- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) may be useful in treating exsanguinating trauma patients. This study seeks to compare rates of success,
complications and time required for vascular access between ultrasound-guidance and surgical cut-down for femoral sheath insertion as a prospective observational case control study.
Participating clinicians from either trauma surgery or anesthesiology were allocated to surgical cut-down or percutaneous ultrasound-guided puncture on a 1:1 ratio. Time spans to vessel
identification, successful puncture, and balloon inflation were recorded. 80 study participants were recruited and allocated to 40 open cut-down approaches and 40 percutaneous
ultrasound-guided approaches. REBOA catheter placement was successful in 18/40 cases (45%) using a percutaneous ultrasound guided technique and 33/40 times (83%) using the open cut-down
approach (_p_ < 0.001). Median times [in seconds] compared between percutaneous ultrasound-guided puncture and surgical cut-down were 36 (18–73) versus 117(56–213) for vessel
visualization (_p_ < 0.001), 136 (97–175) versus 183 (156–219) for vessel puncture (_p_ < 0.001), and 375 (240–600) versus 288 (244–379) for balloon inflation (_p_ = 0.08) overall.
Access to femoral vessels for REBOA catheter placement is safer when performed by cut-down and direct visualization but can be performed faster by an ultrasound-guided technique when vessels
can be identified clearly and rapidly. SIMILAR CONTENT BEING VIEWED BY OTHERS STANDARDIZED DISTANCES FOR PLACEMENT OF REBOA IN PATIENTS WITH AORTIC STENOSIS Article Open access 07 August
2020 USE OF A DISPOSABLE VASCULAR PRESSURE DEVICE TO GUIDE BALLOON INFLATION OF RESUSCITATIVE ENDOVASCULAR BALLOON OCCLUSION OF THE AORTA: A BENCH STUDY Article Open access 15 December 2021
APPLICATION OF PERCLOSE PROGLIDE CLOSURE DEVICE IN TRANSBRACHIAL ENDOVASCULAR INTERVENTION Article Open access 22 January 2025 INTRODUCTION Resuscitative Endovascular Balloon Occlusion of
the Aorta (REBOA) for exsanguinating patients is a comparably old intervention in medicine1. Advances in technology and consensus on the need for swift bleeding control in trauma
resuscitative care within the last decade have renewed clinical and scientific interest in the technique2,3. REBOA has been proven a useful adjunct in the resuscitative care of trauma
patients although there is distinct lack of evidence on the subject4,5. Complications after the use of REBOA have led to the conclusion that its use could even be detrimental6. Several
case-series report at least half of complications to be associated with femoral access for catheter placement7. Issues encompass complications at the site of access itself, ischemia due to
hampered limb perfusion, and inability to achieve access in a timely fashion8. The UK-REBOA Trial has been published recently and concerns about a possible increased mortality have been
raised, with the main concern that the procedure could delay definitive treatment9. To this day there is no clear evidence to guide clinicians on which technique for vascular access should
be preferred, to overcome this issue10. Possible techniques to achieve access to the femoral artery encompass landmark- and palpation-based vessel puncture, ultrasound-guided vessel
puncture, and surgical cut-down towards the femoral vessels. These approaches come with different prerequisites for providers’ skillsets and training and may be associated with different
rates of success and complications. Widespread availability of ultrasound and its superior safety profile over landmark-based blind palpation-only puncture, renders it the favorable method
nowadays for vascular access in critically ill in general11,12 and REBOA especially13. AIM OF THIS STUDY In this study, we primarily seek to compare the rates of success and complications
between ultrasound-guided femoral sheath insertion and surgical cut-down for sheath insertion in a close to (real) life model. Secondly, we aimed to elucidate, whether there are differences
between approaches in the time needed to achieve vascular access. METHODS STUDY DESIGN We designed a prospective observational case control study using a cadaveric training model using the
STROBE guideline14. The CACTUS guideline was used to ensure proper reporting of cadaver characteristics15. Participants were allocated to an open surgical cut-down approach or a percutaneous
ultrasound-guided approach to place the REBOA catheter on a 1:1 ratio. ETHICAL APPROVAL Approval from ethics committee at the Medical University Graz was sought and granted (34-247 ex
21/22) in accordance with the principles of the Declaration of Helsinki and the ICH-GCP Guidelines. PARTICIPANTS Study participants were physicians recruited from the University Medical
Centre Graz (Level-1-Trauma Centre). All participants were involved in the emergency management of major trauma patients either in the emergency department or in the prehospital setting.
Training of participants ranged from junior residents to senior attendings. Participants were recruited from medical specialties tasked with treatment of exsanguinating trauma patients in
our trauma system, i.e., Orthopedics and Trauma Surgery and Anesthesiology and Intensive Care Medicine (Table 1). Participant allocation to different procedure-groups was done based on
specialty: surgically trained personnel were designated to the open cut-down access, non-surgically trained personnel were allocated to the percutaneous ultrasound group. This group
allocation was chosen to assign participants the approach they would most likely be tasked with in our trauma resuscitation setting and in accordance with Austrian physician training
standards to ensure real- life conditions. Each participant was theoretically trained beforehand with lectures and simulation training, and got another on-site lecture on the task to be
performed and familiarization time with the equipment used, before starting the procedure (Table 1). SETTING AND CADAVER SPECIFICS For this study freshly cooled cadavers were used, storage
was between − 1 to + 6 °C until half an hour before the training. The investigated procedures on the cadavers were performed within 48 h after death. The procedure site was the dissecting
room at the Institute for Pathology at the Medical University Graz. 43 cadavers were used during the study period. Median (IQR) age of the deceased was 76 years (62–80) [minimum 29, maximum
85 years] years, median BMI was 27 (26–29) [minimum 19, maximum 39] kg/m2 with 16 cadavers having visual and tactile arterial calcification indicating severe peripheral artery disease.
(Table S1—Additional File 1) Cadavers with previous surgery to the inguinal region or devices placed in the femoral artery were not included in this study. During the procedure, only
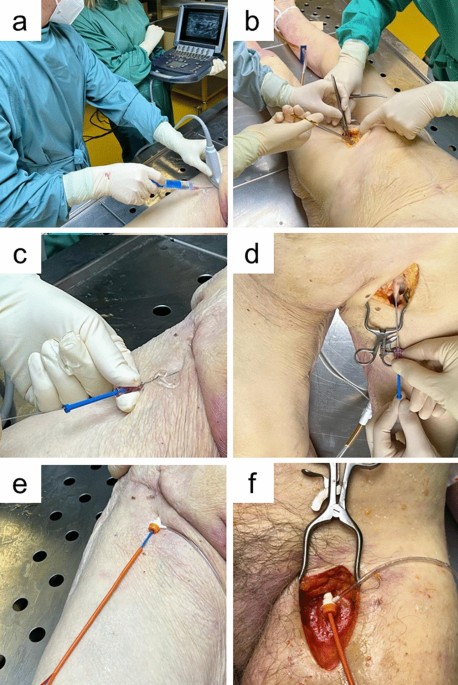
participants and investigators were present out of respect for the human body. PROCEDURE For the cut-down approach, participants were instructed to perform a longitudinal incision beginning
midway between the superior iliac spine and the pubic symphysis, extending over the medial border of the sartorius muscle, and proceeding toward the medial femoral epicondyle. After incision
of the subcutaneous tissue and fascia lata, the femoral sheath was incised to expose the vessels. The following instruments were used to implement the open cut-down approach: surgical
forceps, scalpel, wound distractors, surgical scissors. (Fig. 1). For the percutaneous ultrasound-guided approach, participants were instructed to identify the femoral vessels at the level
of the inguinal ligament with recommended puncture site below the inguinal ligament. For visualization and needle-guidance a 15–6 MHz linear probe and a SonoSite® M-Turbo Series ultrasound
machine was used. (Fig. 1). For both procedures, cannulation of the vessel was performed using a 7 French introducer sheath. For balloon occlusion of the aorta, ER-REBOA catheters (Prytime
Medical®, Boerne, TX, USA) were used and advanced 45-48cm into the vessel; balloon was then inflated with 8ml of water. Placement confirmation was achieved by direct visualization via
opening of the thoracic cavity. OUTCOMES Assessment of correct REBOA placement and any complications were recorded. Successful REBOA catheter placement was determined as balloon inflation in
the descending aorta between the left subclavian artery and the celiac trunk (zone 1). Time spans to identification of the intended target vessel, successful puncture and sheath
introduction, and balloon inflation were recorded. Timing was started after the lecture when handover of the materials to the participants was completed. STATISTICAL METHODS Data were
presented as absolute number (n) and percentage (%), or median and interquartile range (IQR), as appropriate. For main analyses, between-group differences in the outcomes of interest were
assessed by Chi-Square test or Mann–Whitney-U test, as appropriate; _p_-values below 0.05 were considered statistically significant. Time to balloon inflation was censored at 600 s. (i.e.,
10 min) in cases of unsuccessful placement attempts or incorrect catheter positioning. For secondary analyses, time spans elapsed were compared between groups in cases of successful correct
catheter placement only. For exploratory post-hoc analysis, differences in time consumed until vessel visualization and until sheath introduction were compared between successful and
unsuccessful attempts in the group with lower success rates. Vessel visualization was defined by participants’ impression having identified the correct vessel. If significant differences
were found, receiver operation curve (ROC) analysis was used to identify possible cut-off values to predict unsuccessful attempts. All analyses were performed using IBM SPSS Statistics 28.
RESULTS A total of 80 study participants were recruited and allocated to 40 open cut-down approaches and 40 percutaneous ultra-sound guided approaches. Information on successful puncture and
cannulation and documented time spans were available in all cases. Specifics of medical specialties and training status of the participants are given in Table1. MAIN ANALYSIS Successful
placement of the REBOA catheter was achieved in 18 out of 40 cases (45%) using a percutaneous ultrasound guided technique and 33 out of 40 times (83%) using the open cut-down approach (_p_
< 0.001) (Table 2). Median times compared between the percutaneous ultrasound-guided technique and the surgical cut-down approach were 36 (18–73) s versus 117(56–213)s for vessel
visualization (_p_ < 0.001), 136 s. (97–175) versus 183 s. (156–219) for vessel puncture (_p_ < 0.001), and 375 (240–600)s versus 288 (244–379) s for balloon inflation (_p_ = 0.08).
(Table 2). Time for actual REBOA catheter placement after vessel access, i.e., the timespan between vessel puncture and balloon inflation was not significantly different between the
ultrasound-guided technique [121 (82–174) s] and the cut-down approach [90 (61–132) s] (_p_ = 0.122). SECONDARY ANALYSES Median times in cases of correct REBOA catheter placement compared
between the percutaneous ultrasound-guided technique and the surgical cut-down approach were 18 (15–33) s versus 131 (95–165) s for vessel visualization (_p_ < 0.001), 58 (36–170) s
versus 178 (157–211) s for vessel puncture (_p_ < 0.001), and 226 (149–315) s versus 284 (233–359) s for balloon inflation (_p_ = 0.03) (Table 3). Successful REBOA catheter placement was
significantly more likely in the absence of arteriosclerosis [39 out of 53 (74%) vs. 12 out of 27 (44%), _p_ = 0.01], whereas absence of obesity was not associated with a significantly
higher success rate [34 out of 49 (69%) vs. 17 out of 31 (55%), _p_ = 0.187]. Reasons for unsuccessful placement of the REBOA catheter were impossibility of insertion due to peripheral
artery disease [6 out of 29 (21%)], vessel perforation and misplacement during puncture [7 out of 29 (24%)], venous puncture and insertion into inferior vena cava [6 out of 29 (21%)], or not
identifiable vessel [10 out of 29 (34%)]. EXPLORATORY ANALYSES Within the group of percutaneous ultrasound-guided attempts, median times for successful and unsuccessful attempts were 18
(15–33) s versus 53 (35–87) s (_p_ < 0.001) for vessel visualization and 58 (36–170) s versus 155 (89–236) sec. for vessel puncture (p = 0.08), respectively. (Figure S1 and S2—Additional
File 1). ROC analyses yielded best results for time to vessel visualization at 23 s. (sensitivity 0.91, specificity 0.67, AUC 0.83) and 90 s. (sensitivity 0.77, specificity 0.61, AUC 0.74)
for time to vessel puncture, respectively. (Figure S3—Additional File 1). DISCUSSION In this prospective observational case control study using a cadaveric training model, ultrasound-guided
puncture and surgical cut-down of femoral vessels demonstrate significant differences in success rates and time spent for REBOA catheter placement. Success rate for REBOA placement is nearly
twice as high using a cut-down approach compared to the ultrasound-guided technique. This might lead to the conclusion that this technique was the superior approach. However, when comparing
times consumed, the ultrasound-guided approach compared to the cut-down approach requires significantly less time until balloon inflation, allowing for faster bleeding control and potential
of hemodynamic benefit. REBOA can be a life-saving procedure in exsanguinating trauma patients16. Broad consensus now underlines its role in the management of trauma resuscitation17.
However, despite more than 600 publications on the subject, high-quality evidence concerning indications, complications, and outcomes is still lacking. The potential benefit of REBOA in
trauma patients can be limited by complications as well as the elapsed time for catheter placement8,18. On a procedural level, the rate limiting step in placement has been shown to be timing
and safety for femoral artery access8. To our knowledge, this is the first study conducted in order to elucidate profiles of different techniques in femoral vessel access for REBOA catheter
placement. Our results show that clear and prompt identification of the targeted femoral artery are crucial for safe and timely access to femoral vessels for REBOA placement, with both
techniques proving different advantages. Ultrasound-guided placement of different lines for vascular access, both arterial and venous, are nowadays deemed standard of care in critical ill
and emergency patients12. As patients with severe bleeding after trauma can deteriorate rapidly and placement of those lines gets more difficult over time, early access is crucial8,19. Our
study data, in line with other reports, show that if vessels can be identified on ultrasonography vascular access can be established within 2.5 min, but failure to identify the correct
vessel was the main reason for complications in more than half of cases. Furthermore, our data show that attempts for clear vessel identification using ultrasonography of approximately half
a minute or more are predictive of the inability to place the REBOA catheter correctly using ultra-sound guided technique. The DIRECT-IABO investigators report time to access to be directly
associated with survival for patients undergoing REBOA20. If first line placement of a 7 French vascular sheath or a smaller device for arterial pressure monitoring (allowing for the
possibility of using Seldinger’s technique to introduce a larger sheath at a later stage) should be used, is yet to be determined. We thus suggest that arterial access should be obtained
early during treatment of patients with potential benefit of REBOA, in order to prevent harm from complications and unnecessary time-consuming attempts once patients collapse and safe
sonographic vessel visualization becomes more unlikely. Crally et al. have come to the same conclusion in their study, by identifying the time to catheter placement as a crucial step for
improving outcome for this procedure21. If patients already present in extremis, rendering visualization via ultrasonography uncertain within a timely fashion, a cut down approach to the
femoral vessels should be performed. This conclusion is in line with other reports stating that if cardiac arrest is present or imminent cut down may be safer for femoral access22. Notably,
resuscitative thoracotomy and aortic cross-clamping remain possible options in these patients. However, no clear evidence is available to prefer one method over the other4. Furthermore, the
conversion from open aortic cross-clamping to REBOA may be an option in certain circumstances if providers’ training and expertise allow23. Biological age and premorbid status have to be
taken into account when considering different approaches to femoral vessel access. Peripheral Artery Disease, prior surgery or treatment in the anatomical area of interest may be more
prevalent in older individuals. The investigated cadavers in this study, with a median age of 76 years, may overrepresent this age group, potentially skewing results towards one approach.
This may limit generalizability and applicability to certain patients, since on the one hand, trauma and especially exsanguination is the most imminent threat to life in adults younger than
49 years24. On the other hand, due to demographic changes, the age of severely injured patients is steadily increasing25 and thus the investigated cadavers and their specifics regarding age
related comorbidities may represent emerging challenges in trauma care. Because of the high failure rate of ultrasound-guided techniques for REBOA catheter placement demonstrated by our
study as well as previous studies8, we suggest practitioners, regardless of medical specialty, should be trained in both techniques when centers aim to perform REBOA during treatment of
exsanguinating trauma patients. This conclusion is in line with previous studies trying to elucidate which medical specialty should be performing REBOA catheter placement, which have been
unable to produce clear recommendations, but emphasize proper training26. LIMITATIONS This study was conducted in a cadaveric training model with its known downside of not reflecting
conditions in a living human being reliably, especially the absence of pulsations and missing backflow. Since we only used freshly cooled cadavers it still seems reasonable to translate
results to some extent into real-life, as patients in severe shock after major blood loss and patients with traumatic cardiac arrest are considered prime candidates for REBOA catheter
placement. Another downside was that the cadavers presented with a high rate of arteriosclerosis, a condition not usually present in the young exsanguinating trauma patient. With a rising
number of trauma amongst the elderly and demographic changes, these findings still need considering and further research should address this topic as well. Missing arterial pulsation and
vasculature tone might have been unrealistic conditions leading to difficulties in vessel identification, especially for the ultrasound-guided technique. Anyhow, in comparison to embalmed
bodies, fresh cadavers offer a genuine tissue handling and a variety of anatomic and pathologic variations. Another limitation of this study was the lack of cross-over design for different
medical specialties performing different techniques. Basic familiarity with the equipment used could have been a bias both in timing and accuracy, rendering medical specialty training a
remaining potential for bias in our analyses. CONCLUSION Our study shows that access to the femoral vessels for REBOA catheter placement in a resuscitation scenario is safer when performed
by cut-down and direct visualization but can be performed faster by an ultrasound-guided technique when vessels can be identified clearly and rapidly. DATA AVAILABILITY The datasets used and
analyzed are attached in table form to this submission. ABBREVIATIONS * AUC: Area under the curve * BMI: Body mass index * IQR: Interquartile range * REBOA: Resuscitative endovascular
balloon occlusion of the aorta * ROC: Receiver operating characteristics REFERENCES * Hughes, C. W. Use of an intra-aortic balloon catheter tamponade for controlling intra-abdominal
hemorrhage in man. _Surgery_ 36, 65–68 (1954). CAS PubMed Google Scholar * Ordoñez, C. A. _et al._ Damage control resuscitation: REBOA as the new fourth pillar. _Colomb. Med. (Cali.)_ 51,
1–12 (2020). Google Scholar * Biffl, W. L., Fox, C. J. & Moore, E. E. The role of REBOA in the control of exsanguinating torso hemorrhage. _J. Trauma Acute Care Surg._ 78, 1054–1058
(2015). Article PubMed Google Scholar * Cralley, A. L. _et al._ Zone 1 endovascular balloon occlusion of the aorta vs resuscitative thoracotomy for patient resuscitation after severe
hemorrhagic shock. _JAMA Surg._ https://doi.org/10.1001/JAMASURG.2022.6393 (2022). Article PubMed Central Google Scholar * Castellini, G. _et al._ Resuscitative endovascular balloon
occlusion of the aorta (REBOA) in patients with major trauma and uncontrolled haemorrhagic shock: A systematic review with meta-analysis. _World J. Emerg. Surg._
https://doi.org/10.1186/S13017-021-00386-9 (2021). Article PubMed PubMed Central Google Scholar * Joseph, B. _et al._ Nationwide analysis of resuscitative endovascular balloon occlusion
of the aorta in civilian trauma. _JAMA Surg._ 154, 500 (2019). Article PubMed PubMed Central Google Scholar * Ribeiro Junior, M. A. F. _et al._ The complications associated with
resuscitative endovascular balloon occlusion of the aorta (REBOA). _World J. Emerg. Surg._ https://doi.org/10.1186/S13017-018-0181-6 (2018). Article PubMed PubMed Central Google Scholar
* Romagnoli, A. _et al._ Time to aortic occlusion: It’s all about access. _J. Trauma Acute Care Surg._ 83, 1161–1164 (2017). Article PubMed Google Scholar * Jansen, J. O. _et al._
Emergency department resuscitative endovascular balloon occlusion of the aorta in trauma patients with exsanguinating hemorrhage: The UK-REBOA randomized clinical trial. _JAMA_
https://doi.org/10.1001/JAMA.2023.20850 (2023). Article PubMed PubMed Central Google Scholar * Davidson, A. J. _et al._ The pitfalls of resuscitative endovascular balloon occlusion of
the aorta: Risk factors and mitigation strategies. _J. Trauma Acute Care Surg._ 84, 192–202 (2018). Article PubMed Google Scholar * Balceniuk, M. D. _et al._ Regional variation in usage
of ultrasound-guided femoral access in the vascular quality initiative. _Ann. Vasc. Surg._ 72, 544–551 (2021). Article PubMed Google Scholar * Schmidt, G. A. _et al._ Ultrasound-guided
vascular access in critical illness. _Intens. Care Med._ 45, 434–446 (2019). Article CAS Google Scholar * Reva, V. A. _et al._ Ultrasound-guided versus blind vascular access followed by
REBOA on board of a medical helicopter in a hemorrhagic ovine model. _Injury_ 52, 175–181 (2021). Article PubMed Google Scholar * Von Elm, E. _et al._ The strengthening the reporting of
observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. _Epidemiology_ 18, 800–804 (2007). Article Google Scholar * Mantica, G. _et al._
Reporting characteristics of cadaver training and surgical studies: The CACTUS guidelines. _Int. J. Surg._ 101, 106619. https://doi.org/10.1016/J.IJSU.2022.106619 (2022). Article PubMed
Google Scholar * du Bose, J. J. _et al._ The AAST prospective aortic occlusion for resuscitation in trauma and acute care surgery (AORTA) registry: Data on contemporary utilization and
outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). _J. Trauma Acute Care Surg._ 81, 409–419 (2016). Article Google Scholar * Maiga, A. W. _et al._
Systematic review to evaluate algorithms for REBOA use in trauma and identify a consensus for patient selection. _Trauma Surg. Acute Care Open_ 7, e000984 (2022). Article PubMed PubMed
Central Google Scholar * Laverty, R. B. _et al._ Life over limb: Arterial access-related limb ischemic complications in 48-hour REBOA survivors. _J. Trauma Acute Care Surg._ 92, 723–728
(2022). Article PubMed Google Scholar * Hörer, T. Resuscitative endovascular balloon occlusion of the aorta (REBOA) and endovascular resuscitation and trauma management (EVTM): A paradigm
shift regarding hemodynamic instability. _Eur. J. Trauma Emerg. Surg._ 44, 487–489 (2018). Article PubMed Google Scholar * Matsumura, Y. _et al._ Early arterial access for resuscitative
endovascular balloon occlusion of the aorta is related to survival outcome in trauma. _J. Trauma Acute Care Surg._ 85, 507–511 (2018). Article PubMed Google Scholar * Cralley, A. L. _et
al._ Predicting success of resuscitative endovascular occlusion of the aorta: Timing supersedes variable techniques in predicting patient survival. _J. Trauma Acute Care Surg._ 91, 473–479
(2021). Article PubMed Google Scholar * Low, R. B., Longmore, W., Rubinstein, R., Flores, L. & Wolvek, S. Preliminary report on the use of the percluder® occluding aortic balloon in
human beings. _Ann. Emerg. Med._ 15, 1466–1469 (1986). Article CAS PubMed Google Scholar * Matsumura, Y., Matsumoto, J., Kondo, H., Idoguchi, K. & Funabiki, T. Partial occlusion,
conversion from thoracotomy, undelayed but shorter occlusion: Resuscitative endovascular balloon occlusion of the aorta strategy in Japan. _Eur. J. Emerg. Med._ 25, 348–354 (2018). Article
PubMed Google Scholar * Global health estimates: Leading causes of death. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death
(Accessed 23 May2023). * Pfeifer, R., Teuben, M., Andruszkow, H., Barkatali, B. M. & Pape, H. C. Mortality patterns in patients with multiple trauma: A systematic review of autopsy
studies. _PLoS One_ 11, e0148844 (2016). Article PubMed PubMed Central Google Scholar * Hilbert-Carius, P. _et al._ Successfully REBOA performance: Does medical specialty matter?
International data from the ABOTrauma Registry. _World J. Emerg. Surg._ https://doi.org/10.1186/S13017-020-00342-Z (2020). Article PubMed PubMed Central Google Scholar Download
references ACKNOWLEDGEMENTS We want to thank the assistant prosector team of the Institute for Pathology at the Medical University of Graz and all the participating doctors. AUTHOR
INFORMATION AUTHORS AND AFFILIATIONS * Department of Orthopedics and Trauma Surgery, Medical University of Graz, Graz, Austria Peter Grechenig, Nicolas Rene Eibinger, Amir Koutp & Paul
Puchwein * Department of Anaesthesiology and Intensive Care Medicine, Medical University Graz, Auenbruggerplatz 5, 8036, Graz, Austria Barbara Hallmann & Paul Zajic * Diagnostic and
Research Institute of Pathology, Medical University Graz, Graz, Austria Gerald Höfler Authors * Peter Grechenig View author publications You can also search for this author inPubMed Google
Scholar * Barbara Hallmann View author publications You can also search for this author inPubMed Google Scholar * Nicolas Rene Eibinger View author publications You can also search for this
author inPubMed Google Scholar * Amir Koutp View author publications You can also search for this author inPubMed Google Scholar * Paul Zajic View author publications You can also search for
this author inPubMed Google Scholar * Gerald Höfler View author publications You can also search for this author inPubMed Google Scholar * Paul Puchwein View author publications You can
also search for this author inPubMed Google Scholar CONTRIBUTIONS P.G.: Conceptualization, Investigation, Data Curation, Writing—Original, Project administration; P.P.: Conceptualization,
Validation, Investigation, Writing—Review & Editing, Supervision, Project administration; N.R.E.: Investigation, Writing—Review & Editing; A.K.: Investigation, Writing—Review &
Editing; P.Z.: Methodology, Formal analysis, Data Curation, Writing—Review & Editing, Visualization; G.H.: Investigation, Resources, Writing—Review & Editing, Supervision; B.H.:
Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data Curation, Writing—Original, Project administration. CORRESPONDING AUTHOR Correspondence to Barbara Hallmann.
ETHICS DECLARATIONS COMPETING INTERESTS _PP_ received a training device unrelated to this study from Prytime Medical®, the manufacturer of the ER-REBOA catheter used in this study, free of
charge. All the authors declare that they have no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in
published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons
Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original
author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the
article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your
intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence,
visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Grechenig, P., Hallmann, B., Eibinger, N.R. _et al._ Percutaneous
ultrasound-guided versus open cut-down access to femoral vessels for the placement of a REBOA catheter. _Sci Rep_ 14, 9111 (2024). https://doi.org/10.1038/s41598-024-59778-x Download
citation * Received: 02 November 2023 * Accepted: 15 April 2024 * Published: 20 April 2024 * DOI: https://doi.org/10.1038/s41598-024-59778-x SHARE THIS ARTICLE Anyone you share the following
link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature
SharedIt content-sharing initiative




.jpg?w=1200&ar=40%3A21&auto=format%2Ccompress&ogImage=true&mode=crop&enlarge=true&overlay=false&overlay_position=bottom&overlay_width=100)

