- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT To determine the number of patients with acute respiratory distress syndrome (ARDS) who would be eligible to receive veno-venous extracorporeal membrane oxygenation (VV-ECMO). We
conducted a retrospective observational study of ARDS patients admitted to Regina General Hospital Intensive Care Unit (ICU). VV-ECMO eligibility was assessed using selection criteria from
the Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Syndrome trial (EOLIA), the Extracorporeal Life Support Organization (ELSO), New South Wales (NSW), Critical Care
Services Ontario (CCSO) and a Regina-restrictive criteria. Of 415 patients admitted between October 16, 2018, and January 21, 2021, 103 (25%) had mild, 175 (42%) had moderate, and 64 (15%)
had severe ARDS. Of the cohort, 144 (35%) had bacterial pneumonia, 86 (21%) had viral pneumonia (including COVID-19), and 72 (17%) had aspiration pneumonia. Using the EOLIA, ELSO, NSW, CCSO
and Regina-restrictive criteria, 7/415 (1.7%), 6/415 (1.5%), 19/415 (4.6%), 26/415 (6.3%) and 12/415 (2.9%) were eligible for VV-ECMO, respectively. Of all ECMO-eligible patients, only one
(2.4%) actually received VV-ECMO, 20/42 (48%) received prone positioning and 21/42 (50%) received neuromuscular blockade. There is potential for service expansion of VV-ECMO in Regina;
however, there is still a need to improve the delivery of evidence-based ARDS therapies. SIMILAR CONTENT BEING VIEWED BY OTHERS TREND OF EXTRACORPOREAL MEMBRANE OXYGENATION SUPPORT IN
PATIENTS WITH ACUTE RESPIRATORY DISTRESS SYNDROME IN SOUTH KOREA Article Open access 28 March 2022 ECMO IS ASSOCIATED WITH DECREASED HOSPITAL MORTALITY IN COVID-19 ARDS Article Open access
27 June 2024 EXTRACORPOREAL MEMBRANE OXYGENATION AND ACUTE KIDNEY INJURY: A SINGLE-CENTER RETROSPECTIVE COHORT Article Open access 13 September 2023 INTRODUCTION Acute respiratory distress
syndrome (ARDS) is an inflammatory syndrome1, which develops under several clinical conditions such as bacterial and viral pneumonia, including coronavirus-2019 disease (COVID-19)2. In an
international prospective study, LUNG SAFE, 10% of all admissions to the intensive care unit (ICU) had ARDS, with a hospital mortality of 40%3. Common ventilation strategies and adjunctive
therapies for ARDS include low tidal volume ventilation, optimizing positive end expiratory pressure (PEEP), prone positioning, neuromuscular blockade, and inhaled nitric oxide (iNO).
Recently, veno-venous extracorporeal membrane oxygenation (VV-ECMO) has been used as a rescue strategy for severe ARDS, based on a number of clinical trials and subsequent
meta-analyses4,5,6,7. In an individual patient data meta-analysis of patients with severe ARDS, patients treated with VV-ECMO were found to have a relative risk of 0.75 (95% CI, 0.6–0.94)
for 90-day mortality, compared to patients who did not receive VV-ECMO5. Consequently, the use of VV-ECMO for severe ARDS has been on the rise worldwide, and particularly with the recent
COVID-19 pandemic8. In fact, in an international cohort study of the Extracorporeal Life Support Oxygenation (ELSO) registry, 1035 COVID-19 patients were supported with ECMO in 36 countries
between January and May of 20209. Due to an increase in ECMO demand during the COVID-19 pandemic, an ECMO working group was formed at our hospital. Previously, we had assessed potential need
for extracorporeal cardiopulmonary resuscitation need at our centre10. As such, the purpose of the study was to assess potential VV-ECMO volume in Regina, Saskatchewan to allow for program
planning and improve patient outcomes. METHODS STUDY DESIGN AND SETTING A retrospective observational study was conducted of consecutive ICU admissions with ARDS at Regina General Hospital
(RGH) from October 16, 2018, to January 21, 2021. RGH is a tertiary care university-affiliated teaching hospital which can provide both VV- and veno-arterial (VA)-ECMO on an ad hoc basis.
The hospital is a major referral centre in Southern Saskatchewan, serving about 500,000 residents in an area11 over 100,000 km2. RGH has a standard ventilation protocol with most patients
receiving pressure-regulated volume control as the initial set mode, with a set tidal volume of 6–8 mL/kg predicted body weight, while maintaining the peak inspiratory pressure (PIP) ≤ 35 cm
H2O and plateau pressure ≤ 30 cm H2O. PEEP may be set by static compliance measurements and/or esophageal pressure manometry. PARTICIPANTS Patients were included if they met the following
criteria: ≥ 18 years of age, received mechanical ventilation, and were diagnosed with ARDS based on the Berlin definition1. Patients who experienced respiratory failure primarily due to
congestive heart failure were excluded. COVARIATES Demographic and clinical information were collected, including age, biological sex, height, weight, comorbidities, oxygenation and
ventilation parameters, use of adjunctive therapies, and information related to the potential contraindications such as severe bleeding, cardiac arrest prior to ECMO, severe
immunosuppression, and poor neurological prognosis. Largest set and actual delivered tidal volumes (in mL) on the first day of mechanical ventilation were determined from tidal volume and
spontaneous tidal volume measurements. The Charlson comorbidity index (CCI) and sequential organ failure assessment (SOFA) score were determined based on collected data12,13. We categorized
patients into mild, moderate and severe ARDS based on the Berlin definition of ARDS1 (Table 1). Data was stored in a secure REDCap (Vanderbilt University, United States) database.
VENO-VENOUS EXTRACORPOREAL MEMBRANE OXYGENATION SELECTION CRITERIA VV-ECMO eligibility was assessed using pre-defined selection criteria and contraindications that were derived from existing
literature. The final criteria chosen included criteria from the Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Syndrome (EOLIA) trial, ELSO, New South Wales (NSW), and
CCSO (Table S2, Supplementary Appendix)7,14,15,16. The EOLIA trial is a well-known international randomized control trial of VV-ECMO in patients with severe ARDS7. The ELSO has previously
published guidelines on ECMO management for COVID-1914. The more restrictive COVID-19 criteria were chosen over the more recent ELSO criteria as this study had taken place during the
COVID-19 pandemic prior to the publication of the more recent criteria17. CCSO is a Canadian provincial body that has previously published referral criteria for ECMO provision16. The NSW
criteria was chosen to represent criteria from another country from a well-established ECMO program15. The eligibility under each criterion was determined according to indications and only
absolute contraindications (not relative contraindications). We assessed patients between days 1–14 of mechanical ventilation. A final ECMO criteria was created specific to RGH
(Regina-restrictive) based on an internal modified Delphi study. Additional details pertaining to the Delphi study can be found in the Supplementary Appendix. OUTCOMES The primary outcome
was the number of patients that were ECMO-eligible and ECMO-ineligible based on the five different criteria during the study period. Secondary outcomes included in-hospital mortality, length
of stay, and utilization of ventilation strategies and adjunctive therapies. STATISTICAL ANALYSIS All statistical analyses were conducted on Stata 17 (StataCorp, United States). Simple
statistics were reported as frequency counts and percentages, means with standard deviations or medians with interquartile range (IQR) depending on the distribution of data. Normality
testing was performed using the Shapiro–Wilk test. To compare proportions between eligible and non-eligible groups, χ2 squared or Fisher’s exact tests (for groups less than 10 counts) were
used for categorical variables. _T_ test or Wilcoxon rank sum tests were utilized for continuous variables depending on normality of data. To compare continuous variables between two or more
groups, one-way ANOVA or Kruskal–Wallis H test were utilized also depending on normality. ETHICS APPROVAL AND CONSENT TO PARTICIPATE The Research Ethics Board (REB) of the former
Saskatchewan Health Authority had approved the study involving retrospective chart reviews (REB-21-17). A waiver of informed consent was obtained from the Saskatchewan Health Authority
Research Ethics Board (REB-21-17). The University of Saskatchewan Behavioral Research Ethics Board approved the modified Delphi study and provided a certificate of approval (Beh-REB-2825).
All research methods were carried out in accordance with the Health Information Protection Act (HIPA), the Tri-Council Policy Statement (TCPS 2) and the McMaster Chart Review Research
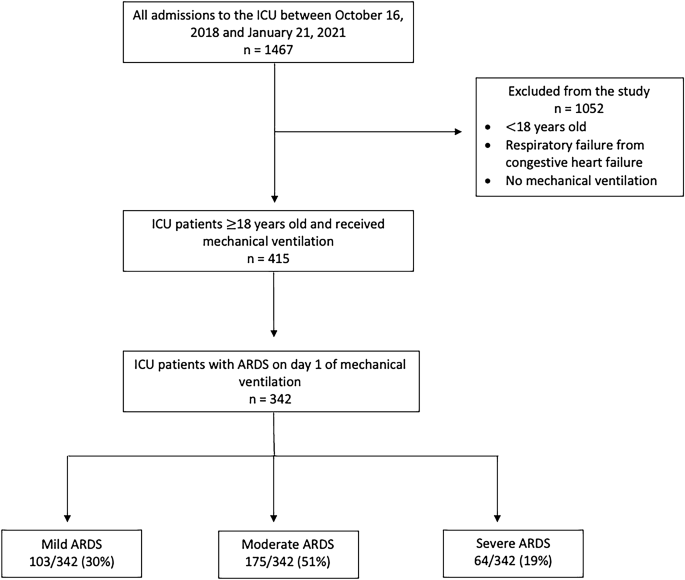
Ethics. RESULTS FULL STUDY COHORT CHARACTERISTICS Out of 1467 patients admitted to the RGH ICU, 415 patients were included in this study (Fig. 1). Of the 415 consecutive patients with ARDS,
165 (40%) patients were female, 144 (35%) had bacterial pneumonia, 86 (21%) had viral pneumonia (including COVID-19), 72 (17%) had aspiration pneumonia, 27 (6.5%) had trauma- or burn-related
ARDS, 55 (13%) had other respiratory diagnoses and 30 (7.2%) had non-respiratory or chronic respiratory diagnoses. Forty-eight (12%) patients had COVID-19. According to the observed
ventilator settings on day one of mechanical ventilation, patients received a median highest set tidal volume of 7.8 mL/kg (IQR 7.2–8.3), a median highest actual delivered tidal volume of
8.5 mL/kg (IQR 7.8–9.7), and a median PEEP of 10 cmH2O (IQR 8–14). In-hospital mortality occurred in 136/415 (33%) patients (Table 2). In the study, 342/415 (82%) patients met clinical
parameters of ARDS by day one of mechanical ventilation. ASSESSMENT OF ECMO ELIGIBILITY AND ASSOCIATED CHARACTERISTICS In this study, 42/415 (10%) patients were potentially eligible to
receive VV-ECMO between all criteria. Between the five different criteria, 7/415 (1.7%), 6/415 (1.5%), 19/415 (4.6%), 26/415 (6.3%) and 12/415 (2.9%) patients were eligible for VV-ECMO,
using the EOLIA, ELSO, NSW, CCSO and Regina-restrictive criteria, respectively (Table 3). Of all ECMO-eligible patients, only 1/42 (2.4%) patient received VV-ECMO and had met only the CCSO
criteria for ECMO. Of all ECMO-eligible patients, 19/42 (45%) patients developed severe ARDS (Table 1). Further, a significantly large proportion of patients eligible for ECMO were males
(79%) compared to non-eligible group (58%, p-value = 0.01). In terms of use of adjunctive therapies, 20/42 (48%) received prone positioning, 21/42 (50%) received neuromuscular blockade and
5/42 (12%) received iNO (Table S4, Supplementary Appendix). Among all patients, there were 48 patients with COVID-19, of which seven (14.6%) were eligible for VV-ECMO, compared to 35 (9.5%)
of patients who did not have COVID-19 (p = 0.30) (Table S5, Supplementary Appendix). OUTCOMES OF ECMO-ELIGIBLE PATIENTS Although 279/415 (62%) of all patients survived to hospital discharge,
only 1/7 (14%), 1/6 (17%), 7/19 (37%), 12/26 (46%), 4/12 (33%) patients, who met the EOLIA, ELSO, NSW, CCSO and Regina-restrictive criteria respectively, survived to hospital discharge. For
all ECMO-eligible patients, in-hospital mortality was 54% (23/42) and the hospital length of stay was a median of 17 days (IQR 8–25). Additional results can be found in the Supplementary
Appendix. DISCUSSION In this study, we used several different criteria varying in their level of stringency to evaluate potential ECMO need in our centre. Approximately six (1.5%) to 26
(6.3%) patients were eligible for VV-ECMO over a duration of 2.3 years at our centre, but only one patient received treatment with ECMO during that period. Thus, the estimated VV-ECMO volume
at RGH could range from at least three to eleven cases of VV-ECMO per year. The estimated incidence of VV-ECMO use for ARDS would be 0.6 to 2.2 cases per 100,000 population per year (based
on RGH’s catchment of approximately 500,000 residents)11. Statistics Canada forecasts a 14.3% to 43.8% growth in the population of Saskatchewan in the next 20 years18. With a potential rise
in RGH’s catchment of 570,000 to 720,000 residents, an incidence of 0.7 to 3.2 cases per 100,000 population per year could be expected for VV-ECMO use for ARDS in 20 years. We did attempt to
distinguish between the need for ECMO among patients that had COVID-19 compared to patients that did not. Even if we were to exclude patients with COVID-19, we would expect around 0.3 to
1.8 cases of ECMO per 100,000 population per year. While it is difficult to predict when the next pandemic may occur, it is likely that a future pandemic may increase ECMO demand. As such,
an increase in local ECMO volume for patients with severe ARDS could be anticipated. For this to occur, human resources and resource allocation (i.e., trained perfusionists) would need to be
assessed at RGH. Although ECMO services may be increased in Regina, Saskatchewan, current ECMO volume may be insufficient to maintain significant expertise (not withstanding additional
patients who may be receiving VA-ECMO for cardiogenic shock and/or extracorporeal cardiopulmonary resuscitation). In a prior study, higher annual adult ECMO centre volume was associated with
lower mortality19. Previously, it has been suggested that centres should maintain an ECMO volume of at least 12 to 20 cases per year to optimize outcomes and maintain expertise19. However,
recent evidence during the COVID-19 pandemic would suggest that newly formed ECMO centres may have acceptable outcomes when supervised in conjunction with an experienced centre20. In Japan,
the Tokyo Medical and Dental University Hospital performs only 5 to 10 VV-ECMO cases per year, yet they were able to achieve a high survival rate with a multidisciplinary team approach21.
Therefore, there are several potential solutions including centralization of ECMO services in Saskatchewan to one tertiary care site and/or partnership with other provincial ECMO programs
(i.e., Alberta Health Services and/or Manitoba Health). However, geographic, climate, and jurisdictional considerations in Saskatchewan limit the ability to transport unstable patients over
large distances and likely justify the current situation of two ECMO referral centres in Saskatchewan. COMPARISON TO OTHER STUDIES Around the world, there are differences in the predicted
incidence of VV-ECMO. The annual rates of VV-ECMO use for ARDS varied from 0.5 to 1 per 100,000 population in France22, 2.4 per 100,000 in Germany23, and 9.8 per 100,000 in South Korea8.
Thus, at around three to eleven cases of VV-ECMO per year, our centre would have comparable incidence of VV-ECMO per population. When comparing ARDS outcomes to other studies, the
in-hospital mortality of VV-ECMO-eligible patients in our study (55%) was higher compared to ARDS patients in the VV-ECMO arm of the EOLIA trial (36%)7. For reference, mortality in the
control group of the EOLIA trial was 57% despite a 28% crossover to ECMO7. This result is unsurprising given the subsequent Bayesian re-analysis and meta-analyses demonstrating benefit to
VV-ECMO use. However, this emphasizes a potential need to improve VV-ECMO access at our institution. On the other hand, there was low adherence to evidence-based ARDS therapies in our
cohort, including low tidal volume ventilation, prone positioning, and neuromuscular blockade. Consequently, ECMO needs could be overestimated if these therapies were instituted routinely.
For comparison to other ECMO-eligible patients in our study, ARDS patients participating in the EOLIA trial had lower tidal volume (mean 6.0 mL/kg in EOLIA trial versus median 8.4 mL/kg in
our study), higher use of prone positioning (56% versus 48% in our cohort), higher use of iNO (51% versus 12%), and higher use of neuromuscular blockade (92% versus 50%)7. FUTURE DIRECTIONS
Our study has important findings and implications for local quality improvement. This may include interventions to improve recognition of ARDS, improve adherence to evidence-based ARDS
therapies, educate staff, develop local treatment guidelines, and streamline the referral process for VV-ECMO. In an observational before and after study, the implementation of an ARDS
protocol reduced patient mortality by 12%, improved clinician recognition of ARDS, improved the detection of unsafe tidal volumes and airway pressures, and increased the use of ventilation
strategies24. LIMITATIONS Our study has limitations. First, we did not collect information on driving pressure, measures of respiratory effort such as P0.1 or airway occlusion pressure, or
other measures of lung stress and strain, as these criterion had not previously been included in previously published ECMO inclusion or exclusion criterion25. Second, the retrospective
nature of the study makes it difficult to accurately assess for contraindications, as they may not have been charted adequately and clinician judgement may also have played a role. Third, as
there was only one patient who received ECMO in our cohort, patient outcomes of ECMO treatment could not be studied. Finally, as this is a single centre study, our findings may not
necessarily apply to other centres. CONCLUSION There may be potential need for expansion of VV-ECMO services in Saskatchewan. However, the use of low tidal volume ventilation, prone
positioning, and neuromuscular blockade in patients with severe ARDS could be optimized through quality improvement, staff education, and protocolized care. DATA AVAILABILITY The data that
support the findings of this study may be available on request from the corresponding author and written permission from the Saskatchewan Health Authority. The data are not publicly
available due to privacy and confidentiality restrictions from the Saskatchewan Health Authority. ABBREVIATIONS * ARDS: Acute respiratory distress syndrome * ICU: Intensive care unit * PEEP:
Positive end expiratory pressure * iNO: Inhaled nitric oxide * FiO2 : Fraction of inspired oxygen * PaO2 : Partial pressure of oxygen * PIP: Peak inspiratory pressure * VV-ECMO: Veno-venous
extracorporeal membrane oxygenation * VA-ECMO: Veno-arterial extracorporeal membrane oxygenation * RGH: Regina General Hospital * SOFA: Sequential organ failure assessment * CCI: Charlson
Comorbidity Index * EOLIA: Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Syndrome * ELSO: Extracorporeal Life Support Organization * CCSO: Critical Care Services Ontario *
CESAR: Conventional Ventilatory Support VS Extracorporeal Membrane Oxygenation for Severe Adult Respiratory Failure * IQR: Interquartile range REFERENCES * Ranieri, V. M. _et al._ Acute
respiratory distress syndrome: The Berlin Definition. _JAMA J. Am. Med. Assoc._ 307(23), 2526–2533 (2012). Google Scholar * Huppert, L. A., Matthay, M. A. & Ware, L. B. Pathogenesis of
acute respiratory distress syndrome. _Semin. Respir. Crit. Care Med._ 40(1), 31–39 (2019). Article PubMed PubMed Central Google Scholar * Bellani, G. _et al._ Epidemiology, patterns of
care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. _JAMA_ 315(8), 788–800 (2016). Article CAS PubMed Google Scholar *
Munshi, L. _et al._ Venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome: A systematic review and meta-analysis. _Lancet Respir. Med._ 7(2), 163–172 (2019).
Article PubMed Google Scholar * Combes, A. _et al._ ECMO for severe ARDS: Systematic review and individual patient data meta-analysis. _Intensive Care Med._ 46(11), 2048–2057 (2020).
Article CAS PubMed PubMed Central Google Scholar * Peek, G. J. _et al._ CESAR: Conventional ventilatory support vs extracorporeal membrane oxygenation for severe adult respiratory
failure. _BMC Health Serv. Res._ 23(6), 163 (2006). Article Google Scholar * Combes, A. _et al._ Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. _N.
Engl. J. Med._ 378(21), 1965–1975 (2018). Article PubMed Google Scholar * Cho, H. W., Song, I. A. & Oh, T. K. Trends in extracorporeal membrane oxygenation treatment from 2005 to 2018
in South Korea. _Perfusion_ 20, 02676591211018130 (2021). Google Scholar * Barbaro, R. P. _et al._ Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of
the Extracorporeal Life Support Organization registry. _Lancet_ 396(10257), 1071–1078 (2020). Article CAS PubMed PubMed Central Google Scholar * Lee, B., Clay, A. & Sy, E.
Evaluation of extracorporeal cardiopulmonary resuscitation eligibility criteria for out-of-hospital cardiac arrest patients. _BMC Res. Notes_ 14(1), 139 (2021). Article PubMed PubMed
Central Google Scholar * Sy, E. _et al._ Long-term safety of directly discharging patients home from the ICU compared to ward transfer. _J. Intensive Care Med._ 29, 08850666221090459
(2022). Google Scholar * Poses, R. M., McClish, D. K., Smith, W. R., Bekes, C. & Scott, W. E. Prediction of survival of critically ill patients by admission comorbidity. _J. Clin.
Epidemiol._ 49(7), 743–747 (1996). Article CAS PubMed Google Scholar * Ferreira, F. L., Bota, D. P., Bross, A., Mélot, C. & Vincent, J. L. Serial evaluation of the SOFA score to
predict outcome in critically ill patients. _JAMA_ 286(14), 1754–1758 (2001). Article CAS PubMed Google Scholar * Shekar, K. _et al._ Extracorporeal life support organization coronavirus
disease 2019 interim guidelines: A consensus document from an international group of interdisciplinary extracorporeal membrane oxygenation providers. _ASAIO J._ 66(7), 707–721 (2020).
Article CAS PubMed Google Scholar * Forrest, P. _et al._ Retrieval of critically ill adults using extracorporeal membrane oxygenation: an Australian experience. _Intensive Care Med._
37(5), 824–830 (2011). Article CAS PubMed Google Scholar * Critical Care Services Ontario. ECMO Consultation Guidelines: Guidance Document for Ontario Hospitals [Internet] (2020).
https://criticalcareontario.ca/wp-content/uploads/2020/10/ECMO-Consultation-Guidelines_Guidance-Document-for-Ontario-Hospitals-FINAL-2020.pdf [cited 2021 Aug 13]. * Tonna, J. E. _et al._
Management of adult patients supported with Venovenous Extracorporeal Membrane Oxygenation (VV ECMO): Guideline from the Extracorporeal Life Support Organization (ELSO). _ASAIO J. Am. Soc.
Artif. Intern. Organs_ 67(6), 601–610 (2021). Article CAS Google Scholar * Statistics Canada. Population Projections for Canada (2021 to 2068), Provinces and Territories (2021 to 2043)
[Internet] (2022). https://www150.statcan.gc.ca/n1/pub/91-520-x/91-520-x2022001-eng.htm [cited 2023 Oct 3]. * Barbaro, R. P. _et al._ Association of hospital-level volume of extracorporeal
membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. _Am. J. Respir. Crit. Care Med._ 191(8), 894–901 (2015). Article PubMed PubMed
Central Google Scholar * Rabie, A. A. _et al._ Implementation of new ECMO centers during the COVID-19 pandemic: Experience and results from the Middle East and India. _Intensive Care Med._
47(8), 887–895 (2021). Article CAS PubMed PubMed Central Google Scholar * Nagaoka, E. _et al._ Efficacy of multidisciplinary team approach with extracorporeal membrane oxygenation for
COVID-19 in a low volume ECMO center. _Artif. Organs_ 45(9), 1061–1067 (2021). Article CAS PubMed PubMed Central Google Scholar * Combes, A. _et al._ Position paper for the organization
of extracorporeal membrane oxygenation programs for acute respiratory failure in adult patients. _Am. J. Respir. Crit. Care Med._ 190(5), 488–496 (2014). Article PubMed Google Scholar *
Karagiannidis, C. _et al._ Extracorporeal membrane oxygenation: evolving epidemiology and mortality. _Intensive Care Med._ 42(5), 889–896 (2016). Article CAS PubMed Google Scholar *
Duggal, A. _et al._ Implementation of protocolized care in ARDS improves outcomes. _Respir. Care_ 66(4), 600–609 (2021). Article PubMed Google Scholar * Goligher, E. C. _et al._ Clinical
strategies for implementing lung and diaphragm-protective ventilation: Avoiding insufficient and excessive effort. _Intensive Care Med._ 46(12), 2314–2326 (2020). Article CAS PubMed
PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS Special thanks to LeeAnn Carr and the Health Information Management Services at Regina General Hospital in helping
retrieve appropriate patient charts for the study. Thank you to the Saskatchewan Health Authority (SHA) Research Department in supporting research needs. Lastly, thank you to Dr. Michael
Szafron at School of Public Health, University of Saskatchewan for coordinating the MPH student’s practicum placement with SHA. DISCLAIMER This article does not necessarily represent the
views of the University of Saskatchewan or the Saskatchewan Health Authority. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * School of Public Health, University of Saskatchewan, 107 Wiggins
Rd, Saskatoon, SK, S7N 5E5, Canada Barsa Saha * School of Health Sciences, Saskatchewan Polytech, 4635 Wascana Pkwy, Regina, SK, S4P 3A3, Canada Savannah Drapak * Pharmacy Department, Royal
Jubilee Hospital, Vancouver Island Health Authority, Victoria, BC, V8R 1J8, Canada Jonathan F. Mailman * College of Medicine, University of Saskatchewan, 1440-14th Avenue, Regina, SK, S4P
0W5, Canada Jonathan F. Mailman & Eric Sy * Faculty of Pharmaceutical Sciences, University of British Columbia, Vancouver, BC, V6T 1Z3, Canada Jonathan F. Mailman * Research Department,
Saskatchewan Health Authority, Wascana Rehabilitation Centre, 2180-23 Ave, Regina, SK, S4S 0A5, Canada Sandy Kassir * Department of Critical Care, Saskatchewan Health Authority, 1440-14th
Avenue, Regina, SK, S4P 0W5, Canada Eric Sy * Surgical Intensive Care Unit, Regina General Hospital, 1440-14 Avenue, Regina, SK, S4P 0W5, Canada Eric Sy Authors * Barsa Saha View author
publications You can also search for this author inPubMed Google Scholar * Savannah Drapak View author publications You can also search for this author inPubMed Google Scholar * Jonathan F.
Mailman View author publications You can also search for this author inPubMed Google Scholar * Sandy Kassir View author publications You can also search for this author inPubMed Google
Scholar * Eric Sy View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS B.S. and E.S. drafted the main manuscript. B.S. and E.S. conducted
statistical analysis on data extracted. B.S., J.M., S.D. and E.S. were responsible for the acquisition, analysis, or interpretation of the data. S.K. provided administrative, technical, and
material support. E.S. supervised the research project. All authors contributed to the concept and design of research, and critical revision of the manuscript for important intellectual
content. CORRESPONDING AUTHOR Correspondence to Eric Sy. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION. RIGHTS AND
PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any
medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The
images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is
not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission
directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Saha, B.,
Drapak, S., Mailman, J.F. _et al._ Evaluating service needs for veno-venous extracorporeal membrane oxygenation in patients with severe acute respiratory distress syndrome in Saskatchewan.
_Sci Rep_ 13, 17627 (2023). https://doi.org/10.1038/s41598-023-45013-6 Download citation * Received: 01 April 2023 * Accepted: 14 October 2023 * Published: 17 October 2023 * DOI:
https://doi.org/10.1038/s41598-023-45013-6 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative