- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT HDL-Cholesterol (HDL-C) is not an accurate surrogate marker to measure the cardioprotective functions of HDL in coronary artery diseases (CAD) patients. Hence, measurement of other
HDL-related parameters may have prognostic superiority over HDL-C. In this work, we examined the predictive value of HDL particles profile for long-term mortality in CAD patients and to
compare its informative value to that of HDL-C and apoA-I. HDL particles profiles were measured by nuclear magnetic resonance (NMR) spectroscopy in 214 male participants with stable CAD
(45–74 years). Median follow up was 12.5 years with a 36.4% mortality rate. Cardiovascular mortality accounted for 64.5%. Mean concentrations of total HDL particles (HDL-P), small-sized HDL
(SHDL-P) and apoA-I were lower in deceased than in surviving patients whereas no difference was observed according to HDL-C and large HDL particles. All NMR-HDL measures were correlated
between themselves and with other HDL markers (HDL-C, apoA-I and LpA-I). In a multivariate model adjusted for cardiovascular risk factors and bioclinical variables, HDL-P and SHDL-P
displayed the strongest inverse association with all-cause and cardiovascular mortality. Weaker associations were recorded for apoA-I. Based on our results, we conclude that HDL particle
profile measured by NMR spectroscopy should be considered to better stratify risk in population at high risk or in the setting of pharmacotherapy. SIMILAR CONTENT BEING VIEWED BY OTHERS
HIGH-SENSITIVITY CRP MAY BE A MARKER OF HDL DYSFUNCTION AND REMODELING IN PATIENTS WITH ACUTE CORONARY SYNDROME Article Open access 01 June 2021 PARTICLE SIZE AND CHOLESTEROL CONTENT OF
CIRCULATING HDL CORRELATE WITH CARDIOVASCULAR DEATH IN CHRONIC HEART FAILURE Article Open access 04 February 2021 TRIGLYCERIDES AND LOW HDL CHOLESTEROL PREDICT CORONARY HEART DISEASE RISK IN
PATIENTS WITH STABLE ANGINA Article Open access 20 October 2021 INTRODUCTION HDL-Cholesterol (HDL-C) has been repeatedly inversely related to cardiovascular risk in all epidemiological
studies. However, pharmacological trials aimed at increasing HDL-C have failed to demonstrate a beneficial effect on clinical outcomes1. Also, some genetic variants associated to increased
HDL-C have not been found associated to a decreased cardiovascular risk2 but those HDL randomization studies are questionable because they disregarded the complexity of lipoprotein
metabolism by excluding from their analyses important genes that not exclusively regulate HDL-C levels but also those of other lipoproteins3,4. This has led to the concept that a single
measurement of HDL-C does not necessarily reflect the functional properties of HDL particles and their effects against atherosclerosis. Indeed, HDL particles are heterogeneous in size and
biochemical composition, and HDL subpopulations might have different functional properties5. NMR-spectroscopy has been recently proposed as a tool to quantify HDL particles and HDL
subpopulations5. This technology enables to measure the total concentration of HDL particles and their size distribution. Numerous recent studies have shown that the atheroprotective
properties of HDL are supported by small and medium-sized HDL particles6, which were inversely related to cardiovascular risk in various clinical settings7,8. In the present study, we have
evaluated HDL particles concentration and distribution in a cohort of patients with established, angiographically documented, coronary artery disease9,10 taking into account an extended
panel of potential confounders related to cardiovascular risk and heart condition. The patients’ vital status was yearly assessed and mortality was recorded, distinguishing all-cause
mortality, cardiovascular mortality and other causes of death, during a 12.5-year median follow-up. In addition, one objective of the study was to compare HDL particles measurements to
routinely available HDL markers, HDL-C and apoA-I, as predictors of mortality in CAD patients. Indeed, apoA-I is the major HDL protein, its immunoassay is today referred to international
standards and now available on automated analyzers. Moreover apoA-I is much less influenced than HDL-C by other components of the lipoprotein profile, like VLDL or LDL, which may have an
impact on HDL lipid composition through action of lipid transfer proteins. RESULTS CHARACTERISTICS OF CAD PATIENTS ACCORDING TO VITAL STATUS The present cohort was constituted of 214 CAD
male patients. After inclusion, the vital patients’ status was yearly assessed. The median follow-up period was 12.5 years (mean: 10.7 years). During follow-up, 78 deaths had been recorded
giving a death rate of 36.4% and a mean annual rate of 3.4%. Cardiovascular mortality accounted for the majority of deaths recorded (64.1%, n = 50) and cancers accounted for 16.7% (n = 13).
Comparison of patients’ data when they were included in the cohort is given in Table 1. Results are presented distinguishing two groups: the “alive group” (patients living at the end of the
follow-up) and the “deceased group” (patients who died during follow-up). Hypertension was diagnosed or treated in 65.6% patients (45.5% under treatment) with no difference between the
deceased and alive groups (p = 0.95). Dyslipidemia was diagnosed or treated in 71.3% (65.4% treated) of the alive group, and in 50.6% (43.6% upon treatment) of the deceased group and the
difference was statistically significant (p = 0.002). Among patients treated for dyslipidemia, 87.8% were treated with statins, 16.2% with fibrates, 4% with both statins and fibrates and
none were treated with niacin or other lipid-lowering therapy. Diabetes was diagnosed in 18.7% (16.9% treated) of the alive group and in 41.8% (37.2% upon treatment) of the deceased group
and the difference was statistically significant (p = 0.001). Patients having deceased during the follow-up period had a longer duration of CAD, a decreased left ventricle ejection volume
(LVEF), a higher heart rate and a more severe angiographic lesion score (Gensini). Regarding cardiovascular risk factors, smoking habits and treatment for diabetes were more frequent in the
deceased group, whereas lipid-lowering therapy was less frequent. Among lipoprotein parameters, only apoA-I, a major HDL marker, was significantly lower in further deceased patients. Hs-CRP,
an inflammatory marker, was lower in surviving than in deceasing patients. NT-proBNP levels were significantly higher in further deceased patients but no difference was observed in the
concentration of hs-TnT between the two groups, indicating that deceased patients suffered from a more severe myocardial dysfunction rather than from a more extended myocardial necrosis. The
distribution of prior cardiovascular events in the studied population of stable CAD patients is shown in Supplementary Table 1. The majority is represented by myocardial infarction (MI,
52.3%), followed by revascularization procedures (37.9%) and then by other ischemic heart disease (IHD, 9.8%, _e.g_. stable angina). Logically, among patients deceased during follow-up, past
history of MI and other IHD were more frequent than in alive patients. HDL PARTICLES ACCORDING TO VITAL STATUS HDL particles’ profile was determined by NMR spectroscopy, enabling to
distinguish large HDL (LHDL-P, 8.8–13 nm) and small-sized HDL (SHDL-P, 7.3–8.7 nm) particles. The latter accounted for about ∼85% of total HDL particles (HDL-P). HDL-P was ∼10% lower in
deceased than in surviving patients (24.6 μmol/L [SD, 6.0] vs. 27.5 μmol/L [SD, 4.9], p = 0.001, Table 2). This difference was entirely due to a decreased number of SHDL-P, whereas number
LHDL-P was not different according to the vital status (Table 2). The average size of total HDL particles (HDL size) was found higher in deceased patients (8.94 nm _versus_ 8.82 nm, p =
0.014). CORRELATIONS BETWEEN HDL PARTICLES MEASURES AND CLINICAL AND BIOLOGICAL PARAMETERS Correlations were investigated between markers of HDL particles and other clinical or biological
parameters in the study population (Table 3). All NMR-HDL measures were correlated between themselves and with other HDL markers: HDL-C, apoA-I and lipoprotein A-I (LpA-I). Logically, the
average HDL size was correlated positively with the number of LHDL-P, and negatively, with the number of SHDL-P. Triglycerides were associated positively with HDL-P and SHDL-P but negatively
with LHDL-P, mean HDL size and HDL-C. No association was observed with apoA-I. These correlations might reflect the remodeling of HDL lipids induced by the cholesterol ester transfer
protein (CETP) acting between HDL particles and triglyceride-rich lipoproteins. Alcohol consumption positively correlated with HDL-C and HDL-P, and more specifically with SHDL-P but not with
apoA-I. Inflammation, as documented by plasma hs-CRP, was inversely associated with apo A-I, HDL-P and SHDL-P, but not with LHDL-P. HDL-P, SHDL-P and apoA-I were negatively associated with
NT-proBNP and hs-TnT. The severity of coronary lesions, as illustrated by the Gensini score, was inversely related to HDL-P. Strong positive associations were observed between LVEF and both
HDL-P and SHDL-P. ApoA-I levels correlated with LVEF but not significantly with the Gensini score. For comparison, no relationship was recorded between HDL-C and either LVEF or the Gensini
score. Thus, although HDL markers were strongly correlated between themselves, total and subclasses of HDL particles displayed specific association with clinical variables. TOTAL AND
CARDIOVASCULAR MORTALITY ACCORDING TO TERTILES OF HDL MARKERS Each one HDL marker was considered according to tertiles of its distribution in the whole study population (Table 4). Death
rates during follow-up were determined across the different tertiles and associations were determined after adjustment on classical risk factors including age, smoking and treatments for
hypertension, diabetes and dyslipidemia. Similar associations were observed without adjustment. The strongest association to total and cardiovascular mortality was observed for HDL-P
distribution. A 45% reduction in death rates was recorded in tertiles 2 and 3, as compared to tertile 1. Each 1 SD increase in HDL particles number was found associated with ∼42% reduction
in total or cardiovascular mortality (HR = 0.58 [95% CI, 0.45–0.75] and 0.59 [95% CI, 0.44–0.80], respectively). Results were almost identical considering SHDL-P (HR = 0.60 [95% CI,
0.46–0.77] and 0.61 [95% CI, 0.45–0.82], respectively). Taking into account fibrate and/or statin use in statistical analyses had no effect on the association of HDL-P and SHDL-P particles
with mortality (not shown). By contrast, no association between LHDL-P and mortality was observed, except for an almost significant positive trend (p = 0.07) between LHDL-P and death rates.
Concordantly, death rates were significantly different across HDL size distribution, an increase in particles size being associated with highest death rates. Considering classical HDL
markers, HDL-C tertiles did not display different death rates, yet a 1 SD increase in HDL-C was associated with a significantly lower HR for total mortality (0.78, p = 0.03). ApoA-I
distribution was associated to total and cardiovascular mortality; each 1 standard deviation increase of apoA-I was associated to a ∼31% risk reduction (HR = 0.69 [95% CI, 0.54–0.88] and
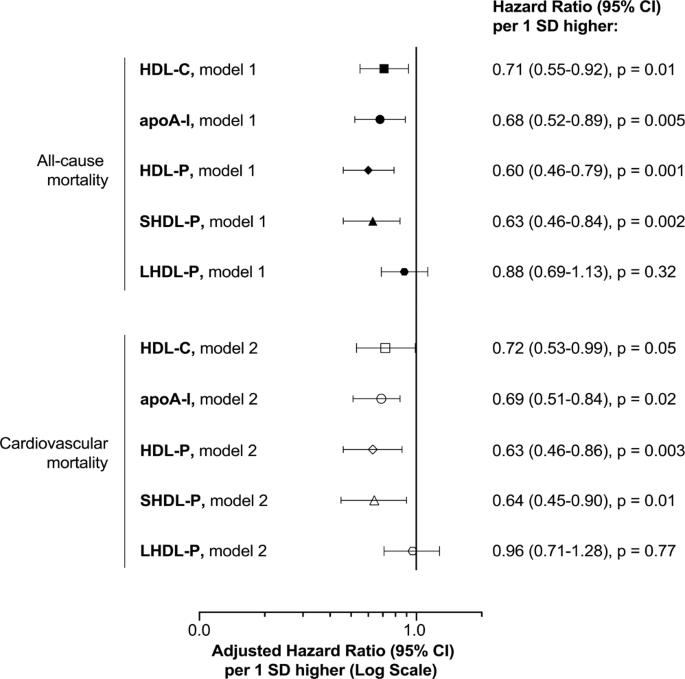
0.67 [95% CI, 0.49–0.91], respectively). A further multivariate analysis was conducted using a forward stepwise selection of adjustment variables (Fig. 1). Regarding total mortality, the
variables retained in the model were age, smoking, treatment for dyslipidemia, renal function (eGFR), LVEF, duration of CAD and Gensini score, the 3 last parameters reflecting heart
condition. For cardiovascular mortality, similar variables were retained except for age, smoking and eGFR. Hazard ratios for mortality per 1-SD increase of HDL-P, SHDL-P, of apoA-I and HDL-C
were all significant (Fig. 1). HR were almost identical for all-cause and CV mortality (Fig. 1). They were the lowest for HDL-P or total and cardiovascular mortality (HR = 0.60 [95% CI,
0.46–0.79] and HR = 0.63 [95% CI, 0.46–0.86], respectively) and the highest and at the limit of significance for HDL-C (HR = 0.71 [95% CI, 0.55–0.92] and HR = 0.72 [95% CI, 0.53–0.99]
respectively). Intermediate values of HR were found for apoA-I. Associations between HDL markers and mortality are illustrated in the survival curves established during the whole follow-up
period for the different tertiles (Fig. 2). Death rates were regular during the whole time course of follow-up. For both HDL-P and SHDL-P, patients in the first tertile had a poorer survival
than patients in tertiles 2 and 3. This was particularly evident for early events: of the 17 deaths recorded during the 0–3 year follow-up, 11 (65%) were in the lowest tertile of HDL-P as
compared to 8 out of 20 (40%) for the deaths recorded in the 9–12 year period. A comparable trend was observed for apoA-I distribution yet survival differences during the whole period did
not reach statistical significance. DISCUSSION In the present study, serum levels of total HDL particles (HDL-P) and of small-sized HDL particles (SHDL-P) were inversely related to all-cause
as well as to specific cardiovascular mortality in CAD patients. Every 1-SD increase of HDL particle number was associated to a 41% decrease in cardiovascular mortality, after multiple
adjustments on cardiovascular risk factors and on clinical markers of heart condition, including LVEF, duration of CAD and Gensini score. Among other HDL markers, apoA-I was also inversely
related, though to a lesser extent, to total and cardiovascular mortality, and HDL-C was found weakly associated to all-cause mortality. Conversely, large HDL particles (LHDL-P) were not
associated with total and cardiovascular mortality. However, higher death rates were recorded as average HDL particle size increased. NMR-based lipoprotein profiling methods are not yet
standardized and the estimated diameter range of HDL subclasses depends on the analytical methods used. Also, no classification for HDL subclasses analysed by NMR has been yet approved for
routine purpose. For instance, the analytical method developed by LipoScience (now LabCorp, Raleigh, NC) grouped HDL particles into 3 subclasses from small (S-HDL-P, 7.3–8.2 nm), medium
(M-HDL-P, 8.2–9.4 nm) to large (L-HDL-P, 9.4–14 nm) with small and medium-sized HDL particles being sometimes grouped (MS-HDL-P, 7.3–9.4 nm), while the AXINON lipoFIT-S100 system (Numares
AG, Regensburg, Germany) used in the present study grouped HDL subclasses into small (SHDL-P, 7.3–8.7 nm) and large (LHDL-P, 8.8–13 nm)11,12. In this latest classification, it is worth
mentioning that the estimated diameter ranges for SHDL-P and LHDL-P were similar to those for HDL3c+3b+3a (7.2–7.8 nm; 7.8–8.2 nm; 8.2–8.8 nm) and HDL2a+2b (8.8–9.7 nm; 9.7–12.9 nm),
respectively, as isolated from plasma by density gradient ultracentrifugation and analyzed by electrophoresis on a nondenaturing gel13,14. To date, the inverse and independent association
between HDL-P / MS-HDL-P and cardiovascular risk has been extensively documented with respect to primary prevention, either in individuals without baseline CAD7,15,16,17,18 and in those with
pre-clinical atherosclerosis, as documented by carotid intima-media thickness7,19, or coronary calcifications20. More recently, in a large study carried out in high-risk individuals
undergoing coronary catheterization for suspicion of CAD, followed-up during 8 years, HDL-P and MS-HDL-P were independent predictors of all-cause mortality8. With respect to secondary
prevention, only a few studies have evaluated the relationship of NMR-derived HDL particle subclasses with cardiovascular disease outcomes in CAD patients. In a prospective nested
case-control study of 364 men with new CAD events (non-fatal myocardial infarction or cardiac death) during a 5.1 year follow-up paired to 697 age-matched control, total HDL-P and small
HDL-P (7.3–8.2 nm) were strong, independent, predictors of recurrent coronary events, whereas levels of HDL-C were not21. Similarly, inverse association between HDL-P and coronary events has
also been reported in a large mixed-gender cohort of CAD patients during a 5.3 years of follow up22. In patients suffering from acute heart failure, concentrations of both HDL-P and small
HDL-P (7.3–8.7 nm) were inversely related to short-term (3-month) mortality, after multiple adjustments on confounding variables, including NT-proBNP, a classical marker of heart failure23.
The present study brings some additional insights on this relation between NMR-derived HDL particles subclasses and long-term prognosis in CAD patients, with angiographically documented
coronary lesions. Association of HDL markers to all-cause and cardiovascular mortality was assessed after adjustment on a large variety of confounders: life-style parameters, clinical and
biological variables documenting cardiovascular risk factors, inflammatory status, renal function and heart condition. In addition, this study has enabled to compare the predictive value of
apoA-I versus HDL-P measurements, which showed comparable associations, although Hazard ratios were better with HDL-P levels. HDL particles, and most particularly small-sized HDL, may act
against atherosclerosis through different mechanisms. Small HDL behave as the best acceptors of ABCA1-mediated cholesterol efflux from macrophages, leading subsequently to the mobilization
of intracellular cholesterol to the plasma membrane24,25. Small and dense HDL particles also protect LDL from oxidation. HDL particles act through removing phospholipid hydroperoxides from
LDL and by inactivating oxidized lipids by specific enzymes like paraoxonase-1 (PON-1) and PAF-acetylhydrolase26,27. Moreover small protein-rich HDL exert anti-inflammatory properties by
depressing expression of VCAM-1 at the surface of endothelial cells28. On these cells, HDL particles appear to be cytoprotective by inhibiting apoptosis induced by oxidized LDL, and small
HDL3 would be the most effective in this function29. Altogether those observations suggest that the proteome associated to small HDL particles support various biological activities, which
impair atherosclerosis development. Moreover, HDL particles may exert beneficial effects on myocardial functions. Indeed, in different experimental contexts, it was demonstrated that HDL
particles protect against ischemia reperfusion injury30, leading to a reduction in infarct size. HDL may also improve myocardial function by reducing ventricular remodelling following
infarction31. In isolated cardiomyocytes, HDL particles were shown to prevent apoptosis through an AMP-kinase dependent mechanism32. These experimental observations on a direct impact of HDL
on myocardial functions might translate into clinical impacts. In support of this concept is the positive correlation observed here between HDL-P, small HDL-P and the left ventricular
ejection fraction, concordant with the negative association between HDL-P, small HDL-P and NT-proBNP observed here and previously reported23, although potential confounders might interfere
with these associations. In this study, concentrations of large HDL particles were not associated to mortality. However, higher death rates were recorded as HDL size increased (p < 0.01);
following multiple adjustments, association to total mortality for the upper tertile of HDL size was close to statistical significance (p = 0.06). Similar observations regarding all-cause
mortality in individuals who are at high cardiovascular risk have been previously reported8. Large HDL-P might be less effective than SHDL-P regarding various atheroprotective functions,
like cholesterol efflux, anti-oxidative and anti-inflammatory properties, and cytoprotective effects on endothelium6,33. Moreover, accumulation of large HDL might reflect a defect in HDL
catabolism, and particularly in HDL liver uptake, which constitutes the last step of reverse cholesterol transport34. Similarly, we did not observe any association of HDL-C with mortality.
This is concordant with the lack of association between LHDL-P and mortality, since HDL-C mainly reflects cholesterol associated with large, lipid rich, HDL particles. ApoA-I was inversely
related to mortality: for each 1-SD increase of apoA-I, a 31% and 33% decrease in all-cause and cardiovascular mortality was recorded, respectively. So far, apoA-I has been little used in
epidemiological studies. However, calibration on reference international standards has made the immunoassay of apoA-I robust and comparable between studies. Furthermore, apoA-I measurement
is much less influenced than HDL-C by intravascular enzymes and lipid transfer proteins, which participate in HDL remodelling. Thus, apoA-I measurement may improve assessment of
cardiovascular risk35. Association to mortality was somewhat weaker for apoA-I than for HDL-P or SHDL-P. This might be explained by the fact that the apoA-I content per particle varies on
average from 2 to 4, between small HDL3 and large HDL2 36, so that large HDL particles are somewhat overrepresented in apoA-I quantification. A number of limitations of the present study
must be noted. First, the small size of the study is a limitation. Indeed, the first 214 consecutive CAD patients from the GENES cohort where included in the present study, which represent
25% of the whole cohort (n = 834). Accordingly, mortality rate was higher in included patients than in the whole cohort (36.4% _versus_ 29.1%, data not shown), probably because of the longer
duration of follow-up for those first included patients. Clinical and biological characteristics were comparable, between included and non-included patients, except for dyslipidemia
treatment, somewhat less frequent in included patients (57.5% vs 65.8%, p = 0.04, Supplementary Table 2). This difference might result from difference in statin administration practice
between the beginning (year 2001) and the end (2004) of the GENES study. Second, this study was designed only with men, which has the advantage of recording a larger number of events than in
a mixed all-gender cohort, particularly in south-western France where the incidence rates are particularly low for women under 65 years of age37 but limited the translatability of our
results to women. Third, despite adjustments on established CVD risk factors the possibility remains that other important confounding variables with effects on HDL parameters were not
measured or considered in our analyses. Finally, NMR-based HDL classification in large and small HDL particles provides limited insights into the biology of these complex particles, now
known to include more than 10 subspecies, for which proteome and lipidome compositions affect functional properties38. In particular the pre-beta HDL which are the principal acceptors for
cholesterol effluxed from the arterial wall39 are not accurately quantified by this method. Thus, comparison with other methods of analysis of HDL subfractions40 would be relevant to confirm
our findings and to improve our understanding of HDL functions. In conclusion, the present study demonstrated that the concentration of total HDL particles and small-sized HDL particles may
serve as a better prediction tool than HDL-C and apoA-I to assess long term prognosis in coronary patients. Studies on HDL metabolism had progressively led to the schematic view of an
interconversion cycle of HDL particles in the plasma compartment, driven by cell cholesterol efflux, enzymes like LCAT, lipases and lipid transfer proteins41,42. More recently the concept
has emerged that HDL particles of different geometry and chemical composition have distinct metabolic fate and display specific functional properties5,6,43. This supports the idea that HDL
functionality might be more precisely assessed by the quantification of specific HDL particles with high atheroprotective effects. In the future, quantification of HDL particle concentration
and HDL subclasses along with HDL functional measurement could be clinically useful in CVD risk assessment. METHODS STUDY PARTICIPANTS The “Génétique et Environnement en Europe du Sud”
(GENES) study is a case-control study designed to assess the role of genetic, biological and environmental determinants in the occurrence of CAD44. Written informed consent was obtained from
all participants, and the study protocol was conducted in accordance with the Helsinki Declaration and approved by the local ethics committee (Comité consultatif de protection des personnes
dans la recherche biomédicale (CCPPRB), Toulouse/Sud-Ouest, file #1-99-48, Feb 2000). All research was performed in accordance with procedures and regulations at the Toulouse University
Hospital. A blood sample collection has been constituted (declared as DC-2008-463 #1 to the Ministry of Research and to the Regional Health Authority). As previously described, cases were
stable male CAD patients living in the Toulouse area (South-west France), aged 45–74 and prospectively recruited from 2001 to 2004 after admission to the Cardiology department, Toulouse
University Hospital, for cardiovascular examination and referred for evaluation and management of their CAD45. Patients included in the present study presented a stable CAD that was defined
by a previous history of acute coronary syndrome, a previous history of coronary artery revascularization, a stable angina or a documented myocardial ischemia, as assessed by presence of
coronary stenosis of ≥50% of luminal narrowing at the coronary angiography. Patients who had presented an acute coronary episode in the seven days prior to the recruitment were not included
in the study, because they were considered unstable. In the present analysis, we only took into account the first 214 consecutive patients (i.e. those with CAD) in whom NMR-HDL profile was
measured and complete data were available for all the subjects. The minimal sample size (n = 186), increased by 15% to take into account missing data, was calculated to detect a HR of 0.8
(for one SD increase of HDL-C) with a 80% power at a 0.05 significance level. The sample size was adjusted for an anticipated event rate of ∼35% corresponding to a median follow-up of 12.5
years. ASSESSMENT OF THE VITAL STATUS Vital status was obtained for each participant through the national database (“RNIPP”), which records, every year, all deaths occurring in the French
population (http://cesp.vjf.inserm.fr/svcd). For each patients, vital status was assessed yearly from the year of recruitment until December 31, 2014, with a median follow up of 12.5 years.
All dates and causes of death were obtained for participants who died during the follow-up. Main and associated causes of deaths were provided by the French National Institute of Health
Research (CépiDc-INSERM), which systematically collects and codes (using the International Classification of Diseases coding system) data recorded on death certificates. Death from a
cardiovascular cause during follow-up was assessed by a committee of four medical doctors, every time cardiovascular disease was reported as the main cause of death, or when it was mentioned
as an associated cause, if the main cause was a plausible complication of cardiovascular disease. Authorizations to use these data were obtained in accordance with French law (Commission
nationale de l’informatique et des libertés (CNIL): authorization 355152v1, September 3, 2008). BIOLOGICAL MEASUREMENT Blood was collected after an overnight fast. Serum sample aliquots were
subsequently stored at −80 °C until biological analyses. The following biomarkers were assayed with enzymatic reagents on automated analyzers (Hitachi 912 and Cobas 8000, Roche Diagnostics,
Meylan, France): serum total cholesterol, HDL-C, triglycerides, fasting glucose, creatinin. eGFR was calculated using the abbreviated Modification of Diet in Renal Disease (MDRD) Study
equation46. ApoA-I, high-sensitive C-Reactive protein (hs-CRP), N-terminal pro-brain natriuretic peptide (NT-proBNP) and high-sensitive cardiac troponin T (hs-TnT) were determined on the
same analyzer by immunoturbidimetry assays (Roche Diagnostics). Lipoprotein A-I, which refers to lipoproteins containing apoA-I but not apoA-II, were measured by an electroimmunodiffusion
technique47 using the HYDRAGEL LPAI PARTICLES Kit (Sebia, Issy-les-Moulineaux, France). DATA COLLECTION Age, environmental characteristics and information on cardiovascular risk factors were
collected through standardized face-to-face interviews, performed by a single physician. Past medical history was collected and checked in the patients’ medical files. Presence of
dyslipidemia, diabetes mellitus or hypertension was assessed from the subjects’ current treatments. Dyslipidemia was defined as treatment with drugs or fasting serum total cholesterol ≥2.40
g/L. Hypertension was defined as treatment with drugs or systolic blood pressure ≥160 mmHg or diastolic blood pressure ≥95 mmHg. Diabetes was defined as treatment with drugs or fasting blood
glucose ≥7.8 mmol/L. Smoking status was classified as current smokers, past smokers having quit for more than 3 years and patients having never smoked. Among current smokers, cigarette
consumption was estimated with the pack-year quantification and recorded as the average number of cigarettes per day. Alcohol consumption was assessed using a typical week pattern. The total
amount of pure alcohol consumption was calculated as the sum of different types of drinks and was expressed as grams per day. Physical activity was investigated through a standardized
questionnaire48 and categorized into three levels as: no physical activity, moderate physical activity during 20 minutes no more than once a week, and high physical activity during 20
minutes, at least twice a week. Blood pressure and resting heart rate were measured with an automatic sphygmomanometer (OMRON 705 CP). Measurements were performed after a minimum of 5
minutes rest; average values from two different measurements were recorded for further analysis. ASSESSMENT OF CAD SEVERITY AND EXTENSION AND ESTIMATION OF CARDIAC FUNCTION All stable CAD
patients enrolled had a coronary angiography even without evidence of active chronic ischemia. Coronary artery stenoses of ≥50% luminal narrowing were considered significant. Extent of
coronary artery disease lesions was assessed by calculating the Gensini Score, based on data from coronary angiography49,50,51. Left Ventricular Ejection Fraction (LVEF) was assessed by
contrast ventriculography using an isotopic method, and/or by echocardiography. HDL MEASUREMENT BY NUCLEAR MAGNETIC RESONANCE (NMR) SPECTROSCOPY HDL particle concentration and size were
measured by NMR spectroscopy using the AXINON lipoFIT-S100 test system (Numares AG, Regensburg, Germany) as previously described11,12,23. Serum samples for NMR spectroscopy were stored at
−80 °C and kept unthawed until the day of NMR measurements. Serum (630 μL) gently mixed with 70 μL of an additives solution containing reference substances, NaN3 and D2O, and 600 μL of the
mixture were transferred into 5 mm NMR tubes with barcode-labeled caps. Briefly, 1H NMR spectra were recorded at a temperature of 310 K on a shielded 600 MHz Avance III HD NMR spectrometer
(Bruker Biospin) with a 5 mm triple resonance TXI probe head including deuterium lock channel, a z-gradient coil and automatic frequency tuning and matching. Prior to each analytical run,
calibration was performed using a calibration sample comprising an aqueous solution of various calibration substances with different molecular masses, 0.01% (w/v) NaN3, 10% (v/v) D2O as a
locking substance and 1% glycerol to adjust viscosity. Two identical control samples were measured directly after calibration and at the end of each run. Each spectrum was referenced,
normalized and subjected to a set of quality checks including checks of baseline properties, noise level, shift, width, and symmetry properties of quality control signals. Lipoprotein
analysis was conducted via deconvolution of the broad methyl group signal at about 0.9–0.8 ppm. In this process, lipoprotein subclasses are reflected by a fixed number of pre-defined
bell-shaped (e.g. Gaussian or Lorentzian) base functions, each of which has a constant position and defined width. The concentrations of lipoprotein particle subclasses as well as the
average particle size were calculated based on the integrals attributable to specific base functions. Fit quality was checked by calculating the residual deviation between fit and spectrum
intensity. In this study, the concentrations of large-sized HDL particles (LHDL-P), small-sized HDL-particle (SHDL-P) and total HDL particles (HDL-P, reported in μmol/L) as well as the
average HDL particle size (HDL size, reported in nm) are used. The two measured HDL subclasses had the following estimated diameter ranges: LHDL-P, 8.8–13 nm; SHDL-P, 7.3–8.7 nm. STATISTICAL
ANALYSES Continuous variables are displayed as means and standard deviations (SD). Categorical variables are presented as proportions. We first described and compared characteristics of
participants according to vital status. Categorical variables were compared between groups using the χ2-test (or Fisher’s exact test when necessary). Student’s _t_-test was used to compare
the distribution of continuous data. A Wilcoxon Mann-Whitney’s test (or logarithmic transformation of the variable when necessary) was performed when distribution departed from normality, or
when homoscedasticity was rejected. Spearman rank correlations were used to test the associations of NMR-HDL parameters and HDL-C with cardiovascular risk factors, severity, extension and
estimation of cardiac function of the disease. Cumulative survival of patients were determined by the Kaplan-Meier method and compared, using the Log-rank test for the individual endpoints
of all-cause mortality. The relation between baseline variables and mortality was assessed using Cox proportional hazards regression analysis. We tested the proportionality assumption using
cumulative sums of martingale-based residuals. We performed regression analyses with polynomial models (quadratic and cubic) to examine for possible non-linear relations between continuous
variables and mortality. Cox regression analyses were performed first without any adjustment for co-variables and, second, with adjustment on classical cardiovascular risk factors (age,
smoking, treatments for dyslipidemia, hypertension and diabetes). In addition, a forward stepwise selection was used to create the multivariate models. Variables with an entry criterion of p
≤ 0.20 were used as candidate covariates in a multivariate cox regression model. Variables were maintained in the model with a retention criterion of p ≤ 0.10 for all-cause of death
analyses and p ≤ 0.05 for cardiovascular mortality. The same covariates were identified for all HDL markers studied. The following variables were introduced into the model as covariates when
considering all cause of death: age, smoking, treatment for dyslipidemia, eGFR, LVEF, duration of CAD and Gensini score. For cardiovascular mortality the variables retained were treatment
for dyslipidemia, LVEF, duration of CAD and Gensini score. All statistical analyses were carried out using the SAS statistical software package 9.4 (SAS Institute, Cary, NC). Analyses were
two-tailed and p < 0.05 was considered to be significant. REFERENCES * Armitage, J., Holmes, M. V. & Preiss, D. Cholesteryl Ester Transfer Protein Inhibition for Preventing
Cardiovascular Events: JACC Review Topic of the Week. _J. Am. Coll. Cardiol._ 73, 477–487 (2019). Article CAS PubMed PubMed Central Google Scholar * Voight, B. F. _et al_. Plasma HDL
cholesterol and risk of myocardial infarction: a mendelian randomisation study. _Lancet_ 380, 572–80 (2012). Article CAS PubMed PubMed Central Google Scholar * Geller, A. S. _et al_.
Genetic and secondary causes of severe HDL deficiency and cardiovascular disease. _J. Lipid Res._ 59, 2421–2435 (2018). Article CAS PubMed PubMed Central Google Scholar * Schaefer, E.
J., Geller, A. S. & Endress, G. The biochemical and genetic diagnosis of lipid disorders. _Curr. Opin. Lipidol._ 30, 56–62 (2019). Article CAS PubMed Google Scholar * Kontush, A. HDL
particle number and size as predictors of cardiovascular disease. _Front. Pharmacol._ 6, 218 (2015). Article PubMed PubMed Central CAS Google Scholar * Camont, L., Chapman, M. J. &
Kontush, A. Biological activities of HDL subpopulations and their relevance to cardiovascular disease. _Trends Mol. Med._ 17, 594–603 (2011). Article CAS PubMed Google Scholar * Mackey,
R. H. _et al_. High-density lipoprotein cholesterol and particle concentrations, carotid atherosclerosis, and coronary events: MESA (Multi-Ethnic Study of Atherosclerosis). _J. Am. Coll.
Cardiol._ 60, 508–516 (2012). Article CAS PubMed PubMed Central Google Scholar * McGarrah, R. W. _et al_. High-density lipoprotein subclass measurements improve mortality risk
prediction, discrimination and reclassification in a cardiac catheterization cohort. _Atherosclerosis_ 246, 229–235 (2016). Article CAS PubMed PubMed Central Google Scholar * Genoux, A.
_et al_. Serum levels of mitochondrial inhibitory factor 1 are independently associated with long-term prognosis in coronary artery disease: the GENES Study. _BMC Med._ 14, 125 (2016).
Article PubMed PubMed Central CAS Google Scholar * Verdier, C. _et al_. Common p2y polymorphisms are associated with plasma inhibitory factor 1 and lipoprotein(a) concentrations, heart
rate and body fat mass: The GENES study. _Arch. Cardiovasc. Dis._ 112, 124–134 (2019). Article PubMed Google Scholar * Hoeke, G. _et al_. Short-term cooling increases serum triglycerides
and small high-density lipoprotein levels in humans. _J. Clin. Lipidol._ 11, 920–928.e2 (2017). Article PubMed Google Scholar * Schettler, V. J. _et al_. NMR‐based lipoprotein analysis
for patients with severe hypercholesterolemia undergoing lipoprotein apheresis or PCSK9‐inhibitor therapy (NAPALI‐Study). _Ther. Apher. Dial._ 23, 467–473 (2019). Article CAS PubMed
Google Scholar * Blanche, P. J., Gong, E. L., Forte, T. M. & Nichols, A. V. Characterization of human high-density lipoproteins by gradient gel electrophoresis. _Biochim. Biophys. Acta_
665, 408–419 (1981). Article CAS PubMed Google Scholar * Rosenson, R. S. _et al_. HDL measures, particle heterogeneity, proposed nomenclature, and relation to atherosclerotic
cardiovascular events. _Clin. Chem._ 57, 392–410 (2011). Article CAS PubMed Google Scholar * Duprez, D. A. _et al_. High Density Lipoprotein Subclasses and Noncardiovascular, Noncancer
Chronic Inflammatory Related Events Versus Cardiovascular Events: The Multi Ethnic Study of Atherosclerosis. _J. Am. Heart Assoc._ 4, e002295 (2015). Article PubMed PubMed Central CAS
Google Scholar * El Harchaoui, K. _et al_. High-density lipoprotein particle size and concentration and coronary risk. _Ann. Intern. Med._ 150, 84–93 (2009). Article PubMed Google Scholar
* Kuller, L. H. _et al_. Lipoprotein particles, insulin, adiponectin, C-reactive protein and risk of coronary heart disease among men with metabolic syndrome. _Atherosclerosis_ 195, 122–8
(2007). Article CAS PubMed Google Scholar * Mora, S., Glynn, R. J. & Ridker, P. M. High-density lipoprotein cholesterol, size, particle number, and residual vascular risk after
potent statin therapy. _Circulation_ 128, 1189–97 (2013). Article CAS PubMed Google Scholar * Kim, D. S. _et al_. Concentration of Smaller High-Density Lipoprotein Particle (HDL-P) Is
Inversely Correlated With Carotid Intima Media Thickening After Confounder Adjustment: The Multi Ethnic Study of Atherosclerosis (MESA). _J. Am. Heart Assoc._ 5, e002977 (2016). PubMed
PubMed Central Google Scholar * Ditah, C. _et al_. Small and medium sized HDL particles are protectively associated with coronary calcification in a cross-sectional population-based
sample. _Atherosclerosis_ 251, 124–131 (2016). Article CAS PubMed Google Scholar * Otvos, J. D. _et al_. Low-density lipoprotein and high-density lipoprotein particle subclasses predict
coronary events and are favorably changed by gemfibrozil therapy in the veterans affairs high-density lipoprotein intervention trial. _Circulation_ 113, 1556–1563 (2006). Article CAS
PubMed Google Scholar * Parish, S. _et al_. Lipids and Lipoproteins and Risk of Different Vascular Events in the MRC/BHF Heart Protection Study. _Circulation_ 125, 2469–2478 (2012).
Article CAS PubMed Google Scholar * Potočnjak, I. _et al_. Serum Concentration of HDL Particles Predicts Mortality in Acute Heart Failure Patients. _Sci. Rep._ 7, 46642 (2017). Article
ADS PubMed PubMed Central CAS Google Scholar * Asztalos, B. F. _et al_. Differential effects of HDL subpopulations on cellular ABCA1- and SR-BI-mediated cholesterol efflux. _J Lipid
Res_ 46, 2246–2253 (2005). Article CAS PubMed Google Scholar * Du, X.-M. _et al_. HDL particle size is a critical determinant of ABCA1-mediated macrophage cellular cholesterol export.
_Circ. Res._ 116, 1133–42 (2015). Article CAS PubMed Google Scholar * Zerrad-Saadi, A. _et al_. HDL3-mediated inactivation of LDL-associated phospholipid hydroperoxides is determined by
the redox status of apolipoprotein A-I and HDL particle surface lipid rigidity: relevance to inflammation and atherogenesis. _Arterioscler. Thromb. Vasc. Biol._ 29, 2169–75 (2009). Article
CAS PubMed Google Scholar * Kontush, A. & Chapman, M. J. Antiatherogenic function of HDL particle subpopulations: focus on antioxidative activities. _Curr. Opin. Lipidol._ 21, 312–8
(2010). Article CAS PubMed Google Scholar * Rye, K.-A., Bursill, C. A., Lambert, G., Tabet, F. & Barter, P. J. The metabolism and anti-atherogenic properties of HDL. _J. Lipid Res._
50(Suppl), S195–200 (2009). Article PubMed PubMed Central CAS Google Scholar * de Souza, J. A. _et al_. Small, dense HDL 3 particles attenuate apoptosis in endothelial cells: pivotal
role of apolipoprotein A-I. _J. Cell. Mol. Med._ 14, 608–20 (2010). PubMed Google Scholar * Gomaraschi, M., Calabresi, L. & Franceschini, G. Protective Effects of HDL Against
Ischemia/Reperfusion Injury. _Front. Pharmacol._ 7, 2 (2016). Article PubMed PubMed Central CAS Google Scholar * Van Linthout, S., Frias, M., Singh, N. & De Geest, B. Therapeutic
potential of HDL in cardioprotection and tissue repair. _Handb. Exp. Pharmacol._ 224, 527–65 (2015). Article PubMed CAS Google Scholar * Spillmann, F. _et al_. High-density lipoproteins
reduce palmitate-induced cardiomyocyte apoptosis in an AMPK-dependent manner. _Biochem. Biophys. Res. Commun._ 466, 272–7 (2015). Article CAS PubMed Google Scholar * Camont, L. &
Chapman, J. & Kontush, a. Functionality of HDL particles: Heterogeneity and relationships to cardiovascular disease. _Arch. Cardiovasc. Dis. Suppl._ 3, 258–266 (2011). Google Scholar *
Martinez, L. O. _et al_. Ectopic beta-chain of ATP synthase is an apolipoprotein A-I receptor in hepatic HDL endocytosis. _Nature_ 421, 75–79 (2003). Article ADS CAS PubMed Google
Scholar * Sandhu, P. K. _et al_. Lipoprotein Biomarkers and Risk of Cardiovascular Disease: A Laboratory Medicine Best Practices (LMBP) Systematic Review. _J. Appl. Lab. Med._ 1, 214–229
(2016). Article CAS PubMed PubMed Central Google Scholar * Deckelbaum, R. J. _et al_. Conversion of human plasma high density lipoprotein-2 to high density lipoprotein-3. Roles of
neutral lipid exchange and triglyceride lipases. _J. Biol. Chem._ 261, 5201–8 (1986). CAS PubMed Google Scholar * Tunstall-Pedoe, H. _et al_. Myocardial infarction and coronary deaths in
the World Health Organization MONICA project: Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. _Circulation_,
https://doi.org/10.1161/01.cir.90.1.583 (1994). * Kajani, S., Curley, S. & McGillicuddy, F. C. Unravelling hdl—looking beyond the cholesterol surface to the quality within.
_International Journal of Molecular Sciences_ 19, 1971 (2018). Article PubMed Central CAS Google Scholar * Kane, J. P. & Malloy, M. J. Prebeta-1 HDL and coronary heart disease.
_Current Opinion in Lipidology_ 23, 367–371 (2012). Article CAS PubMed Google Scholar * Williams, P. T. _et al_. Comparison of four methods of analysis of lipoprotein particle
subfractions for their association with angiographic progression of coronary artery disease. _Atherosclerosis_ 233, 713–20 (2014). Article CAS PubMed PubMed Central Google Scholar *
Barrans, A. _et al_. Hepatic lipase induces the formation of pre-ß1 high density lipoprotein (HDL) from triacylglycerol-rich HDL2. _J. Biol. Chem._ 269, 11572–11577 (1994). CAS PubMed
Google Scholar * Collet, X. _et al_. Remodeling of HDL by CETP _in vivo_ and by CETP and hepatic lipase _in vitro_ results in enhanced uptake of HDL CE by cells expressing scavenger
receptor B-I. _J Lipid Res_ 40, 1185–93 (1999). CAS PubMed Google Scholar * Mendivil, C. O., Furtado, J., Morton, A. M., Wang, L. & Sacks, F. M. Novel Pathways of Apolipoprotein A-I
Metabolism in High-Density Lipoprotein of Different Sizes in Humans. _Arterioscler. Thromb. Vasc. Biol._ 36, 156–65 (2016). Article CAS PubMed Google Scholar * Hascoet, S. _et al_.
Adiponectin and long-term mortality in coronary artery disease participants and controls. _Arterioscler. Thromb. Vasc. Biol._ 33, e19–29 (2013). Article CAS PubMed Google Scholar *
Genoux, A. _et al_. Serum IF1 concentration is independently associated to HDL levels and to coronary heart disease: the GENES study. _J. Lipid Res._ 54, 2550–8 (2013). Article CAS PubMed
PubMed Central Google Scholar * Levey, A. S. _et al_. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet
in Renal Disease Study Group. _Ann. Intern. Med._ 130, 461–70 (1999). Article CAS PubMed Google Scholar * Parra, H. J., Mezdour, H., Ghalim, N., Bard, J. M. & Fruchart, J. C.
Differential electroimmunoassay of human LpA-I lipoprotein particles on ready-to-use plates. _Clin. Chem._ 36, 1431–1435 (1990). Article CAS PubMed Google Scholar * Roeykens, J. _et al_.
Validity and reliability in a Flemish population of the WHO-MONICA Optional Study of Physical Activity Questionnaire. _Med. Sci. Sports Exerc._ 30, 1071–5 (1998). Article CAS PubMed
Google Scholar * Gensini, G. G. A more meaningful scoring system for determining the severity of coronary heart disease. _Am J Cardiol_ 51, 606 (1983). Article CAS PubMed Google Scholar
* Califf, R. M. _et al_. Prognostic value of a coronary artery jeopardy score. _J. Am. Coll. Cardiol._ 5, 1055–63 (1985). Article CAS PubMed Google Scholar * Ducimetiere, P. _et al_.
Arteriographically documented coronary artery disease and alcohol consumption in French men. The CORALI Study. _Eur. Heart J._ 14, 727–33 (1993). Article CAS PubMed Google Scholar
Download references ACKNOWLEDGEMENTS This work was supported by the French National Research Agency (ANR, #ANR-16-CE18-0014-01), European Regional Development Fund (ERDF, Fonds Européen de
Développement Régional) and “La Région Occitanie” (Project THERANOVASC n° ESR_R&S_DF-000094/2018-003303/18009464). AUTHOR INFORMATION Author notes * These authors contributed equally:
Bertrand Perret and Laurent O. Martinez. AUTHORS AND AFFILIATIONS * Institut National de la Santé et de la Recherche Médicale (INSERM), UMR 1048, Institute of Metabolic and Cardiovascular
Diseases, Toulouse, France Thibaut Duparc, Annelise Genoux, Cécile Ingueneau, Souad Najib, Bertrand Perret & Laurent O. Martinez * University of Toulouse, UMR1048, Paul Sabatier
University, Toulouse, France Thibaut Duparc, Annelise Genoux, Cécile Ingueneau, Souad Najib, Bertrand Perret & Laurent O. Martinez * Department of Epidemiology, Health Economics and
Public Health, UMR1027 INSERM, Toulouse University, Toulouse University Hospital (CHU), Toulouse, France Jean-Bernard Ruidavets & Jean Ferrières * Service de Biochimie, Pôle biologie,
Hôpital de Purpan, CHU de Toulouse, Toulouse, France Annelise Genoux, Cécile Ingueneau & Bertrand Perret * Fédération de Cardiologie, Toulouse University Hospital, Toulouse, France Jean
Ferrières Authors * Thibaut Duparc View author publications You can also search for this author inPubMed Google Scholar * Jean-Bernard Ruidavets View author publications You can also search
for this author inPubMed Google Scholar * Annelise Genoux View author publications You can also search for this author inPubMed Google Scholar * Cécile Ingueneau View author publications You
can also search for this author inPubMed Google Scholar * Souad Najib View author publications You can also search for this author inPubMed Google Scholar * Jean Ferrières View author
publications You can also search for this author inPubMed Google Scholar * Bertrand Perret View author publications You can also search for this author inPubMed Google Scholar * Laurent O.
Martinez View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS Conception and design of the study: J.F., B.P., L.O.M.; acquisition of data, or
analysis and interpretation of data: T.D., J.B.R., A.G., C.I., S.N., L.O.M.; drafting the article or revising it critically for important intellectual content: A.G., J.B.R., J.F., L.M.,
B.P.; all Authors have read and approved the final version of the manuscript. CORRESPONDING AUTHOR Correspondence to Laurent O. Martinez. ETHICS DECLARATIONS COMPETING INTERESTS The authors
declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which
permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to
the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless
indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or
exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints
and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Duparc, T., Ruidavets, JB., Genoux, A. _et al._ Serum level of HDL particles are independently associated with long-term prognosis in
patients with coronary artery disease: The GENES study. _Sci Rep_ 10, 8138 (2020). https://doi.org/10.1038/s41598-020-65100-2 Download citation * Received: 10 December 2019 * Accepted: 27
April 2020 * Published: 18 May 2020 * DOI: https://doi.org/10.1038/s41598-020-65100-2 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get
shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative