- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Advanced cell therapies require robust delivery materials and silk is a promising contender with a long clinical track record. Our aim was to optimise self-assembling silk hydrogels
as a mesenchymal stem cell (MSC)-support matrix that would allow future minimally invasive brain application. We used sonication energy to programme the transition of silk (1–5% w/v)
secondary structure from a random coil to a stable β-sheet configuration. This allowed fine tuning of self-assembling silk hydrogels to achieve space conformity in the absence of any silk
hydrogel swelling and to support uniform cell distribution as well as cell viability. Embedded cells underwent significant proliferation over 14 days _in vitro_, with the best proliferation
achieved with 2% w/v hydrogels. Embedded MSCs showed significantly better viability _in vitro_ after injection through a 30G needle when the gels were in the pre-gelled versus post-gelled
state. Silk hydrogels (4% w/v) with physical characteristics matching brain tissue were visualised in preliminary _in vivo_ experiments to exhibit good space conformity in an ischemic cavity
(intraluminal thread middle cerebral artery occlusion model) in adult male Sprague-Dawley rats (n = 3). This study informs on optimal MSC-hydrogel matrix conditions for minimally invasive
application as a platform for future experiments targeting brain repair. SIMILAR CONTENT BEING VIEWED BY OTHERS BIOMIMETIC MICROENVIRONMENTAL PRECONDITIONING ENHANCE NEUROPROTECTIVE
PROPERTIES OF HUMAN MESENCHYMAL STEM CELLS DERIVED FROM WHARTON'S JELLY (WJ-MSCS) Article Open access 09 October 2020 NANO-SCAFFOLD CONTAINING FUNCTIONAL MOTIF OF STROMAL CELL-DERIVED
FACTOR 1 ENHANCES NEURAL STEM CELL BEHAVIOR AND SYNAPTOGENESIS IN TRAUMATIC BRAIN INJURY Article Open access 17 February 2025 ENGINEERING OF AN ELECTRICALLY CHARGED HYDROGEL IMPLANTED INTO A
TRAUMATIC BRAIN INJURY MODEL FOR STEPWISE NEURONAL TISSUE RECONSTRUCTION Article Open access 14 February 2023 INTRODUCTION Cell-based therapy, especially the use of stem cells, is one of
the main approaches that successfully promotes neurorestoration of function and improves outcomes such as angiogenesis, neuroprotection, immune response and modulated inflammation in
experimental models1. Stem cell therapy is now showing signs of success in human clinical trials2. For example, mesenchymal stem cells (MSCs) are appealing because these cells can be derived
from an autologous cell source and they promote the repair of neurovascular units and exert potent immunomodulatory functions that result in neurorestorative effects in experimental
models3. However, one key issue hindering the translation of cell therapies to the clinic is the lack of suitable cell delivery technologies that can support cell survival and provide
transplanted cells with the necessary cues to perform their intended restorative functions such as trophic factor production3,4. These support and cueing functions are normally provided by
the extracellular matrix (ECM), which is critical for the storage and presentation of growth and signalling factors and the provision of cell adhesion sites to guide and promote
proliferation and survival. Physical cues, such as substrate elasticity and surface topography, also direct stem cell lineage commitment5,6. Therefore, the ECM represents a critical
signalling hub that allows (stem) cells to respond to their environment. The ECM can be mimicked quite effectively by engineered hydrogels7,8; however, clinical translation of stem cell
therapies still requires the development of engineered materials to support function. Ideally, hydrogel materials should be biocompatible, biodegradable, minimally invasive, programmable
(i.e. solution-gel transition), cytocompatible and space conforming, and they should match brain tissue mechanics, show no material swelling and support even cell distribution (reviewed
in9,10). Many hydrogels presently being explored as carriers for cell therapies9,10 are derived from a broad spectrum of materials, including tissue-derived extracellular matrix, synthetic
polymers, biopolymers, peptides and hybrid materials (reviewed in11,12). Examples include heparin13 or hyaluronic acid14 polyethylene glycol hybrid hydrogels, self-assembling RADA (ref.15)
peptides functionalised with a laminin-derived IKVAV motif16, alginate hydrogels15 and self-healing chitosan hydrogels17. Other materials include extracted extracellular matrix from
Engelbreth-Holm-Swarm mouse sarcoma (i.e. Matrigel) or collagen from bovine or rodent tissues18. More recently, basement membrane and tunica propria ECM isolated from porcine urinary bladder
is emerging as an interesting alternative to existing ECM preparations19,20. All these systems have shown promise for brain repair, but these materials continue to show limitations.
Emerging evidence suggests that ECM tissue specificity is important for obtaining the desired treatment outcome21, so ECM extracts from tumours or tissues that are unrelated to the brain are
likely to require further optimisation. Single ECM component systems, such as collagen-based hydrogels, have been used extensively (reviewed in11), but these hydrogels have poor mechanical
properties, limited resistance to biodegradation (or ability to fine tune this) and a marked tissue response22. Collagen is also predominantly of bovine origin, so its use in the nervous
system raises theoretical risks of introducing prions directly into the brain. The development of biomimetic hydrogels (e.g. peptides, peptoids) and biohybrid hydrogel systems is promising,
although these systems still require significant research efforts to yield self-assembling hydrogels with sufficiently robust mechanical properties, _in vivo_ biocompatibility and the
desired performance12,23. The silk from _Bombyx mori_ has a long track record of use in humans24, as this biopolymer is clinically approved as a suture and surgical mesh25. Its renowned
mechanical properties26, biocompatibility and biodegradability27 make silk an ideal contender for applications that go beyond its current clinically approved load-bearing applications. The
silk fibre can be completely reverse engineered into an aqueous silk solution28, which can then be processed into many different formats, including physically cross-linked hydrogels. It also
has the ability to self-assemble in response to environmental triggers, making it particularly appealing for cell delivery applications (reviewed in29). Furthermore, silk is able to support
cell growth and cell differentiation of various stem cells, including pluripotent30, neural31,32 and MSC types33. Silk has therefore been investigated in a range of regenerative medicine
applications; however, at present, no studies have optimised self-assembling silk hydrogels-MSC conditions as a platform for future experiments on cell therapy into the brain. Towards that,
we hypothesized that _B. mori_ silk could be used to generate a delivery system suitable for (i) minimally invasive application (for example, stereotactic injection for intracerebral
delivery) and (ii) MSC support. For minimally invasive brain administration and stem cell support, the solution-gel characteristics and substrate elasticity are critical so we therefore
focussed on optimising the physical and chemical cues of self-assembling silk hydrogels for brain administration and stem cell support. Therefore the aim of the present study was to
fine-tune the processing parameters of self-assembling silk hydrogels to generate a delivery system that shows controllable solution-gel kinetics, elasticity, space conformity and
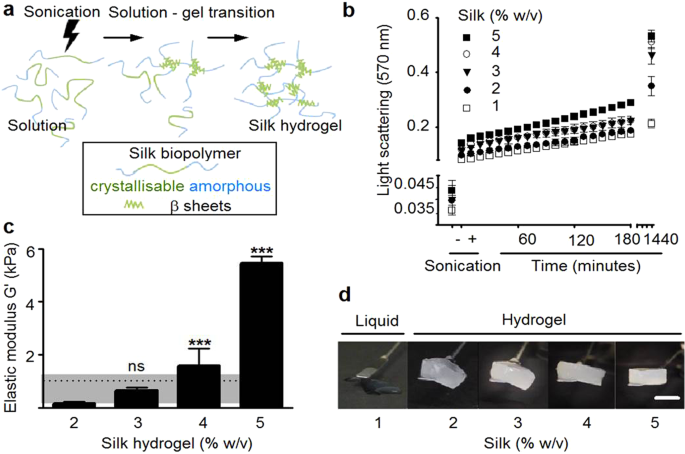
MSC-biocompatibility appropriate for administration to the brain. RESULTS PHYSICAL ASSESSMENT OF SELF-ASSEMBLING SILK HYDROGELS The solution-gel characteristics and elasticity of
self-assembling silk hydrogels were assessed because control of these parameters is critical for minimally invasive applications, including brain delivery. Silk self-assembly was initiated
by sonication energy (Fig. 1a) and the visible kinetics of silk nanocrystal formation was monitored by light scattering (Fig. 1b). For all silk concentrations, energy input increased light
scattering even at the first measurement point (i.e. within 10 minutes of energy input) when compared to the respective untreated silk solution controls. Over the subsequent 240 minutes,
light scattering increased in a linear fashion; at 24 hours, the silk hydrogels showed the highest light scattering properties over the time frame tested. The extent of light scattering
depended on the amount of silk present: the highest scattering values were observed for the 5% w/v hydrogels gels and lowest for 2% w/v hydrogels (note that 1% w/v silk did not form a robust
hydrogel). Increasing the amount of silk also significantly changed the rheological properties, which were used to estimate silk hydrogel elasticity (Fig. 1c). The lowest substrate
elasticity was observed for 2% w/v silk hydrogels and a near exponential increase was observed, from 0.17 to 5.46 kPa, for 2 and 5% w/v silk hydrogels, respectively. Visual inspection of the
silk hydrogels (Fig. 1d) supported the observations made by light scattering and rheological measurements. First, an increasing level of opaqueness (i.e. light scattering) was evident for 1
to 5% w/v silk samples (note that the liquid 1% w/v silk sample was also opaque). Second, the overall mechanical strength increased for the 2 to 5% w/v silk hydrogels, while 1% silk
remained liquid. STRUCTURAL ASSESSMENT OF SELF-ASSEMBLING SILK HYDROGELS Scanning electron microscope of silk hydrogels showed a porous silk structure for 2% w/v silk hydrogels and
progressively less porosity for the high concentration samples (Fig. 2a). Secondary structure analysis by FTIR analysis showed an amide I absorption peak at 1625 cm−1 (i.e. β-sheet) for all
silk hydrogels (Fig. 2b). FTIR measurements were complemented by dynamic CD measurements of silk hydrogels. Ellipticity at 217 nm was used to track β-sheet conformation between 1 and 24
hours post sonication. At a lower silk content, the hydrogel showed a time-dependent increase in β-sheet content over 24 hours, whereas hydrogels with a higher silk content had essentially
completed β-sheet formation by 1 hour post sonication. SPACE CONFORMITY AND ABSENCE OF SWELLING FOR SELF-ASSEMBLING SILK HYDROGELS Space conforming properties without swelling are important
properties as the materials designed to fill a cavity should not compress the surrounding tissue in order to be minimally invasive. The _in vitro_ swelling studies showed that the weights of
the self-assembling silk hydrogels did not differ during the solution-gel transition or following overnight incubation in PBS (Fig. 3a). The conformity of the self-assembling silk hydrogels
was then assessed _in vitro_ before and after the completion of the solution-gel transition. Visual inspection showed that only silk samples that were still in the solution state achieved
complete space filling (Fig. 3b, left cuvette). A quantitative measurement of space conformity was devised by determining the amount of silk that was able to fill a pre-defined space. For 3%
w/v and 4% w/v silk samples, significantly more silk could be applied to a fixed volume when silk was in the solution state rather than in the gelled state; however, no statistical
difference was observed for 2% w/v silk samples (Fig. 3c). Preliminary _in vivo_ experiments, were designed to provide qualitative proof of concept insight to support these _in vitro_
results on space conformity. One excellent model system is experimental stroke which provides a cavity for space conformity to be visualised. After chronic cerebral ischemia, application of
the self-assembling silk hydrogels to the affected hemisphere resulted in excellent conformal fit (Supplementary Fig. S1). However, injection of self-assembling silk hydrogels in mice with
no apparent infarct cavity (i.e. the lesion had not fully developed) resulted in silk hydrogel accumulation in the ventricle with excellent space conformity (Supplementary Fig. S1). In rats
with small and medium lesions (i.e. cavities of variable sizes, detailed in Supplementary Fig. S3), injection of self-assembling silk hydrogels into the affected area showed excellent space
conformity, a seamless tissue-silk hydrogel interface, and no gross adverse tissue response 7 days after application (Fig. 4). The silk hydrogel appeared intact, with no obvious signs of
degradation. CYTOCOMPATIBILITY, INJECTABILITY AND DISTRIBUTION OF MSCS IN SELF-ASSEMBLING SILK HYDROGELS Exploiting self-assembling silk hydrogels for cell delivery requires that these
systems be cytocompatible, injectable and tuneable to control cell distribution within the three dimensional hydrogel structure. An initial drop in MSC viability was observed for all
hydrogels (Fig. 5a). For 2% w/v silk hydrogels, the cell viability was stabilised at day 2 and significant cell proliferation was observed from day 5 onwards, over the next 10 days, until
the end of the study period. Of all the hydrogels studied, the 2% w/v hydrogels supported the best MSC growth (Fig. 5a). For 3% w/v and 4% w/v hydrogels, the cell viability stabilised at day
3 and then steadily increased over the remaining culture period (up to 14 days) (Fig. 5a). The impact of injection shearing on cell viability was also assessed using silk still in the
solution state and in the gelled state (Fig. 5b). For 2% w/v silk, the use of only the smallest gauge needle (30G) resulted in a substantial drop in cell viability when the gelled samples,
rather than the liquid samples, were injected. This difference was less noticeable for 25G needles and was not observed for 21G needles. For 3% w/v silk samples, no difference was noted
between the samples when a 21G needle was used. However, a significant and size-dependent reduction in cell viability was noted between gelled and solution samples after injection though 25G
and 30G needles. The 4% w/v silk samples gave similar results, but a significant reduction in cell viability was even observed with a 21G needle (Fig. 5b). Following injection (i.e. needle
shearing forces), cell viability was better preserved for all solution silk samples than for the respective hydrogels. Using an injectable biomaterial for cell delivery requires control over
the (even) distribution of viable cells throughout the carrier matrix. Therefore, MSC distribution in the silk hydrogels was assessed by histology (Fig. 6a). MSCs were added to sonicated
silk within 10 and 60 minutes of the solution-gel transition: at 10 minutes, an even distribution of cells was observed at every level throughout the hydrogel, whereas at 60 minutes, most
cells had sunk to the bottom of the hydrogel due to gravity (Fig. 6b). Preliminary experiments in ischemic mice showed that addition of cells to silk undergoing the solution-gel transition
within the 10 minute time window resulted in uniform cell distribution _in vivo_ (Supplementary Fig. S2). DISCUSSION To date, no hydrogel system has been introduced into clinical practice
for the delivery of cells to the brain, despite the position of several biopolymers at the clinical forefront. For example, multivalent cation-induced self-assembly of alginate has been
exploited for encapsulation of genetically modified MSCs to express glucagon-like peptide-1 (i.e. GLP-1 CellBeads)34. These GLP-1 CellBeads have progressed to Phase I clinical trials
(ClinicalTrials.Gov identifier: NCT01298830) for treatment of ischemic stroke. However, the lack of long-term mechanical robustness and challenges in navigating regulatory hurdles remain
significant weaknesses of this delivery system. In addition, it ultimately requires surgical removal. Silk, by contrast, has a robust clinical track record in humans24 and our ability to
reverse engineer silk is introducing new silk formats for novel applications29. Cell delivery to the brain is emerging as a promising therapeutic strategy. However, current delivery
technologies (e.g. simple injection of cells without a matrix) fall short of our insight into (stem) cell niches thus potentially undermining their therapeutic potential by stripping them of
their supportive microenvironment (reviewed in9,10). We therefore explored the suitability of self-assembling silk hydrogels for future minimally invasive cell application; one potential
scenario is the administration to the brain and for supporting stem cells. For minimally invasive brain administration, the solution-gel characteristics and substrate elasticity are critical
so we therefore focussed on optimising the physical and chemical cues of self-assembling silk hydrogels for brain administration and stem cell support. Energy input into a silk solution
displaces solvating water molecules and exposes the hydrophobic silk domains, which subsequently rearrange and grow into nanocrystallites33. Secondary structure analysis by FTIR and CD (Fig.
2b and c, respectively) showed that these nanocrystallites were β-sheets and thus represented the points of physical crosslinking within the hydrogel. These nanocrystallites are responsible
for the observed light scattering and gave rise to the observed opaqueness of the silk hydrogels (this contrasts with chemically cross-linked silk hydrogels, which are transparent to
visible light)29. As expected, the overall solution-gel kinetics were concentration dependent, with higher silk concentrations forming mechanically stable hydrogels more rapidly. The lower
threshold for the formation of silk hydrogels was 1% w/v (Fig. 1d); in all probability, this concentration did not contain sufficient silk to form a mechanically robust hydrogel network,
despite the formation of nanocrystallites. Overall, the observed changes in secondary structure and the solution-gel transition were in good agreement with those reported in previous
studies33,35. Control over mechanical properties, such as stiffness, is also essential to recreate an orphan tissue microenvironment that can support (stem) cell function, tissue growth and
seamless integration with existing tissues7. Increasing silk content resulted in increased stiffness in the respective silk hydrogels due to the presence of nanocrystallites that provided
mechanical strength (Fig. 1c). At 2 to 4% w/v, the silk hydrogels exhibited matrix elasticity similar to that of brain tissue (0.1 to 1 kPa, indicated by dotted line and shading, Fig. 1c)36.
Qualitative assessment of these hydrogels by scanning electron microscopy showed a porous three-dimensional structure. For the clinical translation of (self-assembling) hydrogels for
intracerebral injection, good space-conforming properties without swelling are necessary to avoid compression against adjacent tissues, as this can further exacerbate cellular injury and
clinical symptoms9,10. The self-assembling silk hydrogels exhibited no swelling during the solution-gel transition and showed excellent space conformity _in vitro_ when injected in the
pre-gelled state, especially at a higher silk content (Fig. 3a,b and c). In support of our _in vitro_ results, preliminary _in vivo_ experiments allowed visualisation of good space
conformity in an ischemic cavity, in mice (Supplementary Fig. S1) and rats (Fig. 4) using 3% w/v and 4% w/v self-assembling silk hydrogels, respectively with no apparent adverse effects on
animal health or behaviour (Supplementary Fig. S1). This observation agreed with the work by Fernández-García and co-workers, who showed that the use of silk hydrogels in healthy mice caused
no considerable cognitive or sensorimotor deficits in either behavioural tests or electrophysiological analyses37 and, though outwith the scope of the present study, provide a platform for
future experiments that characterise cellular phenotype and survival as well as compatibility in the brain tissue after transplantation. The ability to fill irregularly shaped defects by
injecting a self-assembling material without the need for premoulding is essential for many therapeutic applications, including the stroke setting. One therapeutic strategy is the use of
MSCs (reviewed in1,2,38). Therefore, we examined the performance of MSCs following their embedding within self-assembling silk hydrogels _in vitro_. Over the course of the study period, the
MSCs proliferated, although they showed a transient decrease in cell viability for the first 3 days (Fig. 5a). Similar observations have been made previously with (silk) hydrogel systems
(e.g33,39,40.). For example, Wang and co-workers showed MSC proliferation over 21 days in 4% w/v silk hydrogels but negligible proliferation (and a degree of cell death) in 8% w/v and 12%
w/v hydrogels. This effect of high silk concentrations likely reflects nutrient mass transport limitations and possible mechanical restrictions imposed by the hydrogels33. We speculate that,
over time, MSCs are able to modify the silk hydrogel by endogenous ECM deposition. The differential response of MSCs to 2 and 4% w/v silk hydrogels reported here suggests a direct influence
of mechanobiology on MSC cell proliferation, which is not a unique effect of silk. For example, MSCs in collagen mimetic peptide hydrogels had better cell viability on softer hydrogels40;
similar observations have also been made with different stem/progenitor cells and hydrogel systems (e.g. neural stem/progenitor cells and methacrylamide chitosan)39. MSC cultures growing on
two-dimensional silk hydrogels showed a more spindle shaped morphology on soft silk hydrogels (6 kPa) and progressively spread out on stiffer substrates41. Treatment of MSCs with
transforming growth factor 1 enabled the transition to a vascular smooth muscle cell phenotype and the best results were achieved using silk hydrogels of medium stiffness (33 kPa)41.
Overall, (silk) mechanics is emerging as an important factor in MSC biological responses. Application of a therapeutic payload to the brain is an appealing therapeutic avenue, but it
requires minimally invasive administration of the payload. Delivery of MSCs requires a sustained cell viability and efficient cell distribution. We found that MSCs encapsulated in silk
hydrogel that gelled within 10 minutes showed excellent cell distribution throughout the hydrogel, when compared to longer solution-gel transition times where gravity resulted in MSC
settling (Fig. 6). Shear stress also affected MSC viability (Fig. 5b); as expected, cell viability was higher following injection from 21G needles than from narrower bore 25G and 30G
needles, and the best results were achieved with pre-gelled systems. In human clinical trials, delivery of stem cells into the cavity typically requires a custom-made needle with an internal
diameter of 0.35 mm (similar to 22G to 23G) (e.g.42). We therefore used gauge size 22G and 26G needles in our rat and mouse pre-clinical stroke models, respectively. These needle sizes
limit tissue damage but are also relevant for cell delivery. Preliminary studies in mouse stroke model showed uniform cell distribution (Supplementary Fig. S2). CONCLUSIONS Taken together,
this study provides valuable information regarding the optimal MSC-hydrogel matrix combinations for future experimental studies targeting central nervous system repair. The key findings of
the present study are that (i) self-assembling silk hydrogels exhibit controllable solution-gel kinetics, elasticity, and secondary structure, (ii) these self-assembling silk hydrogels can
be fine-tuned to achieve uniform cell distribution, viability and space conformity in the absence of any silk hydrogel swelling; and (iii) preliminary proof-of-concept studies allowed
visualisation of space conformity of self-assembling silk hydrogels after injection into the brain. Overall, our _in vitro_ data indicates that 3% w/v silk hydrogels, which gelled within 10
min of MSC addition, should be injected in the pre-gelled state to provide optimal support of MSC viability and distribution. MATERIALS AND METHODS SILK SOLUTION PREPARATION _Bombyx mori_
silk cocoons were reverse engineered as detailed previously28; for a video-based protocol, see43. Briefly, dried cocoons (Tajima Shoji Co., Yokohama, Japan) were degummed for 60 minutes in
25 mM Na2CO3 and then rinsed in ddH2O to remove sericin. Dried degummed silk fibres were dissolved in 9.3 M LiBr solution at 60 °C for 3 to 4 hours. The resulting solution was dialysed
against ddH2O using a dialysis cassette (molecular cut off of 3,500 Da; Thermo Fisher Scientific Inc., Waltham, MA, USA) for 2 days, with several changes of water, to remove LiBr salts. The
resulting aqueous silk solution (typically between 6 to 7% w/v) was centrifuged to remove any silk aggregates and the resulting silk solution was stored at 4 °C until use. MANUFACTURE,
MONITORING AND CHARACTERISATION OF SELF-ASSEMBLING SILK HYDROGELS Self-assembling silk hydrogels were prepared using a digitally controlled probe sonicator (Sonoplus HD 2070, Bandelin,
Berlin, Germany) fitted with a 23 cm long sonication tip (0.3 cm diameter tip and tapered over 8 cm). Unless otherwise stated, 4 to 8 ml sample batches in 15 ml Falcon tubes (1.4 cm diameter
and 11 cm long) (Greiner Bio-One GmbH, Kremsmünster, Austria) were exposed to a 30% amplitude for typically 3 to 6 sonication cycles on ice (one cycle consisted of 30 seconds on and 30
seconds off) to induce the solution-gel transition of 1 to 5% w/v silk samples (Fig. 1a). One method used to track the solution-gel transition was to measure light scattering at 405 nm
(Spectra Max M5, Molecular devices, Sunnyvale, CA, USA), because physically crosslinked silk hydrogels develop nanocrystalline regions that scatter light29. In the present study, this was
done by subjecting the silk solution samples to two 30 second sonication cycles, and light scattering was monitored for 24 hours. Circular dichroism (CD) spectroscopy was used to assess the
kinetic transition from a random coil to a stable β-sheet. Following sonication, samples were immediately loaded into a 0.01 mm path length measuring cell. The temperature was kept constant
at 25 °C, and the samples were scanned at one single time with a CD spectrometer (Chirascan-plus, Applied Photophysics Ltd, Leatherhead, UK) over the 190 to 250 nm spectrum with a 1 nm
resolution and 3 scans per time point over 24 hours. The change in ellipticity at 217 nm was used to monitor β-sheet formation. The silk secondary structure was assessed using Fourier
transform infrared (FTIR) spectroscopy, with measurements being repeated (total twice). For FTIR measurements, the silk hydrogel samples were exposed to 128 scans at 4 cm−1 resolutions over
the wavenumber range 400 to 4000 cm−1 using a TENSOR II FTIR spectrometer (Bruker Optik GmbH, Ettlingen, Germany). Baseline and peak fit were corrected by OriginPro 9.2 software at the amide
I region (1595–1705) as detailed previously44. The amide I region was identified and deconvoluted, as follows: 1605−1615 cm−1 as side chain/aggregated strands, 1616−1637 cm−1 and 1697−1703
cm−1 as β-sheet structure, 1638−1655 cm−1 as random coil structure, 1656−1662 cm−1 as α-helical bands and 1663−1696 cm−1 as β-turns. For rheological assessments, 2 to 5% w/v silk hydrogels
(0.2 ml) were prepared and equilibrated in PBS overnight. The hydrogels were then subjected to rheological characterization (Kinexus pro+ rheometer, Malvern Instruments Ltd., UK) using a 20
mm diameter plate set to 25 °C and appropriate gap size. Strain stress was measured first from 0.1 to 100% with at a set frequency of 1.0 Hz, followed by a frequency sweep. For scanning
electron microscopy (SEM), silk hydrogels were frozen and then freeze dried (Micro Modulyo, Thermo Fisher Scientific Inc.). Dried samples were immediately moved to a desiccator and sputter
coated with carbon using a vacuum coater (Polaron Division E6100, Bio-Rad, Birmingham, UK). Coated samples were imaged twice with a FE-SEM SU6600 scanning electron microscope (Hitachi High
Technologies, Krefeld, Germany) using 5 kV acceleration voltage. Electron micrographs were analysed using ImageJ v1.50i (National Institutes of Health, Bethesda, MD, USA). ASSESSMENT OF SILK
HYDROGEL SWELLING AND SPACE CONFORMITY To determine silk hydrogel swelling, 300 µl of sonicated silk solution was added to pre-weighed Eppendorf tubes and weighed. Once the hydrogel had
gelled, phosphate buffered saline (PBS; 300 µl) was added carefully on top of the silk hydrogel, the tubes were re-weighed and left for 24 hours. After complete removal of PBS, the final
weight was determined. The swelling ratio was calculated using the initial silk solution weight and the final weight after 24 hours of PBS incubation. The silk hydrogels were generated
(detailed above) and subjected to _in vitro_ space conformity testing. Sonicated silk samples were drawn up into 1 ml syringes (without a needle), and either (i) the silk sample was left in
the syringe to complete the solution-gel transition and subsequently transferred to a cuvette, or (ii) the silk sample was immediately transferred from the syringe to the cuvette (i.e. still
in its liquid form) and allowed to gel in the cuvette. In both conditions, the cuvettes were filled with the silk hydrogel samples up to the 1 ml mark. The cuvettes were then weighed and
the conformity was calculated using the theoretical weight of the respective 1 ml sample as 100%. PREPARATION AND ASSESSMENT OF MESENCHYMAL STEM CELLS IN SELF-ASSEMBLING SILK HYDROGELS Mouse
C3H10T0.5 mesenchymal stem cells (American Type Culture Collection) were grown on tissue culture treated polystyrene flasks (Corning Inc., New York, USA) and cultured in Roswell Park
Memorial Institute medium 1640 containing 4.5G GlutaMAX, supplemented with 10% v/v foetal bovine serum and penicillin and streptomycin (50 U/mL penicillin and 50 μg/mL streptomycin) (Thermo
Fisher Scientific). Cells were maintained in a humidified atmosphere of 5% CO2 at 37 °C, and subconfluent cultures were routinely subcultured with trypsin/EDTA every 2 to 3 days. For silk
hydrogel cell culture studies, the silk solution was filter sterilised (33 mm Millex-GP syringe filter fitted with a polyethersulfone membrane with 0.22 µm pores) and the silk solution was
sonicated on ice in a class II biological safety cabinet. Next, 10× PBS was added to the aqueous silk solutions to yield an isotonic solution and C3H10T0.5 cells (2 × 105 cells per 50 μl of
silk were added to the processed silk samples at 28 °C to 32 °C). The exact timing of cell addition was established by monitoring the flow characteristics of the silk sample. Uniform cell
seeding throughout the silk hydrogel was achieved by adding cells once the initiation of the solution-gel transition was evident. The MSC silk mixture (2 × 105 cells in 50 μl) was pipetted
into a 96-well plate well (well surface area 0.32 cm2) and transferred to the cell incubator for 10 to 30 minutes to allow completion of the solution-gel transition. Next, 200 µl of complete
culture medium was carefully added on the top of the mixture, and this was changed every 3 days. Cell viability was assessed by adding 25 μl AlamarBlue (Thermo Fisher Scientific) to the
respective well and the cells were allowed to metabolise the substrate for 4 hours. The culture supernatant was then transferred to a black 96-well plate (Sigma-Aldrich, St. Louis, MO, USA)
and measured with a fluorescence plate reader (POLARstar Omega BMG LABTECH GmbH, Ortenburg, Germany) by fixing the photo multiplier tube and setting the excitation and emission filters to
560 nm and 590 nm, respectively. The viability of the MSCs in silk hydrogels post-injection was assessed by injecting 50 µl of silk MSC sample mixtures in either the pre-gelled (i.e. in the
liquid form) or post-gelled state through different needle gauges (21, 25 and 30G) into 96-well plates to establish the effect of shear stress on cell viability. The cell viability was
assessed within 180 minutes after injection using AlamarBlue, as detailed above. This short time frame was selected to assess shear stress induced changes in viability while minimizing
differences due to proliferation. In a final set of _in vitro_ studies, the distribution of encapsulated MSCs in silk hydrogels was assessed by histology. The solution-gel transition was
fine tuned to occur within 10 or 60 minutes. During this solution-gel transition time window, cells were added to the silk samples and the MSC silk mixture was transferred into 24-well plate
Transwell inserts with the smallest pore size of 0.4 µm to mitigate sample leakage (Corning Life Sciences B.V., Amsterdam, The Netherlands). These Transwell inserts have a surface area of
0.32 cm2 and therefore resemble the 96-well plate format used in our study. To facilitate sample handling, the MSC silk mixture was scaled up to 200 µl. Once the silk samples had completed
their solution-gel transition, the Transwell membrane was cut to facilitate removal of the intact silk hydrogels. The hydrogels were fixed in 4% paraformaldehyde for 30 minutes, then
immersed in sucrose (30% w/v) overnight at 4 °C, frozen in isopentane/dry ice at −42 °C for 2 minutes and cryosectioned. The 20 µm sections were stained using haematoxylin and eosin. A
minimum of 3 consecutive sections per sample were analysed. Each image was segmented into 4 equal levels, based on their depth in the hydrogel in the Transwell, with level 4 being at the
bottom of the hydrogel in the Transwell and level 1 being at the top of the hydrogel in the Transwell (see Supplementary Fig. S4). Levels 1–4 are shown on the Fig. 6a on the left hand sides
of the images. The number of cells in each level was counted. The purpose of the 4 levels was to quantify whether the cells had sunk to the bottom of the hydrogel in the Transwell or whether
the cells had equal distribution throughout the hydrogel. RAT STROKE MODEL AND ADMINISTRATION OF SELF-ASSEMBLING SILK HYDROGELS Preliminary experiments were designed to allow visualisation
of space conformity _in vivo_. All _in vivo_ studies were approved by the Home Office of the United Kingdom (Project License Number 60/4469). All procedures complied with the UK Animals
(Scientific) Procedures Act (1986) and the Ethical Review Process of the Institute of Pharmacy and Biomedical Sciences at the University of Strathclyde. The _in vivo_ studies followed the
ARRIVE guidelines45. Animals were kept under a 12 hour light/dark cycle and were fed _ad libitum_. The _in vivo_ studies were conducted in rodent models. The rat data are shown in the
manuscript. The mice data are shown in Supplementary information only. The rat study was performed as detailed previously46. Briefly, male Sprague-Dawley rats (n = 4, weight 240–290G, 8–9
weeks, Harlan, UK) underwent a right transient middle cerebral artery occlusion for 60 minutes by insertion of a propylene filament (Doccol Corporation; tip diameter with coating 0.33 +/−
0.02 mm), via the common carotid artery to the ostium of the middle cerebral artery in the circle of Willis. A priori exclusion criterion was any animal found to be moribund due to excessive
weight loss (>20% of start weight). No animals were excluded based on this exclusion criteria, however one animal was excluded due to damage to tissue during processing of the tissue for
histology, leading to a final n number n = 3. At 14 days after this middle cerebral artery occlusion, 10 μl of 4% w/v self-assembling silk hydrogel was injected at a rate of 2 μl/minute at
coordinates (L) −1.5 mm, (A-P) −3.5 mm and (V) −6.5 mm, using a Hamilton syringe with a 22 gauge blunt tip needle. Animals were terminally anaesthetised at 1 week after the transplantation
by overdosing with sodium pentobarbital. A transcardial perfusion of 0.9% w/v saline was followed by 4% w/v ice-cold paraformaldehyde in 0.2 M PBS. Brains were removed following craniotomy
and were fixed in paraformaldehyde for 24 hours. The brains were then immersed in cryoprotective solution (30% w/v sucrose in PBS with 0.01% w/v sodium azide for 72 hours, followed by rapid
freezing on dry ice). Coronal (40 μm) cryostat sections were cut and stained with haematoxylin and eosin. STATISTICAL ANALYSES Data were analysed using GraphPad Prism 7.0 (GraphPad Software,
La Jolla, CA, U.S.A.). Sample pairs were analysed with the Student’s t-test. Multiple samples were evaluated by one-way analysis of variance (ANOVA), followed by Dunnett’s multiple
comparison post hoc test. Asterisks were used to denote statistical significance as follows: *P < 0.05, **P < 0.01, ***P < 0.001. All data were presented as mean values ± standard
deviation (SD). The number of independent experiments (n) is noted in each figure legend. DATA AVAILABILITY SECTION All data created during this research are openly available from the
University of Strathclyde-Pure, at https://doi.org/10.15129/2bbce19a-4b47-43d9-b9d5-7549b4d9ae4a. REFERENCES * Sinden, J. D. & Muir, K. W. Stem cells in stroke treatment: the promise and
the challenges. _Int. J. Stroke_ 7, 426–434 (2012). Article PubMed Google Scholar * Nagpal, A. _et al_. Safety and effectiveness of stem cell therapies in early-phase clinical trials in
stroke: a systematic review and meta-analysis. _Stem Cell Res. Ther._ 8, 191 (2017). Article PubMed PubMed Central Google Scholar * Wang, J. _et al_. Ischemic stroke and repair: current
trends in research and tissue engineering treatments. _Regen. Med. Res._ 2, 3 (2014). Article PubMed PubMed Central Google Scholar * Lindvall, O. & Kokaia, Z. Stem cells in human
neurodegenerative disorders–time for clinical translation? _J. Clin. Invest._ 120, 29–40 (2010). Article PubMed PubMed Central CAS Google Scholar * Vining, K. H. & Mooney, D. J.
Mechanical forces direct stem cell behaviour in development and regeneration. _Nat. Rev. Mol. Cell Biol._ 18, 728–742 (2017). Article PubMed PubMed Central CAS Google Scholar * Dalby,
M. J., Gadegaard, N. & Oreffo, R. O. Harnessing nanotopography and integrin-matrix interactions to influence stem cell fate. _Nat. Mater._ 13, 558–569 (2014). Article ADS PubMed CAS
Google Scholar * Darnell, M. & Mooney, D. J. Leveraging advances in biology to design biomaterials. _Nat. Mater._ 16, 1178–1185 (2017). Article ADS PubMed CAS Google Scholar *
Prewitz, M., Seib, F. P., Pompe, T. & Werner, C. Polymeric biomaterials for stem cell bioengineering. _Macromol. Rapid Commun._ 33, 1420–1431 (2012). Article PubMed CAS Google Scholar
* Nih, L. R., Carmichael, S. T. & Segura, T. Hydrogels for brain repair after stroke: an emerging treatment option. _Curr. Opin. Biotechnol_ 40, 155–163 (2016). Article PubMed PubMed
Central CAS Google Scholar * Tam, R. Y., Fuehrmann, T., Mitrousis, N. & Shoichet, M. S. Regenerative therapies for central nervous system diseases: a biomaterials approach.
_Neuropsychopharmacology_ 39, 169–188 (2014). Article PubMed CAS Google Scholar * Gasperini, L., Mano, J. F. & Reis, R. L. Natural polymers for the microencapsulation of cells. _J.
R. Soc. Interface_ 11, 20140817 (2014). Article PubMed PubMed Central CAS Google Scholar * Nguyen, M. K. & Alsberg, E. Bioactive factor delivery strategies from engineered polymer
hydrogels for therapeutic medicine. _Prog. Polym. Sci._ 39, 1236–1265 (2014). Article PubMed PubMed Central CAS Google Scholar * Freudenberg, U. _et al_. A star-PEG-heparin hydrogel
platform to aid cell replacement therapies for neurodegenerative diseases. _Biomaterials_ 30, 5049–5060 (2009). Article PubMed CAS Google Scholar * Li, S. _et al_. Hydrogels with
precisely controlled integrin activation dictate vascular patterning and permeability. _Nat. Mater._ 16, 953–961 (2017). Article ADS PubMed PubMed Central CAS Google Scholar * Emerich,
D. F. _et al_. Injectable VEGF hydrogels produce near complete neurological and anatomical protection following cerebral ischemia in rats. _Cell Transplant._ 19, 1063–1071 (2010). Article
PubMed Google Scholar * Cheng, T. Y., Chen, M. H., Chang, W. H., Huang, M. Y. & Wang, T. W. Neural stem cells encapsulated in a functionalized self-assembling peptide hydrogel for
brain tissue engineering. _Biomaterials_ 34, 2005–2016 (2013). Article PubMed CAS Google Scholar * Tseng, T. C. _et al_. An Injectable, Self-Healing Hydrogel to Repair the Central
Nervous System. _Adv. Mater._ 27, 3518–3524 (2015). Article PubMed CAS Google Scholar * Thonhoff, J. R., Lou, D. I., Jordan, P. M., Zhao, X. & Wu, P. Compatibility of human fetal
neural stem cells with hydrogel biomaterials _in vitro_. _Brain Res._ 1187, 42–51 (2008). Article PubMed CAS Google Scholar * Ghuman, H. _et al_. Long-term retention of ECM hydrogel
after implantation into a sub-acute stroke cavity reduces lesion volume. _Acta Biomater._ 63, 50–63 (2017). Article PubMed CAS Google Scholar * Massensini, A. R. _et al_.
Concentration-dependent rheological properties of ECM hydrogel for intracerebral delivery to a stroke cavity. _Acta Biomater._ 27, 116–130 (2015). Article PubMed PubMed Central CAS
Google Scholar * Prewitz, M. C. _et al_. Tightly anchored tissue-mimetic matrices as instructive stem cell microenvironments. _Nat. Methods_ 10, 788–794 (2013). Article PubMed CAS Google
Scholar * Gorgieva, S. & Kokol, V. In _Biomaterials Applications for Nanomedicine_ (ed. Rosario Pignatello) Ch. Collagen- vs. Gelatine-Based Biomaterials and Their Biocompatibility:
Review and Perspectives, 17–52 (InTech, 2011). * Seliktar, D. Designing cell-compatible hydrogels for biomedical applications. _Science_ 336, 1124–1128 (2012). Article ADS PubMed CAS
Google Scholar * Holland, C., Numata, K., Rnjak-Kovacina, J. & Seib, F. P. The Biomedical Use of Silk: Past, Present, Future. _Adv. Healthc. Mater._
https://doi.org/10.1002/adhm.201800465 (2018). * Jewell, M., Daunch, W., Bengtson, B. & Mortarino, E. The development of SERI® Surgical Scaffold, an engineered biological scaffold. _Ann.
N.Y. Acad. Sci._ 1358, 44–55 (2015). Article ADS PubMed CAS Google Scholar * Vollrath, F. & Porter, D. Silks as ancient models for modern polymers. _Polymer_ 50, 5623–5632 (2009).
Article CAS Google Scholar * Thurber, A. E., Omenetto, F. G. & Kaplan, D. L. _In vivo_ bioresponses to silk proteins. _Biomaterials_ 71, 145–157 (2015). Article PubMed PubMed
Central CAS Google Scholar * Rockwood, D. N. _et al_. Materials fabrication from Bombyx mori silk fibroin. _Nat. Protoc._ 6, 1612–1631 (2011). Article PubMed CAS Google Scholar *
Seib, F. P. In _Hydrogel_s: D_es_ign, _Synthesis and Application in Drug Delivery & Regenerative Medicine_ (eds T. Singh, R. R., Laverty, G. & Donnelly, R.) Ch. 2, 208–227 (CRC Press
2018). * Sun, W. _et al_. Genipin-crosslinked gelatin-silk fibroin hydrogels for modulating the behaviour of pluripotent cells. _J. Tissue Eng. Regen. Med._ 10, 876–887 (2016). Article
PubMed CAS Google Scholar * Bai, S. _et al_. Silk Nanofiber Hydrogels with Tunable Modulus to Regulate Nerve Stem Cell Fate. _J. Mater. Chem. B_ 2, 6590–6600 (2014). Article PubMed
PubMed Central CAS Google Scholar * Sun, W. _et al_. Viability and neuronal differentiation of neural stem cells encapsulated in silk fibroin hydrogel functionalized with an IKVAV
peptide. _J. Tissue Eng. Regen. Med._ 11, 1532–1541 (2017). Article PubMed CAS Google Scholar * Wang, X., Kluge, J. A., Leisk, G. G. & Kaplan, D. L. Sonication-induced gelation of
silk fibroin for cell encapsulation. _Biomaterials_ 29, 1054–1064 (2008). Article PubMed CAS Google Scholar * Wallrapp, C. _et al_. Cell-based delivery of glucagon-like peptide-1 using
encapsulated mesenchymal stem cells. _J. Microencapsul._ 30, 315–324 (2013). Article PubMed CAS Google Scholar * Seib, F. P., Pritchard, E. M. & Kaplan, D. L. Self-assembling
doxorubicin silk hydrogels for the focal treatment of primary breast cancer. _Adv. Funct. Mater._ 23, 58–65 (2013). Article PubMed CAS Google Scholar * Goriely, A. _et al_. Mechanics of
the brain: perspectives, challenges, and opportunities. _Biomech. Model. Mechanobiol._ 14, 931–965 (2015). Article PubMed PubMed Central Google Scholar * Fernandez-Garcia, L. _et al_.
Safety and tolerability of silk fibroin hydrogels implanted into the mouse brain. _Acta Biomater._ 45, 262–275 (2016). Article PubMed CAS Google Scholar * Kenmuir, C. L. & Wechsler,
L. R. Update on cell therapy for stroke. _Stroke Vasc. Neurol._ 2, 59–64 (2017). Article PubMed PubMed Central Google Scholar * Leipzig, N. D. & Shoichet, M. S. The effect of
substrate stiffness on adult neural stem cell behavior. _Biomaterials_ 30, 6867–6878 (2009). Article PubMed CAS Google Scholar * Liu, S. Q. _et al_. Biomimetic hydrogels for chondrogenic
differentiation of human mesenchymal stem cells to neocartilage. _Biomaterials_ 31, 7298–7307 (2010). Article PubMed CAS Google Scholar * Floren, M. _et al_. Human mesenchymal stem
cells cultured on silk hydrogels with variable stiffness and growth factor differentiate into mature smooth muscle cell phenotype. _Acta Biomater._ 31, 156–166 (2016). Article PubMed CAS
Google Scholar * Kalladka, D. _et al_. Human neural stem cells in patients with chronic ischaemic stroke (PISCES): a phase 1, first-in-man study. _Lancet_ 388, 787–796 (2016). Article
PubMed Google Scholar * Wongpinyochit, T., Johnston, B. F. & Seib, F. P. Manufacture and Drug Delivery Applications of Silk Nanoparticles. _J. Vis. Exp_. e54669, (2016). *
Wongpinyochit, T., Uhlmann, P., Urquhart, A. J. & Seib, F. P. PEGylated Silk Nanoparticles for Anticancer Drug Delivery. _Biomacromolecules_ 16, 3712–3722 (2015). Article PubMed CAS
Google Scholar * Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research.
_PLoS Biol._ 8, e1000412 (2010). Article PubMed PubMed Central CAS Google Scholar * Kazanis, I. _et al_. The late response of rat subependymal zone stem and progenitor cells to stroke
is restricted to directly affected areas of their niche. _Exp. Neurol._ 248, 387–397 (2013). Article PubMed PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS The authors
would like to thank Tracy Sutherland (University of Strathclyde) for technical assistance. This work was supported by a Taif University PhD fellowship (Saudi Arabia) (I.O.), EPSRC First
Grant (EP/N03127X/1) (F.P.S.), a FP7-PEOPLE-2012-CIG Marie-Curie Action Career Integration Grant 334134 within the 7th European Union Framework Program (F.P.S.) and a Daphne Jackson
Fellowship (N.G.) which was sponsored by Medical Research Scotland. AUTHOR INFORMATION Author notes * Seib, F. P. and Carswell, H. V. O. contributed equally. AUTHORS AND AFFILIATIONS *
Strathclyde Institute of Pharmacy and Biomedical Sciences, University of Strathclyde, Glasgow, UK I. Osama, N. Gorenkova, C. M. McKittrick, T. Wongpinyochit, A. Goudie, F. P. Seib & H.
V. O. Carswell * Leibniz Institute of Polymer Research Dresden, Max Bergmann Center of Biomaterials Dresden, Hohe Strasse 6, 01069, Dresden, Germany F. P. Seib Authors * I. Osama View author
publications You can also search for this author inPubMed Google Scholar * N. Gorenkova View author publications You can also search for this author inPubMed Google Scholar * C. M.
McKittrick View author publications You can also search for this author inPubMed Google Scholar * T. Wongpinyochit View author publications You can also search for this author inPubMed
Google Scholar * A. Goudie View author publications You can also search for this author inPubMed Google Scholar * F. P. Seib View author publications You can also search for this author
inPubMed Google Scholar * H. V. O. Carswell View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS I.O. performed the experiments, analysed and
interpreted the data and wrote the manuscript draft. N.G. performed _in vivo_ studies in rats and provided stroke model expertise. C.M. provided expertise with the mouse stroke model. T.W.
provided expertise in the CD and FTIR experiments. A.G. provided technical assistance. H.C. and F.P.S. conceived and designed the research study, interpreted the data and edited the content
of the manuscript. CORRESPONDING AUTHORS Correspondence to F. P. Seib or H. V. O. Carswell. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL
INFORMATION PUBLISHER'S NOTE: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. ELECTRONIC SUPPLEMENTARY MATERIAL
SUPPLEMENTARY INFORMATION RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation,
distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and
indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to
the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will
need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE
CITE THIS ARTICLE Osama, I., Gorenkova, N., McKittrick, C.M. _et al._ _In vitro_ studies on space-conforming self-assembling silk hydrogels as a mesenchymal stem cell-support matrix suitable
for minimally invasive brain application. _Sci Rep_ 8, 13655 (2018). https://doi.org/10.1038/s41598-018-31905-5 Download citation * Received: 28 February 2018 * Accepted: 23 August 2018 *
Published: 12 September 2018 * DOI: https://doi.org/10.1038/s41598-018-31905-5 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable
link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * Silk Hydrogels *
Mesenchymal Stem Cells (MSC) * Uniform Cell Distribution * Silk Samples * Silk Solution








