyroid physicians having better diagnostic skills and treatment techniques, which maximized benefits for patients
with fewer injuries22,23. Furthermore, it may be related to the improvement in imaging technology24, which has contributed to the early diagnosis and treatment of patients with thyroid
cancer. Compared with the non-FT group, the FT group had more patients who underwent unilateral thyroidectomy, which may explain the shorter average hospitalization time and fewer
postoperative complications in this group. In our study, consistent with the American Thyroid Association Guidelines14, total thyroidectomy was implemented for patients who had distant
metastases, marked extraglandular invasion, clear lymph node metastasis, poorly differentiated pathological subtypes, and high-risk factors for previous head and neck radiation exposure
history. Patients who undergo total thyroidectomy are required to take thyroxine for life, which impacts their lives and finances. Therefore, patients in the FT group underwent more
unilateral thyroidectomies within the scope of surgical indications. In the FT group, 85.8% of patients underwent CLND, with this proportion being 14.1% higher than that in the non-FT group.
Most patients had negative lymph nodes on both preoperative and postoperative pathology evaluations. Therefore, we opted for preventive dissection of the CLND (pCLND). However, it remains
unclear whether pCLND should be performed in patients with cN0 thyroid cancer25,26. Therefore, it is important to thoroughly assess the specific situation of patients, evaluate the risk or
benefit of pCLND, and make a choice that is the least harmful but also the most beneficial strategy for patients. In our study, only 7.1% of patients in the FT group did not undergo lymph
node dissection, with the implementation rate being 10.9% lower than that in the non-FT group. This indicates that trained thyroid physicians are more inclined to perform pCLND, which allows
accurate staging for predicting prognosis and determining subsequent treatment20. The intraoperative parathyroid implantation rate was higher in the FT group than in the non-FT group,
indicating a reduced risk of postoperative hypoparathyroidism in patients with thyroid cancer. In terms of the operation time, the incidence of hypoparathyroidism was lower in the FT group
than in the non-FT group when the operation time was ≤ 200 min. Due to the small sample size of this study, this finding requires further verification. In terms of the extent of lymph node
dissection, we observed a significant between-group difference in the incidence of nerve injury and hypoparathyroidism among patients undergoing central lymph node dissection. Specifically,
the incidence of hypoparathyroidism in the FT group was 10.9% lower than that in the non-FT group, indicating that patients with thyroid cancer who were treated by trained thyroid physicians
had a lower risk of postoperative hypoparathyroidism. There was no significant between-group difference in the incidence of nerve injury or hypoparathyroidism among patients who did not
undergo lymph node dissection. This could be attributed to the fact that physicians in both groups could perform a simple thyroidectomy and avoid damage to the parathyroid gland, reducing
the incidence of postoperative hypoparathyroidism. There was no significant between-group difference in the incidence of nerve injury and hypoparathyroidism among patients who underwent
dissection of the central and lateral cervical lymph nodes. This could be attributed to the larger extent of lymph node dissection, which significantly increased the incidence of
postoperative complications. Nerve paralysis may occur due to the inexperience of the surgeon, tumor invasion and infiltration, compression by a large tumor, and surgical manipulation,
including stretch, compression, thermal injury, or transection27. In the present study, the occurrence rate of postoperative nerve injury was lower in the FT group than that in the non-FT
group, which may be explained by the fact that trained surgeons better understand the nerve anatomy, and thus avoid nerve damage. Accordingly, fewer patients in the FT group presented with
postoperative symptoms, including hoarseness and coughing. With regard to operating time stratification, when the operating time was ≤ 200 min, the rate of occurrence of nerve injury was
lower in the FT group than in the non-FT group. This may be due to the fact that trained thyroid surgeons can better grasp the anatomical structure around the thyroid gland as well as the
critical points and difficulties of thyroid surgery, which allows avoidance of intraoperative nerve damage. These parameters did not show a significant between-group difference when the
operating time was > 200 min. This may be related to the long-term traction of the tissue during surgery, which deserves more attention in clinical practice. Based on the extent of lymph
node dissection, we found a significant between-group difference in the rate of occurrence of nerve injury and hypoparathyroidism among patients who underwent CLND. Specifically, the rate of
occurrence of nerve injury was 6.5% lower in the FT group than in the non-FT group, indicating that trained thyroid physicians can reduce the incidence of postoperative nerve injury. The
present study had some limitations. First, this was a retrospective study; therefore, any conclusions drawn were subject to the limitations of the respective study design, including recall
and observation bias. Second, the follow-up period in the non-FT group was longer than that in the FT group; accordingly, subacute and late-onset complications were more likely to be
reported over a longer follow-up period. Third, this study was conducted at a single center with a restricted sample size. The relatively small sample size may have compromised the power of
the primary results. Future studies are warranted to focus on this topic. CONCLUSIONS Our findings showed that FT for thyroid specialists is beneficial for patients with thyroid cancer.
Patients undergoing thyroidectomy by physicians with FT show reduced hospital stay, intraoperative blood loss, and postoperative complications, as well as increased rates of preoperative
FNA, parathyroid implantation, and preventive central lymph node dissection. Future s large-scale studies are warranted to confirm our findings. DATA AVAILABILITY The datasets used and/or
analysed during the current study available from the corresponding author on reasonable request. REFERENCES * La Vecchia, C. _et al._ Thyroid cancer mortality and incidence: A global
overview: Thyroid Cancer Mortality and Incidence. _Int. J. Cancer_ 136(9), 2187–2195 (2015). Article PubMed Google Scholar * Vaccarella, S. _et al._ The impact of diagnostic changes on
the rise in thyroid cancer incidence: A population-based study in selected high-resource countries. _Thyroid_ 25(10), 1127–1136 (2015). Article PubMed Google Scholar * Pizzato, M. _et
al._ The epidemiological landscape of thyroid cancer worldwide: GLOBOCAN estimates for incidence and mortality rates in 2020. _Lancet Diabetes Endocrinol._ 10(4), 264–272 (2022). Article
PubMed Google Scholar * Broome, J. T. _et al._ Anaplastic thyroid cancer manifesting as new-onset horner syndrome. _Endocr. Pract._ 15(6), 563–566 (2009). Article PubMed Google Scholar
* Collazo-Clavell, M. L., Gharib, H. & Maragos, N. E. Relationship between vocal cord paralysis and benign thyroid disease. _Head Neck_ 17(1), 24–30 (1995). Article CAS PubMed Google
Scholar * Cipriani, N. A. _et al._ Large cytologically benign thyroid nodules do not have high rates of malignancy or false-negative rates and clinical observation should be considered: A
meta-analysis. _Thyroid_ 28(12), 1595–1608 (2018). Article PubMed Google Scholar * Gupta, S. _et al._ Very low rates of ureteral injury in laparoscopic hysterectomy performed by
fellowship-trained minimally invasive gynecologic surgeons. _J. Minim. Invasive Gynecol._ 29(9), 1099–1103 (2022). Article PubMed Google Scholar * Levy, M. _et al._ The role of
experience: how case volume and endourology-fellowship training impact surgical outcomes for ureteroscopy. _J. Endourol._ 37(7), 843–851 (2023). PubMed Google Scholar * Fisher, B. T. _et
al._ Does surgeon subspecialty training affect outcomes in the treatment of displaced supracondylar humerus fractures in children?. _J. Am. Acad. Orthop. Surg._ 29(9), e447–e457 (2021).
Article PubMed Google Scholar * Levy, H. A. _et al._ Effect of fellow involvement and experience on patient outcomes in spine surgery. _J. Am. Acad. Orthop. Surg._ 30(17), 831–840 (2022).
Article PubMed Google Scholar * Flores, S. E., Borak, K. R. & Zhang, A. L. Hip arthroscopic surgery for femoroacetabular impingement: A prospective analysis of the relationship
between surgeon experience and patient outcomes. _Orthop. J. Sports Med._ 6(2), 232596711875504 (2018). Article Google Scholar * Harness, J. K. _et al._ Future of thyroid surgery and
training surgeons to meet the expectations of 2000 and beyond. _World J. Surg._ 24(8), 976–982 (2000). Article CAS PubMed Google Scholar * Perrier, N. D., Brierley, J. D. & Tuttle,
R. M. Differentiated and anaplastic thyroid carcinoma: Major changes in the American joint committee on cancer eighth edition cancer staging manual. _CA Cancer J. Clin._ 68(1), 55–63 (2018).
Article PubMed Google Scholar * Haugen, B. R. _et al._ 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer:
The American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. _Thyroid_ 26(1), 1–133 (2016). Article PubMed PubMed Central Google Scholar *
Parsa-Parsi, R. W. The international code of medical ethics of the world medical association. _JAMA_ 328(20), 2018 (2022). Article Google Scholar * Schuster-Bruce, J. _et al._ A
comparison of the burden of thyroid cancer among the european union 15+ countries, 1990–2019: Estimates from the global burden of disease study. _JAMA Otolaryngol. Head Neck Surg._ 148(4),
350 (2022). Article PubMed PubMed Central Google Scholar * Lim, H. _et al._ Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. _JAMA_ 317(13), 1338 (2017).
Article PubMed PubMed Central Google Scholar * Wu, J. _et al._ The epidemic of thyroid cancer in China: Current trends and future prediction. _Front. Oncol._ 12, 932729 (2022). Article
PubMed PubMed Central Google Scholar * Li, Y., Piao, J. & Li, M. Secular trends in the epidemiologic patterns of thyroid cancer in China over three decades: An updated systematic
analysis of global burden of disease study 2019 Data[J]. _Front. Endocrinol._ 12, 707233 (2021). Article Google Scholar * Feng, J.-W. _et al._ Determine the optimal extent of thyroidectomy
and lymphadenectomy for patients with papillary thyroid microcarcinoma. _Front. Endocrinol._ 10, 363 (2019). Article Google Scholar * Gharib, H. _Thyroid Nodules_ (Springer, Cham, 2018).
Book Google Scholar * Zhao, H. & Cui, L. Extent of surgery and the prognosis of unilateral papillary thyroid microcarcinoma. _Front. Endocrinol._ 12, 655608 (2021). Article Google
Scholar * Gartland, R. M. & Lubitz, C. C. Impact of extent of surgery on tumor recurrence and survival for papillary thyroid cancer patients. _Ann. Surg. Oncol._ 25(9), 2520–2525
(2018). Article PubMed Google Scholar * Nabhan, F., Dedhia, P. H. & Ringel, M. D. Thyroid cancer, recent advances in diagnosis and therapy. _Int. J. Cancer_ 149(5), 984–992 (2021).
Article CAS PubMed Google Scholar * Zhao, W. _et al._ Evaluating the effectiveness of prophylactic central neck dissection with total thyroidectomy for cN0 papillary thyroid carcinoma:
An updated meta-analysis. _Eur. J. Surg. Oncol._ 43(11), 1989–2000 (2017). Article PubMed Google Scholar * Ahn, S.-H. & Kim, W. S. The effect of prophylactic central neck dissection
during hemithyroidectomy on locoregional recurrence in patients with papillary thyroid carcinoma: A meta-analysis. _Clin. Exp. Otorhinolaryngol._ 13(2), 194–202 (2020). Article PubMed
PubMed Central Google Scholar * Russell, M. D., Kamani, D. & Randolph, G. W. Surgical management of the compromised recurrent laryngeal nerve in thyroid cancer. _Best Pract. Res. Clin.
Endocrinol. Metab._ 33(4), 101282 (2019). Article PubMed Google Scholar Download references ACKNOWLEDGEMENTS The authors thank Prof. Zhengrong Zheng and Prof. Feng Zheng for their
careful reading and useful comments. We would like to thank Editage (www.editage.cn) for English language editing. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Thyroid and
Breast Surgery, The Second Affiliated Hospital of Fujian Medical University, Quanzhou, 362000, Fujian Province, China Rujiao Lin, Sitao Huang, Shengnan Gao & Zhengrong Zheng * Department
of Neurosurgery, The Second Affiliated Hospital of Fujian Medical University, Quanzhou, 362000, Fujian Province, China Xiumei Guo & Feng Zheng * Department of Neurology, The Second
Affiliated Hospital of Fujian Medical University, Quanzhou, 362000, Fujian Province, China Xiumei Guo Authors * Rujiao Lin View author publications You can also search for this author
inPubMed Google Scholar * Sitao Huang View author publications You can also search for this author inPubMed Google Scholar * Xiumei Guo View author publications You can also search for this
author inPubMed Google Scholar * Shengnan Gao View author publications You can also search for this author inPubMed Google Scholar * Feng Zheng View author publications You can also search
for this author inPubMed Google Scholar * Zhengrong Zheng View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS Study conception and design, data
interpretation and reviewed the literature, Z.Z. Statistical analysis, study monitoring,and reviewed the literature, F.Z. Study conception, methodology, data acquisition, interpreted the
results and wrote the manuscript, R.L. Data acquisition, analysis and interpretation, S.H., X.G. and S.G. CORRESPONDING AUTHORS Correspondence to Feng Zheng or Zhengrong Zheng. ETHICS
DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims
in published maps and institutional affiliations. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits
use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the
Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless
indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory
regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Lin, R., Huang, S., Guo, X. _et al._ Impact of fellowship training for specialists
on thyroidectomy outcomes of patients with thyroid cancer. _Sci Rep_ 14, 9033 (2024). https://doi.org/10.1038/s41598-024-59864-0 Download citation * Received: 31 January 2024 * Accepted: 16
April 2024 * Published: 19 April 2024 * DOI: https://doi.org/10.1038/s41598-024-59864-0 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get
shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * Thyroid
cancer * Fellowship * Thyroid surgery * Prophylactic neck dissection * Postoperative complications * Impact







