- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT After a stroke event, most survivors suffer from arm paresis, poor motor control and other disabilities that make activities of daily living difficult, severely affecting quality of
life and personal independence. This randomized controlled trial aimed at evaluating the efficacy of a music-based sonification approach on upper limbs motor functions, quality of life and
pain perceived during rehabilitation. The study involved 65 subacute stroke individuals during inpatient rehabilitation allocated into 2 groups which underwent usual care dayweek)
respectively of standard upper extremity motor rehabilitation or upper extremity treatment with sonification techniques. The Fugl-Meyer Upper Extremity Scale, Box and Block Test and the
Modified Ashworth Scale were used to perform motor assessment and the McGill Quality of Life-it and the Numerical Pain Rating Scale to assess quality of life and pain. The assessment was
performed at baseline, after 2 weeks, at the end of treatment and at follow-up (1 month after the end of treatment). Total scores of the Fugl-Meyer Upper Extremity Scale (primary outcome
measure) and hand and wrist sub scores, manual dexterity scores of the affected and unaffected limb in the Box and Block Test, pain scores of the Numerical Pain Rating Scale (secondary
outcomes measures) significantly improved in the sonification group compared to the standard of care group (time*group interaction < 0.05). Our findings suggest that music-based
sonification sessions can be considered an effective standardized intervention for the upper limb in subacute stroke rehabilitation. SIMILAR CONTENT BEING VIEWED BY OTHERS A RANDOMISED
CLINICAL TRIAL COMPARING 35 HZ VERSUS 50 HZ FREQUENCY STIMULATION EFFECTS ON HAND MOTOR RECOVERY IN OLDER ADULTS AFTER STROKE Article Open access 28 April 2021 FEASIBILITY OF HOME HAND
REHABILITATION USING MUSICGLOVE AFTER CHRONIC SPINAL CORD INJURY Article Open access 09 November 2022 CLINICAL EFFICACY OBSERVATION OF REPETITIVE MAGNETIC STIMULATION FOR TREATING UPPER LIMB
SPASTICITY AFTER STROKE Article Open access 22 May 2025 INTRODUCTION After a stroke event, most survivors (80–90%) suffer from arm paresis, poor motor control and other disabilities, which
evolve in a chronic condition in about 30–40% of cases1,2. Consequently, patients have difficulty in performing activities of daily living, a fact that severely affects their quality of life
and independence3. Task-oriented sensory-motor training, which allows to transmit the sensory information of the feedback to the central nervous system during task execution, and movements
adaptation, is recognized as significant in increasing post-stroke arm function and dexterity2,4. Beside other factors, such as patient’s compliance and subjective interest in stimulus, the
intensity of training and patient’s motivation have been indicated as key features for a successful rehabilitation therapy5,6. The development of technologies for rehabilitation has made it
possible to formulate new application paradigms obtained by integrating the current rehabilitation pathways with instrumental interventions7,8. Sensory-motor rehabilitation techniques,
obtained through technological devices (such as virtual reality, robots, non-invasive stimulations , motion capture) and used in support of traditional rehabilitation techniques, seem to
provide objective parameters for patient evaluation, accelerate the process of motor recovery and improve motor performance at discharge by means of a top-down approach9,10. Although the
results obtained with the currently available devices are encouraging, we are only at an early stage for the exploitation of these technologies. In fact, while technology-assisted
rehabilitation of the upper limb has demonstrated to have a significant impact on motor outcomes, especially at the proximal level (shoulder and elbow)11, the functional recovery of the hand
(in particular of the prehension function) still presents some issues12,13. Music and its elements (especially the rhythm) are widely used in rehabilitation14.This is due to the activation
of the neuronal networks, in the limbic and paralimbic areas, and in the brain areas involved in movement (motor cortex, supplementary motor area, cerebellum, basal ganglia, etc.)15,16. Many
studies document the possibility that exposure to music during training, but, also through specific rehabilitation interventions, may induce plastic changes15,16,17,18,19 in the
sensory-auditory circuits and motor areas20,21. These changes, resulting in a neuronal reorganization in the nodal points of the brain networks and in fiber bundles, can determine effects
lasting beyond the actual duration of the rehabilitation intervention15. Moreover, music in the rehabilitation process determines an emotional involvement, creating a strong motivational
basis15,16. The recent literature shows how the use of music in stroke rehabilitation can improve gait (speed, cadence and step length, balance)22,23, movement of the upper limbs24,25,
language26,27, but also mood and other psychological aspects28,29,30. More recent studies use, for the rehabilitation of the upper limbs, the mapping of the patient’s movements to whom a
sonorous stimulus is associated (sonification)31,32,33,34. Sonification can improve motor functions rehabilitation and can facilitate the integration of auditory and sensory-motor
systems35,36,37. This technique can also strengthen and support the damaged proprioceptive system and can make the rehabilitative process more pleasant and stimulating from an emotional and
motivational point of view15,37. In some studies, the kinematic data of the gesture are translated into modulations of some parameters (typically frequency and amplitude) of a continuous
synthetic sound38,39,40. In other post-stroke hand rehabilitation studies, the sonification action was based on the execution of short scales or melodic intervals that the patient had to
reproduce through specific movements, with the final goal of creating "simple nursery rhymes or other familiar tunes", modulating music timbre and intensity41. Further, Reh et
al.42 supported the rehabilitation of walking by a combination of an ecological sound (noise produced by a step in the snow) together with a predetermined glissando effect. In this study the
sonification can be considered as a properly selected set of sonorous-music stimuli activated by patient’s movements with the mediation of a sensor (in this specific case the Leap Motion
Controller). Synthesized sounds/musical texture and their parameters (mainly rhythm, pitch/melody, intensity/dynamics, harmony and timbre) are used to represent movements characteristics,
especially from a temporal and spatial point of view. Sonification makes possible the improvement of sensorimotor learning, proprioception, movements planning and execution37. In particular
music elements used in this study were automatically associated to the patient’s movements without involvement of any cognitive tasks. This allows the patient to focus attention mainly on
the motor outcome. In particular, given the importance of hand functions in activities of daily living and manipulation, the protocol (Sonichand) was developed and validated for the training
of pronation and supination of the forearm, ulnar and radial deviation of the wrist and hand grasping movements43. The main objective of this randomized controlled study conducted in
subacute stroke patients during inpatient rehabilitation, was to verify the effectiveness (evaluated through the assessment of the upper limb level of impairment at baseline and end of
treatment) of a new rehabilitative hand treatment based on a musical sonification approach compared to a conventional intervention. The secondary aim was to evaluate if this technique could
be beneficial for reduction of pain perceived during training and improve the patient's perceived quality of life. The main hypothesis of this study was that our sonification approach
could be more effective than a conventional intervention for the rehabilitation of subacute stroke patients, especially for the recovery of hand motor function. RESULTS Clinical
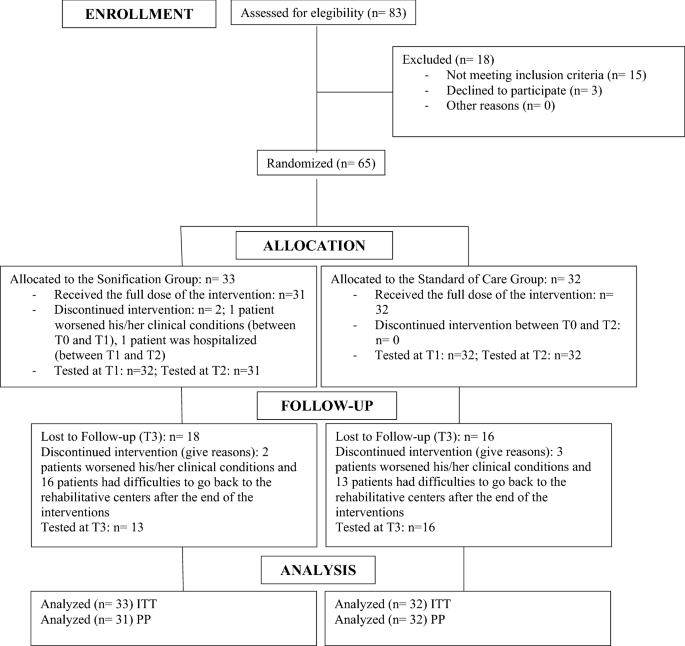
characteristics of the sample at baseline are reported in Table 1. Two patients allocated to the Sonification Group interrupted the trial between T0 and T2: the first one worsened his/her
clinical condition and the second one was hospitalized. In addition, 18 patients in the Sonification Group and 16 patients in the Standard of Care Group were lost to follow-up due to the
clinical worsening (2 patients in the Sonification Group and 3 patients in the Standard of Care Group) or to the difficulty to go back to the rehabilitative centers after the end of the
interventions (16 patients in the Sonification Group and 13 patients in the Standard of Care Group) (Flow Diagram is reported in Fig. 1). No side effects were observed in both the
experimental and control groups after training. PRIMARY OUTCOME The upper limb impairment assessed by the Fugl-Meyer Upper Extremity scale total score44 , showed a significantly greater
improvement between T0 and T2 (Table 2, Fig. 2) in the Sonification Group compared to the Standard of Care Group (time*group interaction: p = 0.024), as pointed out by the Intention To Treat
analysis. SECONDARY OUTCOMES At the Intention To Treat analysis, other significantly greater improvements between T0 and T2 in the Sonification versus the Standard of Care Groups were found
for the Distal Score (time*group interaction: p = 0.016), Wrist Score (time*group interaction: p = 0.033) and Hand Score (time*group interaction: p = 0.04) subscales. Also, Manual dexterity
significantly improved (T0 vs T2) in the Sonification Group as showed by the Box and Block Test45 (affected limb time*group interaction: p = 0.020; unaffected limb time*group interaction: p
= 0.004). The Box and Block Test score Ratio improvement was not significant (time*group interaction: p = 0.19). In addition to motor outcomes the study put in evidence the effects of
sonification in pain perception: the Sonification Group showed a significant reduction in Numerical Pain Rating Scale46 scores compared to the Standard of Care Group (time*group interaction:
p = 0.006). No significant changes were observed in spasticity (Modified Ashworth Scale)47 and perceived quality of life (McGill Quality of Life)48. All results are summarized in Table 2
and Fig. 3 and the same findings were confirmed at the Per Protocol analyses (Supplementary Table S1). DISCUSSION The study confirmed how the sonification with music elements is able to
facilitate the recovery process compared to the traditional rehabilitative approach. Main results are related to the global upper limb impairment (primary endpoint of the study), assessed by
the Fugl-Meyer Upper Extremity scale (FM-UE). In particular, both the experimental (SG) and control (SoCG) groups scored a clinically significant increase of the FM-UE total score after
training, but only the SG had a clinically significant (> 5) improvement49. Conversely to the control group the experimental group did not show a significant improvement at proximal level
at T2. A possible explanation could be that the Sonichand protocol involves mainly the distal segments of the arm and this aspect should be considered in future studies. Results of the
present study can be extended to manual dexterity, as testified by the improved Box and Block Test (BBT), both in affected and unaffected limbs. The score improvement observed for the
presumed-to-be-unaffected upper extremity could be due to a learning phenomenon obtained during repeated evaluations or to undetected motor deficit due to the brain lesion thus involving
slight abnormal kinematics subject to improvements50. In addition, some BBT variability could be due to a day-by-day effect that however should be minimized by taking into consideration the
ratio score51. In accordance with Kinney et al.52 thresholds, our study showed a large effect size for time effect (> 0.55) for both FM-UE total and subscales values and for the BBT of
the affected upper limb, a medium effect size (≥ 0.31, < 0.55) for BBT of unaffected upper limb and a small effect size (≥ 0.14, < 0.31) for the remaining outcome variables. Conversely
to a study for robot assisted hand training53, the effect size for group effect of our study was not statistically significant for all outcome variables. This could be likely due to the
different training device and intensity of training (20 min. vs. 60 min.) adopted in the two studies. Finally, small effect sizes of the time*group interactions should be evaluated in a
framework of power of interactions in the analysis of variance models. The sonification technique used in our study was very intuitive, compared to other similar interventions37. In fact,
music support was intrinsically associated with the patient's movements, regardless of his/her intention to produce sounds. This peculiarity allowed the patient to focus mainly on the
movement and, at the same time, to receive a natural feedback on its coherence and quality (i.e. a correct movement produced a fluent musical progression). The above mentioned mechanisms
could have helped the patient to model/adjust and re-learn movements during the rehabilitative intervention. Another important result was found by evaluating the effect of sonification on
pain perception associated to upper extremity movements during the rehabilitation intervention. Despite higher levels of perceived pain (Baseline scores) in the Sonification group compared
to those perceived by the control group patients, the music-based rehabilitative approach used in this study was able to produce a significant decrease of NPRS score. In accordance with the
literature concerning the use of music in pain medicine, our data showed how the presence of musical patterns can significantly reduce the perceived pain, likely because music helps patients
to get distracted from the pain condition54. The harmonic and melodic progressions used in the study, compared to other possible sounds (e.g. sinusoidal tones) could have contributed to
create predictable and pleasant sequences, involving the recall and recognition of the tonal trend typical of the music listening experience. In addition, the predictability of sequences
could also have produced a facilitation effect during the preparation and execution of movements. One of the main limitations of the study is the limited data available for the planned
follow-up assessment at 1 month after the end of treatment (T3). In spite of therapists’ recommendation, only less than 50% of patients completed the study, making the reliability of results
at T3 questionable. This could be due to the patients’ difficulties to get back to the rehabilitative centers after the end of the interventions and/or to other reasons, such as a lack of
motivation/unwillingness due to a follow-up too close to the study conclusion and conflicting with the new difficulties of daily life activities of the whole family. For this reason, we
decided to include the follow-up analysis only into the supplementary materials (Supplementary Table S2). This analysis showed a maintenance of results over time. Another limitation of the
study is that we did not apply block randomization in the allocation of patients to experimental and control groups. Taking into account the defined exclusion criteria, the block
randomization would not have guaranteed in a reasonable time, patients’ enrollment at the different Units, with a balanced and homogeneous sample size. In addition, an increased sample size
could have produced greater effect size to support the beneficial effect of the sonification technique. Finally, the lack of other evaluation methods, such as neuroimaging techniques (fMRI)
aimed at pointing out possible changes in the brain connectivity and their possible correlation with post-treatment performance indexes, should be considered as a further limitation. The
study proved that this type of music intervention can improve movements and reduce pain during the rehabilitation process in patients with stroke. Upper limb rehabilitation with sonification
techniques can be considered a standardized intervention, effective and easy to implement in subacute stroke rehabilitation. The low-cost of the sonification set-up makes the intervention
widely exploitable into the standard occupational/physical therapy settings. Also, it is expected that the Sonichand protocol and approach, thanks to the powerful feedback produced by
movements sonification, could be beneficial also for the treatment of other neurological conditions in which upper limbs movements are impaired due to specific brain lesions (i.e., gesture
disturbances, apraxia and poor gesture imitation). Future studies involving other clinical conditions and with a more comprehensive assessment protocol, could strengthen the significant
findings obtained by this study. METHODS This randomized controlled trial involved 65 subacute stroke patients who underwent inpatient rehabilitation allocated into two groups: the SG (n =
33) underwent sonification sessions (see “Interventions” sub-section) and the SoCG (n = 32) underwent traditional motor rehabilitation sessions. The randomization was centrally managed: a
randomization list (simple randomization), generated accordance with a completely randomized parallel group study design, was generated at the beginning of the study and delivered to the
Principal Investigator (PI) of the study. Each recruited subject was allocated in SG or SoCG by the PI on the basis of the randomization list by assigning a unique identifying code so to
guarantee data anonymization during data collection, analysis and interpretation processes. The blindness of the evaluations was guaranteed both for questionnaires data collection and
statistical processing. Subjects were recruited from March 27th 2017 to April 15th 2019 in 5 Italian rehabilitative units located at Maugeri Scientific Clinical Institutes of Pavia,
Montescano (PV) and Nervi (GE), S. Lucia Foundation IRCCS (Rome) and Neurological Clinic of S. Martino Hospital (University of Genoa). All procedures performed in this study were in
accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The study was approved by the Ethical Board of the Istituti Clinici Scientifici Maugeri IRCCS, Pavia, Italy (2088 CE, December 19th, 2016) and registered on https://clinicaltrials.gov
(Trial Number Identifier: NCT03306797, date of registration: 11/10/2017), all participants gave their written informed consent to participate in the study. INCLUSION AND EXCLUSION CRITERIA
Patients matching the following characteristics were included in the study: * Age 40–85 years * Ischaemic lesion in a single hemisphere (right or left hemiplegia/hemiparesis) * Clinically
evaluable residual movement capacity of the paretic upper limb (ability to autonomously make postural adjustments during reaching tasks) * Mini Mental State Examination > 24 * Acute onset
no more than 180 days prior to enrollment in the study The exclusion criteria of the Study were the following: * Presence of neglect (evaluated through a clinical and functional assessment)
* previous or concomitant diseases affecting upper limb functions (e.g. Parkinson's disease, multiple sclerosis, shoulder periarthritis, Dupuytren's disease, etc.) *
rehabilitation treatments with music in the last year INTERVENTIONS The patients recruited in the study were admitted to the rehabilitation centers and received usual treatment for their
subacute stage of disease (such as occupational therapy, speech therapy, psychological support, lower extremity rehabilitation, etc.) in addition to a specific upper extremity rehabilitation
based on (a) standard motor exercises or (b) standard motor exercises supported by sonification techniques. STANDARD MOTOR EXERCISES The upper limb rehabilitation was carried out in
accordance with the Italian Stroke Prevention and Educational Awareness Diffusion (SPREAD) guidelines55 and took into account a traditional neuro-motor approach aimed at improving motor
control and reducing spasticity. At the same time, these methods were combined with an individualized and progressive functional re-education through task-oriented programs56. The first
phase of the treatment (passive treatment, 15 min) aimed at relaxing muscle tone with stretching. The exercises were chosen, based on the needs and residual motor skills of the patient, from
among the following: * fingers opening and closing * prono-supination of the forearm * wrist mobilization The second phase of the treatment (20 min) included movements actively performed by
the patient. The patient was offered at least 6 different exercises. Each exercise lasted 90 s and was followed by a break of 30–60 s. The exercises were chosen from the following: * 1.
Forearm–wrist: (a) flexion and extension of the wrist in the intermediate position of the forearm (horizontal plane), (b) flexion and extension of the wrist with pronated arm (vertical
plane), (c) ulnar and radial deviation of the wrist, (d) pronation and supination of the forearm. * 2. Hand: (a) grasp; (b) pinch; (c) finger extension (d) abduction and adduction of the
fingers * 3. Shoulder-elbow: (a) elbow flexion and extension; (b) combined movement of shoulder flexion and elbow extension During the active phase the therapist assisted the patient in the
movement that took place autonomously, with the active participation of the patient. The exploration of the workspace was carried out using tools such as a table facilitating sliding of the
arm on the work surface. If compatible with patient’s impairment and performance, grip-release exercises of medium-volume objects and their displacement in the space were also included.
STANDARD MOTOR EXERCISES SUPPORTED BY SONIFICATION TECHNIQUES This intervention was similar to the above mentioned treatment (a), i.e. it included a passive treatment phase without
sonification (15 min) and a second phase (20 min) in which the motor exercises were supported by sonification techniques. In this second phase of treatment the patient performed the
movements actively, by practicing a sequence of exercises lasting about 90 s each, separated by a 30–60 s resting period. The sonification process was made using an adequate setup including
a technological sensor (Leap Motion Controller)57,58,59, managed with an ad-hoc developed application parameterizing the data read by the sensor by producing sounds in response to some
specific hand movements. The Leap Motion Controller (LMC; Leap Motion, Inc., San Francisco, CA, USA) is described as a low-cost Human Computer Interface specifically optimized for the
recognition of gestures produced by hands, fingers and pointer objects, with a precision, validated in real situation, of about 0.7 mm. The LMC is connected to the computer through a USB 3.0
communication interface and does not require contact with the patient. Thanks to the use of 3 infrared LEDs and 2 optical sensors, it can create a three-dimensional workspace of about 120
cm × 60 cm × 60 cm. The LMC is capable to capture the movement of hands and fingers thanks to two monochromatic cameras and three infrared LEDs and it is able to build a vector
representation of the hand, fingers, wrist and forearm up to the elbow. The device is not so precise for temporal responses but, unlike tapping, this type of exercises do not need a strict
temporal association between movements and sounds. Before starting, the minimum and maximum points of the movements (range of motion) are measured. If the sonification is discrete (e.g. 4
notes of a musical scale) this range is further divided into thresholds. During the performance, if the read value falls within a preset range around a minimum/maximum threshold, a preset
sound sample is played (basically each threshold is a trigger for the assigned note). If the sonification is continuous, the read value will modulate the sound along a continuum, from the
minimum to the maximum level measured (range of motion). In this trial we used a sampling rate of 25 Hz. The sensor, which is positioned under the palm of the hand at a distance of about 15
cm, identifies and maps the limb, creating a representation of it in points, providing the relative kinetic characteristics (spatial coordinates, acceleration, direction, inclination, etc.)
for each point. The software program (https://ismm.ircam.fr/leapmotion/ ), used to carry out our experiments, was developed with the Max 7 software programming environment (Max 7 by Cycling
’74, Walnut, CA, USA, https://cycling74.com). Thanks to this application the patient's gestures are supported by two modalities: * 1. In the first, movements (forearm-wrist: flexion and
extension of the wrist in the intermediate position of the forearm—horizontal plane-, flexion and extension of the wrist with pronated arm—vertical plane-, ulnar and radial deviation of the
wrist; hand: pinch, finger extension; shoulder-elbow: elbow flexion and extension) trigger and modulate a harmonic progression built on the consecutive grades of the major scale played as
an ascending and descending arpeggio also with a consistent volume (ascending crescendo and descending diminuendo sounds) (Supplementary Video S3). * 2. In the second, movements
(forearm-wrist: pronation and supination of the forearm; hand: grasp, abduction and adduction of the fingers; shoulder-elbow: combined movement of shoulder flexion and elbow extension)
modulate the volume and low-pass cutoff frequency of a tone filter applied to a synthetic texture. It is a kind of tone modulation of a pad sound, from dull to bright, based on a harmonic
progression built on the consecutive grades of a major scale (Supplementary Video S4). On the basis of the exercises selected for rehabilitation, some music parameters (pitch, volume and
spectrum—quality/brilliance of tone) have been identified and superimposed on the gesture. The correct execution of the gesture leads patients to cyclically perform a harmonic progression of
arpeggios. Considering the daily administration of the training protocol, different instruments were associated to the various exercises to increase the sound variability (for example:
trumpet, flute, cello, guitar, piano etc., as well as some timbre variants for the pad performed by a synthesizer). To ensure correct understanding of the training protocol, before the
experimental intervention, the therapist measured the active range of motion for sensor mapping and provided a short demonstration of the exercises (learning phase) to the patient who
carried out a short training with the non-plegic limb. In addition, in order to guarantee uniformity of intervention, the experimental set up (including a wheelchair with a transparent table
and a clamp to support the Leap Motion Controller) was replicated in each Unit involved in the study. All interventions (5 days a week for 4 weeks, for a total of 20 sessions) were assisted
by physiotherapists or occupational therapists with an expertise in hand rehabilitation or neurorehabilitation and specifically trained to use the Leap Motion Controller and the
sonification described setting. The therapists involved into the protocol received at least 8 h of specific training before the beginning of experiments. ASSESSMENT The rehabilitation
interventions were evaluated by blinded evaluators at baseline (T0), after 2 weeks (T1), at the end of treatment (T2, after 4 weeks) and 1 month after the end of the treatment (T3). The
FM-UE44 (score range 0–66) was used to evaluate the performance-based sensorimotor functions of the impaired upper limb. Furthermore, in order to detail the motor improvement both at the
proximal and distal level, the FM-UE was sub-scaled into proximal (shoulder/elbow, score range 0–42), distal (wrist/hand, score range 0–24), wrist (score range 0–10) and hand (score range
0–14) subscores60. The Modified Ashworth Scale (MAS, score range 0–4; 6 categories) was used to evaluate muscle tone at the upper limb61. In accordance with previous studies, the score of
‘1+’ category was converted to 1.4 to be managed in statistical analysis60. The BBT was used as a measure of gross manual dexterity62. In particular, for this test we assessed the
performance (number of blocks) both of the affected and unaffected limbs and their score ratio (BBT ratio = BBT affected limb/BBT unaffected limb) in order to compensate for their
variability51. Pain and quality of life assessment were rated using respectively the NPRS63 (score range 0–10) and the McGill Quality of Life (MQOL-it, score range 0–160)48. OUTCOMES
MEASURES The primary outcome measure of the study was the evaluation of the improvement in total scores of the FM-UE between T0 and T2. Secondary outcomes measure were other motor aspects
(including scores of BBT, MAS and sub-items scores of the FM-UE), pain (scores of NPRS) and the perceived quality of life (MQOL-it). STATISTICS Sample size: the sample size estimate is based
on previous data acquired from results of rehabilitation interventions, with and without technology-assisted techniques, carried out at the facilities participating in the study64. For the
sizing of the present study it is assumed that the use of a technological system for sonification allows to achieve at least clinically relevant results as traditional rehabilitation. An
increase of at least 6 points in FM-UE is recognized to be the minimal clinically important difference between baseline and end of treatment following rehabilitation54. The work hypothesis,
based on previous data, was that the pre-post treatment difference in FM-UE was at least 5 point higher in the SG than in the SoCG groups. With these hypotheses and assuming a standard
deviation of the pre-post treatment differences of 10, a total sample of 65 subjects can guarantee a study power of 80% and a type I error of 5%. DATA ANALYSIS Descriptive statistics were
carried out for all the collected variables. Means and standard deviations were reported for normally distributed quantitative variables. In case of significant discrepancy from the
normality, medians and interquartile ranges were also included. Nominal level variables were summarized as frequencies and percentages. Baseline clinical characteristics between SG and SoG
groups were compared by means of Student’s t test, Mann–Whitney U test or chi-square test according to the nature and distribution of the variables. Inferential statistics were performed on
the Intention To Treat population defined as all randomized subjects. Handling of missing data was managed according to a strategy pre-specified in the study protocol and referred to the
four time points of assessment. Imputation strategy included the handling of missing at random and not at random. Generalized linear mixed models were applied to handle missingness at single
timepoints where measured repeatedly over time. Last Observation Carried Forward (LOCF) method was applied to missingness of patients who prematurely interrupted the trial. Analyses on the
PP population were also conducted to support the findings. Repeated measures analysis of variance with one factor (factor: experimental/control group) or non-parametric approach
(Kruskall-Wallis statistics) was used to assess potential differences between baseline (T0) and end of treatment (T2) for the primary and secondary endpoints. The same models were applied to
assess trends over time at the four assessment timepoints foreseen in the protocol (T0 = baseline T1 = 2 weeks of treatment, T2 = 4 weeks, end of treatment, T3 = 8 weeks, follow-up). Due to
the huge amount of missing data at the follow-up (T3), this analysis was carried out on the per protocol population only without any imputation of missing data. Effect sizes of the main
effects, repeated measures and interactions were finally computed to point out the magnitude of the effects in a standardized metric with the aim of favoring comparisons with other studies.
Effect size was rated as small (d = 0.14), medium (d = 0.31) and large (d = 0.55) in accordance with the effect size interpretation guidelines provided by Kinney and coll. for a study
classified as a Multicomponent intervention52. Experiment-wise error rate was set at 5%. All analyses were conducted using SPSS Statistics Professional package. DATA AVAILABILITY The
datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. REFERENCES * Langhorne, P., Coupar, F. & Pollock, A.
Motor recovery after stroke: A systematic review. _Lancet Neurol._ 8, 741–754 (2009). Article PubMed Google Scholar * Pollock, A. _et al._ Interventions for improving upper limb function
after stroke. _Cochrane Database Syst. Rev._ 12, CD0102820 (2014). Google Scholar * Kwakkel, G. & Kollen, B. J. Predicting activities after stroke: What is clinically relevant?. _Int.
J. Stroke_ 8, 25–32 (2013). Article CAS PubMed Google Scholar * Nowak, D. A., Hermsdörfer, J. & Topka, H. Deficits of predictive grip force control during object manipulation in
acute stroke. _J. Neurol._ 250, 850–860 (2003). Article PubMed Google Scholar * Kwakkel, G. Impact of intensity of practice after stroke: Issues for consideration. _Disabil. Rehabil._ 28,
823–830 (2006). Article PubMed Google Scholar * Maclean, N., Pound, P., Wolfe, C. & Rudd, A. Qualitative analysis of stroke patients’ motivation for rehabilitation. _BMJ_ 321,
1051–1054 (2000). Article CAS PubMed PubMed Central Google Scholar * Iosa, M. _et al._ Seven capital devices for the future of stroke rehabilitation. _Stroke Res. Treat._ 2012, 187965
(2012). CAS PubMed PubMed Central Google Scholar * Moens, B. & Leman, M. Alignment strategies for the entrainment of music and movement rhythms. _Ann. N. Y. Acad. Sci._ 1337, 86–93
(2015). Article ADS PubMed Google Scholar * Morone, G. _et al._ Rehabilitative devices for a top-down approach. _Expert Rev. Med. Devices_ 16, 187–195 (2019). Article CAS PubMed
Google Scholar * Dauvergne, C. _et al._ Home-based training of rhythmic skills with a serious game in Parkinson’s disease: Usability and acceptability. _Ann. Phys. Rehabil. Med._ 61,
380–385 (2018). Article PubMed Google Scholar * Mehrholz, J., Pohl, M., Platz, T., Kugler, J. & Elsner, B. Electromechanical and robot-assisted arm training for improving activities
of daily living, arm function, and arm muscle strength after stroke. _Cochrane Database Syst. Rev._ 9, CD006876 (2018). PubMed Google Scholar * Balasubramanian, S., Klein, J. & Burdet,
E. Robot-assisted rehabilitation of hand function. _Curr. Opin. Neurol._ 23, 661–670 (2010). Article PubMed Google Scholar * Yue, Z., Zhang, X. & Wang, J. Hand rehabilitation
robotics on poststroke motor recovery. _Behav. Neurol._ 2017, 3908135 (2017). Article PubMed PubMed Central Google Scholar * Moumdjian, L., Sarkamo, T., Leone, C., Leman, M. & Feys,
P. Effectiveness of music-based interventions on motricity or cognitive functioning in neurological populations: A systematic review. _Eur. J. Phys. Rehabil. Med._ 53, 466–482 (2017). PubMed
Google Scholar * Schlaug, G. Part VI introduction: Listening to and making music facilitates brain recovery processes. _Ann. N. Y. Acad. Sci._ 1169, 372–373 (2009). Article ADS PubMed
PubMed Central Google Scholar * Altenmuller, E., Marco-Pallares, J., Munte, T. F. & Schneider, S. Neural reorganization underlies improvement in stroke-induced motor dysfunction by
music-supported therapy. _Ann. N. Y. Acad. Sci._ 1169, 395–405 (2009). Article ADS CAS PubMed Google Scholar * Ripollés, P. _et al._ Music supported therapy promotes motor plasticity in
individuals with chronic stroke. _Brain Imaging Behav._ 10, 1289–1307 (2016). Article PubMed Google Scholar * Sihvonen, A. J. _et al._ Music-based interventions in neurological
rehabilitation. _Lancet Neurol._ 16, 648–660 (2017). Article PubMed Google Scholar * Herholz, S. C. & Zatorre, R. J. Musical training as a framework for brain plasticity: Behavior,
function, and structure. _Neuron_ 76, 486–502 (2012). Article CAS PubMed Google Scholar * Bangert, M. & Altenmuller, E. Mapping perception to action in piano practice: A longitudinal
DC-EEG-study. _BMC Neurosci._ 4, 26–36 (2003). Article PubMed PubMed Central Google Scholar * Bangert, M. _et al._ Shared networks for auditory and motor processing in professional
pianists: Evidence from fMRI conjunction. _Neuroimage_ 30, 917–926 (2006). Article PubMed Google Scholar * Suh, J. H. _et al._ Effect of rhythmic auditory stimulation on gait and balance
in hemiplegic stroke patients. _NeuroRehabilitation_ 34, 193–199 (2014). Article PubMed Google Scholar * Hayden, R., Clair, A. A., Johnson, G. & Otto, D. The effect of rhythmic
auditory stimulation (RAS) on physical therapy outcomes for patients in gait training following stroke: A feasibility study. _Int. J. Neurosci._ 119, 2183–2195 (2009). Article PubMed
Google Scholar * van Wijck, F. _et al._ Making music after stroke: Using musical activities to enhance arm function. _Ann. N. Y. Acad. Sci._ 1252, 305–311 (2012). Article ADS PubMed
Google Scholar * Schneider, S., Schonle, P. W., Altenmuller, E. & Munte, T. F. Using musical instruments to improve motor skill recovery following a stroke. _J. Neurol._ 254, 1339–1346
(2007). Article CAS PubMed Google Scholar * Lim, K. B. _et al._ The therapeutic effect of neurologic music therapy and speech language therapy in post-stroke aphasic patients. _Ann.
Rehabil. Med._ 37, 556–562 (2013). Article ADS PubMed PubMed Central Google Scholar * Kim, S. J. & Jo, U. Study of accent-based music speech protocol development for improving voice
problems in stroke patients with mixed dysarthria. _NeuroRehabilitation_ 32, 185–190 (2013). Article PubMed Google Scholar * Jun, E. M., Roh, Y. H. & Kim, M. J. The effect of
music-movement therapy on physical and psychological states of stroke patients. _J. Clin. Nurs._ 22, 22–31 (2013). Article PubMed Google Scholar * Kim, D. S. _et al._ Effects of music
therapy on mood in stroke patients. _Yonsei Med. J._ 52, 977–981 (2011). Article ADS PubMed PubMed Central Google Scholar * Magee, W. L. & Davidson, J. W. The effect of music
therapy on mood states in neurological patients: A pilot study. _J. Music Ther._ 39, 20–29 (2002). Article PubMed Google Scholar * Bevilacqua, F. _et al._ Sensori-motor learning with
movement sonification: Perspectives from recent interdisciplinary studies. _Front. Neurosci._ 10, 385 (2016). Article PubMed PubMed Central Google Scholar * Effenberg, O., Fehse, U.,
Schmitz, G., Krueger, B. & Mechling, H. Movement sonification: Effects on motor learning beyond rhythmic adjustments. _Front. Neurosci._ 10, 219 (2016). Article PubMed PubMed Central
Google Scholar * Friedman, N. _et al._ Retraining and assessing hand movement after stroke using the MusicGlove: Comparison with conventional hand therapy and isometric grip training. _J.
Neuroeng. Rehabil._ 11, 76 (2014). Article PubMed PubMed Central Google Scholar * Zondervan, D. K. _et al._ Home-based hand rehabilitation after chronic stroke: Randomized, controlled
single-blind trial comparing the MusicGlove with a conventional exercise program. _J. Rehabil. Res. Dev._ 53, 457–472 (2016). Article PubMed Google Scholar * Scholz, D. S. _et al._
Sonification as a possible stroke rehabilitation strategy. _Front. Neurosci._ 8, 332 (2014). Article PubMed PubMed Central Google Scholar * Scholz, D. S., Rhode, S., Großbach, M.,
Rollnik, J. & Altenmüller, E. Moving with music for stroke rehabilitation: A sonification feasibility study. _Ann. N. Y. Acad. Sci._ 1337, 69–76 (2015). Article ADS PubMed Google
Scholar * Scholz, D. S. _et al._ Sonification of arm movements in stroke rehabilitation—a novel approach in neurologic music therapy. _Front. Neurol._ 7, 106 (2016). Article PubMed PubMed
Central Google Scholar * Schmitz, G. _et al._ Movement sonification in stroke rehabilitation. _Front. Neurol._ 9, 389 (2018). Article PubMed PubMed Central Google Scholar * Ghai, S.,
Schmitz, G., Hwang, T. H. & Effenberg, A. O. Auditory proprioceptive integration: Effects of real-time kinematic auditory feedback on knee proprioception. _Front. Neurosci._ 12, 142
(2018). Article PubMed PubMed Central Google Scholar * Effenberg, A. O. & Schmitz, G. Acceleration and deceleration at constant speed: Systematic modulation of motion perception by
kinematic sonification. _Ann. N. Y. Acad. Sci._ 1425, 52–69 (2018). Article ADS PubMed Google Scholar * Nikmaram, N. _et al._ Musical sonification of arm movements in stroke
rehabilitation yields limited benefits. _Front. Neurosci._ 13, 1378 (2019). Article PubMed PubMed Central Google Scholar * Reh, J., Hwang, T. H., Schmitz, G. & Effenberg, A. O. Dual
mode gait sonification for rehabilitation after unilateral hip arthroplasty. _Brain Sci._ 9, 66 (2019). Article PubMed Central Google Scholar * Colombo, R. _et al._ The SonicHand protocol
for rehabilitation of hand motor function: A validation and feasibility study. _IEEE Trans. Neural. Syst. Rehabil. Eng._ 27, 664–672 (2019). Article CAS PubMed Google Scholar * Chen,
P., Lai, C. K., Chung, R. C. & Ng, S. S. The Jacket Test for assessing people with chronic stroke. _Disabil. Rehabil._ 39, 2577–2583 (2017). Article PubMed Google Scholar * Leathley,
M. J. _et al._ Reliability of measurements of muscle tone and muscle power in stroke patients. _Age Ageing_ 29, 223–228 (2000). Article PubMed Google Scholar * Desrosiers, J., Bravo, G.,
Hébert, R., Dutil, E. & Mercier, L. Validation of the box and block test as a measure of dexerity of elderly people: Reliability, validity, and norms studies. _Arch. Phys. Med. Rehabil._
75, 751–755 (1994). Article CAS PubMed Google Scholar * McCaffery, M. & Beebe, A. _Pain: Clinical Manual for Nursing Practice_ (CV Mosby Company, 1989). Google Scholar * Sguazzin,
C., Giorgi, I., Alesii, A. & Fini, M. Italian validation of the McGill Quality of Life Questionnaire (MQOL-It). _G. Ital. Med. Lav. Ergon._ 32, B58-62 (2010). PubMed Google Scholar *
Page, S. J., Fulk, G. D. & Boyne, P. Clinically important differences for the upper-extremity Fugl-Meyer Scale in people with minimal to moderate impairment due to chronic stroke. _Phys.
Ther._ 92, 791–798 (2012). Article PubMed Google Scholar * Nakamura, T., Abreu, B. C., Patterson, R. M., Buford, W. L. Jr. & Ottenbacher, K. J. Upper-limb kinematics of the
presumed-to-be-unaffected side after brain injury. _Am. J. Occup. Ther._ 62, 46–50 (2008). Article PubMed Google Scholar * Mathiowetz, V., Volland, G., Kashman, N. & Weber, K. Adult
norms for the Box and Block Test of manual dexterity. _Am. J. Occup. Ther._ 39, 386–391 (1985). Article CAS PubMed Google Scholar * Kinney, A. R., Eakman, A. M. & Graham, J. E. Novel
effect size interpretation guidelines and an evaluation of statistical power in rehabilitation research. _Arch. Phys. Med. Rehabil._ 101, 2219–2226 (2020). Article PubMed Google Scholar
* Orihuela-Espina, F. _et al._ Robot training for hand motor recovery in subacute stroke patients: A randomized controlled trial. _J. Hand Ther._ 29, 51–57 (2016). Article PubMed Google
Scholar * Linnemann, A. _et al._ The effects of music listening on pain and stress in the daily life of patients with fibromyalgia syndrome. _Front. Hum. Neurosci._ 9, 434 (2015). Article
PubMed PubMed Central Google Scholar * AA.VV. Trattamento riabilitativo e continuità dell’assistenza, in Stroke Prevention And Educational Awareness Diffusion (SPREAD), Ictus Cerebrale:
Linee guida italiane di prevenzione e trattamento, Pubblicazioni Catel-Hyperphar Group SpA, pp. 297–376 (2003). * Carr, J. H. & Shepherd, R. B. A motor learning model for stroke
rehabilitation. _Physiotherapy_ 75, 372–380 (1989). Article Google Scholar * Iosa, M. _et al._ Leap motion controller videogame-based therapy for rehabilitation of elderly patients with
post-acute stroke: A feasibility pilot study. _Top Stroke Rehabil._ 22, 306–316 (2015). Article PubMed Google Scholar * Smeragliuolo, A. H., Hill, N. J., Disla, L. & Putrino, D.
Validation of the leap motion controller using markered motion capture technology. _J. Biomech._ 49, 1742–1750 (2016). Article PubMed Google Scholar * Li, W., Hsieh, C., Lin, L. &
Chu, W. Hand gesture recognition for post-stroke rehabilitation using leap motion. _Int. Conf. Appl. Syst. Innov._ 2017, 386–388 (2017). Google Scholar * Qian, Q. _et al._ Distal versus
proximal—an investigation on different supportive strategies by robots for upper limb rehabilitation after stroke: A randomized controlled trial. _J. Neuroeng. Rehabil._ 3, 64 (2019).
Article Google Scholar * Bohannon, R. W. & Smith, M. B. Interrater reliability of a modified Ashworth scale of muscle spasticity. _Phys. Ther._ 67, 206–207 (1987). Article CAS PubMed
Google Scholar * Platz, T. _et al._ Reliability and validity of arm function assessment with standardized guidelines for the Fugl-Meyer Test, Action Research Arm Test and Box and Block
Test: A multicentre study. _Clin. Rehabil._ 19, 404–411 (2005). Article PubMed Google Scholar * Williamson, A. & Hoggart, B. Pain: A review of three commonly used pain rating scales.
_J. Clin. Nurs._ 14, 798–804 (2005). Article PubMed Google Scholar * Colombo, R. _et al._ Comparison of exercise training effect with different robotic devices for upper limb
rehabilitation: A retrospective study. _Eur. J. Phys. Rehabil. Med._ 53, 240–248 (2017). PubMed Google Scholar Download references FUNDING This work was partially supported by the “Ricerca
Corrente” funding provided by the Italian Ministry of Health. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Istituti Clinici Scientifici Maugeri, I.R.C.C.S., Istituti Clinici Scientifici
Maugeri, Music Therapy Research Laboratory, Scientific Institute of Pavia , Via Maugeri 10, 27100, Pavia, Italy Alfredo Raglio, Monica Panigazzi, Roberto Colombo, Paola Baiardi, Daniele
Molteni, Chiara Imbriani, Chiara Imarisio & Marcello Imbriani * Fondazione S. Lucia, I.R.C.C.S., Rome, Italy Marco Tramontano, Marco Iosa, Sara Mastrogiacomo & Carlo Caltagirone *
Istituti Clinici Scientifici Maugeri, I.R.C.C.S., Nervi (GE), Pavia, Italy Eleonora Baldissarro & Caterina Pistarini * Neurological Clinic, S. Martino Hospital, University of Genoa,
Genoa, Italy Mehrnaz Hamedani & Gian Luigi Mancardi * Istituti Clinici Scientifici Maugeri, I.R.C.C.S, Montescano, PV, Italy Laura Eretti Authors * Alfredo Raglio View author
publications You can also search for this author inPubMed Google Scholar * Monica Panigazzi View author publications You can also search for this author inPubMed Google Scholar * Roberto
Colombo View author publications You can also search for this author inPubMed Google Scholar * Marco Tramontano View author publications You can also search for this author inPubMed Google
Scholar * Marco Iosa View author publications You can also search for this author inPubMed Google Scholar * Sara Mastrogiacomo View author publications You can also search for this author
inPubMed Google Scholar * Paola Baiardi View author publications You can also search for this author inPubMed Google Scholar * Daniele Molteni View author publications You can also search
for this author inPubMed Google Scholar * Eleonora Baldissarro View author publications You can also search for this author inPubMed Google Scholar * Chiara Imbriani View author publications
You can also search for this author inPubMed Google Scholar * Chiara Imarisio View author publications You can also search for this author inPubMed Google Scholar * Laura Eretti View author
publications You can also search for this author inPubMed Google Scholar * Mehrnaz Hamedani View author publications You can also search for this author inPubMed Google Scholar * Caterina
Pistarini View author publications You can also search for this author inPubMed Google Scholar * Marcello Imbriani View author publications You can also search for this author inPubMed
Google Scholar * Gian Luigi Mancardi View author publications You can also search for this author inPubMed Google Scholar * Carlo Caltagirone View author publications You can also search for
this author inPubMed Google Scholar CONTRIBUTIONS A.R. designed the experiment and the protocol, provided music therapy expertise, interpreted the results, and prepared the manuscript.
S.M., C.I., L.E. and M.H. performed the experiments. M.P., M.T., E.B. and C.P. provided clinical support and supervision. P.B. performed statistical analysis. R.C. and M.I. provided
engineering support and contributed to prepare the manuscript. D.M. and C.I. provided music and music technology expertise. M.I., G.M. and C.C. contributed to data interpretation and
critical reading/revision of the manuscript. All authors have read and approve of the final manuscript version. CORRESPONDING AUTHOR Correspondence to Alfredo Raglio. ETHICS DECLARATIONS
COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published
maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION 1. SUPPLEMENTARY INFORMATION 2. Supplementary Video 1. Supplementary Video 2. RIGHTS AND PERMISSIONS
OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or
format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or
other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not
included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission
directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Raglio,
A., Panigazzi, M., Colombo, R. _et al._ Hand rehabilitation with sonification techniques in the subacute stage of stroke. _Sci Rep_ 11, 7237 (2021).
https://doi.org/10.1038/s41598-021-86627-y Download citation * Received: 03 September 2020 * Accepted: 17 March 2021 * Published: 31 March 2021 * DOI:
https://doi.org/10.1038/s41598-021-86627-y SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative







