- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
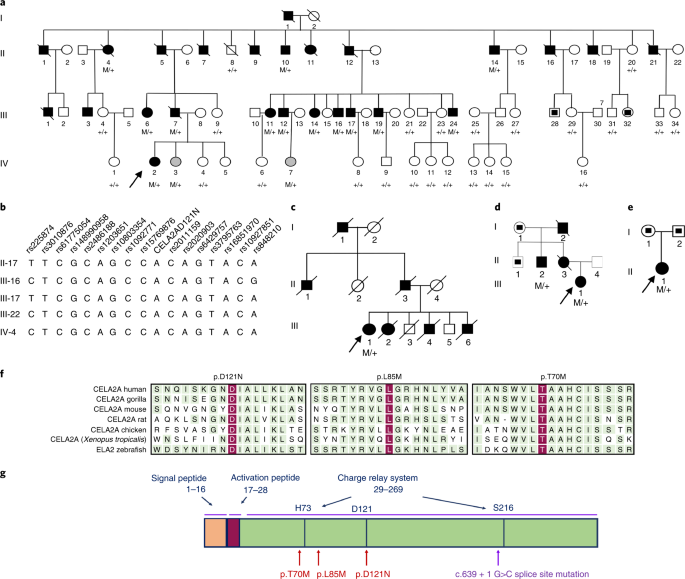
ABSTRACT Factors that underlie the clustering of metabolic syndrome traits are not fully known. We performed whole-exome sequence analysis in kindreds with extreme phenotypes of early-onset
atherosclerosis and metabolic syndrome, and identified novel loss-of-function mutations in the gene encoding the pancreatic elastase chymotrypsin-like elastase family member 2A (CELA2A). We
further show that CELA2A is a circulating enzyme that reduces platelet hyperactivation, triggers both insulin secretion and degradation, and increases insulin sensitivity. CELA2A plasma
levels rise postprandially and parallel insulin levels in humans. Loss of these functions by the mutant proteins provides insight into disease mechanisms and suggests that CELA2A could be an
attractive therapeutic target. Access through your institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your
institution Access Nature and 54 other Nature Portfolio journals Get Nature+, our best-value online-access subscription $32.99 / 30 days cancel any time Learn more Subscribe to this journal
Receive 12 print issues and online access $209.00 per year only $17.42 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices
may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support
SIMILAR CONTENT BEING VIEWED BY OTHERS ASSOCIATION OF PROTEIN FUNCTION-ALTERING VARIANTS WITH CARDIOMETABOLIC TRAITS: THE STRONG HEART STUDY Article Open access 04 June 2022 INFRAME
INSERTION AND SPLICE SITE VARIANTS IN _MFGE8_ ASSOCIATE WITH PROTECTION AGAINST CORONARY ATHEROSCLEROSIS Article Open access 17 August 2022 IDENTIFICATION OF A NOVEL _LDLR_ P.GLU179MET
VARIANT IN THAI FAMILIES WITH FAMILIAL HYPERCHOLESTEROLEMIA AND RESPONSE TO TREATMENT WITH PCSK9 INHIBITOR Article Open access 21 March 2024 DATA AVAILABILITY Human variants and phenotypes
have been reported to ClinVar under accession numbers SCV000916382, SCV000916383, SCV000916384 and SCV000916385. The data have also been reported to NIH with other identified variants in the
Yale Center for Mendelian Genomics. Proteomics data are available on request. REFERENCES * Murray, C. L. & Lopez, A. D. Global mortality, disability, and the contribution of risk
factors: global burden of disease study. _Lancet_ 349, 1436–1442 (1997). Article CAS Google Scholar * Malik, S. et al. Impact of the metabolic syndrome on mortality from coronary heart
disease, cardiovascular disease, and all causes in United States adults. _Circulation_ 110, 1245–1250 (2004). Article Google Scholar * Marenberg, M., Risch, N., Berkman, L. F., Floderus,
B. & Defaire, U. Genetic susceptibility to death from coronary heart-disease in a study of twins. _N. Engl. J. Med._ 330, 1041–1046 (1994). Article CAS Google Scholar * Abifadel, M.
et al. Mutations in _PCSK9_ cause autosomal dominant hypercholesterolemia. _Nat. Genet._ 34, 154–156 (2003). Article CAS Google Scholar * Mani, A. et al. _LRP6_ mutation in a family with
early coronary disease and metabolic risk factors. _Science_ 315, 1278–1282 (2007). Article CAS Google Scholar * Keramati, A. R. et al. A form of the metabolic syndrome associated with
mutations in _DYRK1B_. _N. Engl. J. Med._ 370, 1909–1919 (2014). Article Google Scholar * Szepessy, E. & Sahin-Toth, M. Inactivity of recombinant ELA2B provides a new example of
evolutionary elastase silencing in humans. _Pancreatology_ 6, 117–122 (2006). Article CAS Google Scholar * Largman, C., Brodrick, J. W. & Geokas, M. C. Purification and
characterization of two human pancreatic elastases. _Biochemistry_ 15, 2491–2500 (1976). Article CAS Google Scholar * Adzhubei, I. A. et al. A method and server for predicting damaging
missense mutations. _Nat. Methods_ 7, 248–249 (2010). Article CAS Google Scholar * Warren, H. R. et al. Genome-wide association analysis identifies novel blood pressure loci and offers
biological insights into cardiovascular risk. _Nat. Genet._ 49, 403–415 (2017). Article CAS Google Scholar * Wain, L. V. et al. Novel blood pressure locus and gene discovery using
genome-wide association study and expression data sets from blood and the kidney. _Hypertension_ https://doi.org/10.1161/HYPERTENSIONAHA.117.09438 (2017). * Hoffmann, T. J. et al.
Genome-wide association analyses using electronic health records identify new loci influencing blood pressure variation. _Nat. Genet._ 49, 54–64 (2017). Article CAS Google Scholar *
Fersht, A. & Sperling, J. The charge relay system in chymotrypsin and chymotrypsinogen. _J. Mol. Biol._ 74, 137–149 (1973). Article CAS Google Scholar * Frey, P. A., Whitt, S. A.
& Tobin, J. B. A low-barrier hydrogen bond in the catalytic triad of serine proteases. _Science_ 264, 1927–1930 (1994). Article CAS Google Scholar * Oleksyszyn, J. & Powers, J. C.
Irreversible inhibition of serine proteases by peptide derivatives of (alpha-aminoalkyl)phosphonate diphenyl esters. _Biochemistry_ 30, 485–493 (1991). Article CAS Google Scholar * Yang,
X., Pratley, R. E., Tokraks, S., Bogardus, C. & Permana, P. A. Microarray profiling of skeletal muscle tissues from equally obese, non-diabetic insulin-sensitive and insulin-resistant
Pima Indians. _Diabetologia_ 45, 1584–1593 (2002). Article CAS Google Scholar * Marselli, L. et al. Gene expression profiles of beta-cell enriched tissue obtained by laser capture
microdissection from subjects with type 2 diabetes. _PLoS ONE_ 5, e11499 (2010). Article Google Scholar * Hulme, J. T. et al. Sites of proteolytic processing and noncovalent association of
the distal C-terminal domain of CaV1.1 channels in skeletal muscle. _Proc. Natl Acad. Sci. USA_ 102, 5274–5279 (2005). Article CAS Google Scholar * Gao, T. et al. C-terminal fragments of
the α1C (CaV1.2) subunit associate with and regulate l-type calcium channels containing C-terminal-truncated α1C subunits. _J. Biol. Chem._ 276, 21089–21097 (2001). Article CAS Google
Scholar * Steneberg, P. et al. The type 2 diabetes-associated gene _ide_ is required for insulin secretion and suppression of α-synuclein levels in β-cells. _Diabetes_ 62, 2004–2014 (2013).
Article CAS Google Scholar * Farris, W. et al. Insulin-degrading enzyme regulates the levels of insulin, amyloid β-protein, and the β-amyloid precursor protein intracellular domain in
vivo. _Proc. Natl Acad. Sci. USA_ 100, 4162–4167 (2003). Article CAS Google Scholar * Schilling, R. J. & Mitra, A. K. Degradation of insulin by trypsin and α-chymotrypsin. _Pharm.
Res_ 8, 721–727 (1991). Article CAS Google Scholar * Poy, M. N. et al. CEACAM1 regulates insulin clearance in liver. _Nat. Genet._ 30, 270–276 (2002). Article Google Scholar * Shattil,
S. J., Hoxie, J. A., Cunningham, M. & Brass, L. F. Changes in the platelet membrane glycoprotein IIb·IIIa complex during platelet activation. _J. Biol. Chem._ 260, 11107–11114 (1985).
CAS PubMed Google Scholar * Yeh, J. J. et al. P-selectin-dependent platelet aggregation and apoptosis may explain the decrease in platelet count during _Helicobacter pylori_ infection.
_Blood_ 115, 4247–4253 (2010). Article CAS Google Scholar * Kato, S. et al. Increased calcium-channel currents of pancreatic β cells in neonatally streptozocin-induced diabetic rats.
_Metabolism_ 43, 1395–1400 (1994). Article CAS Google Scholar * Calanna, S. et al. Secretion of glucagon-like peptide-1 in patients with type 2 diabetes mellitus: systematic review and
meta-analyses of clinical studies. _Diabetologia_ 56, 965–972 (2013). Article CAS Google Scholar * Herzberg-Schafer, S., Heni, M., Stefan, N., Haring, H. U. & Fritsche, A. Impairment
of GLP1-induced insulin secretion: role of genetic background, insulin resistance and hyperglycaemia. _Diabetes Obes. Metab._ 14, 85–90 (2012). Article Google Scholar * Pidard, D.,
Frelinger, A. L., Bouillot, C. & Nurden, A. T. Activation of the fibrinogen receptor on human platelets exposed to alpha chymotrypsin. relationship with a major proteolytic cleavage at
the carboxyterminus of the membrane glycoprotein IIb heavy chain. _Eur. J. Biochem._ 200, 437–447 (1991). Article CAS Google Scholar * Robert, L., Jacob, M. P. & Labat-Robert, J.
Cell–matrix interactions in the genesis of arteriosclerosis and atheroma: effect of aging. _Ann. NY Acad. Sci._ 673, 331–341 (1992). Article CAS Google Scholar * Katsunuma, H., Shimizu,
K., Iwamoto, T. & Kiyokawa, M. Anti-atherosclerotic action of elastase—with special reference to its effect on elastic fibres. _Age Ageing_ 12, 183–194 (1983). Article CAS Google
Scholar * Zureik, M. et al. Serum elastase activity, serum elastase inhibitors, and occurrence of carotid atherosclerotic plaques: the Etude sur le Vieillissement Arteriel (EVA) study.
_Circulation_ 205, 2638–2645 (2002). Article Google Scholar * Tzoulaki, I. et al. Relative value of inflammatory, hemostatic, and rheological factors for incident myocardial infarction and
stroke: the Edinburgh Artery Study. _Circulation_ 115, 2119–2127 (2007). Article Google Scholar * Talukdar, S. et al. Neutrophils mediate insulin resistance in mice fed a high-fat diet
through secreted elastase. _Nat. Med._ 18, 1407–1412 (2012). Article CAS Google Scholar * Lee, J., Hong, Y. P., Shin, H. J. & Lee, W. Associations of sarcopenia and sarcopenic obesity
with metabolic syndrome considering both muscle mass and muscle strength. _J. Prev. Med. Public Health_ 49, 35–44 (2016). Article Google Scholar * NHLBI GO Exome Sequencing Project (ESP),
_Exome Variant Server_ http://evs.gs.washington.edu/EVS/ (accessed June 2013). * Szabo, A., Pilsak, C., Bence, M., Witt, H. & Sahin-Toth, M. Complex formation of human proelastases with
procarboxypeptidases A1 and A2. _J. Biol. Chem._ 291, 17706–17716 (2016). Article CAS Google Scholar * Go, G. W. et al. The combined hyperlipidemia caused by impaired Wnt-LRP6 signaling
is reversed by Wnt3a rescue. _Cell Metab._ 19, 209–220 (2014). Article CAS Google Scholar * Miller, M. B. et al. Brain region and isoform-specific phosphorylation alters kalirin SH2
domain interaction sites and calpain sensitivity. _ACS Chem. Neurosci._ 8, 1554–1569 (2017). Article CAS Google Scholar * Baucum, A. J., Shonesy, B. C., Rose, K. L. & Colbran, R. J.
Quantitative proteomics analysis of CaMKII phosphorylation and the CaMKII interactome in the mouse forebrain. _ACS Chem. Neurosci._ 6, 615–631 (2015). Article CAS Google Scholar * Lee, S.
H. et al. Inducing mitophagy in diabetic platelets protects against severe oxidative stress. _EMBO Mol. Med._ 8, 779–795 (2016). Article CAS Google Scholar Download references
ACKNOWLEDGEMENTS We thank T. Lam, J. Kanyo, W. Wang and N. Rauniar from the Yale Keck Mass Spectrometry and Proteomics Services for help with the proteomics analysis, and J. Murphy from the
Department of Pharmacology at Yale University School of Medicine for preparing the ribbon diagrams. This work was supported by grants from the National Institutes of Health (NIH) (RHL135767A
and P30 DK34989 to A.M., NIH R01DK095753 to M.S.-T. and NIH T32DK to F.E. (DK007356)), a grant from the NIH Centers for Mendelian Genomics (5U54HG006504) and a VA Merit Award to F.S.G. (NIH
S10 (SIG) OD018034 awarded to the Mass Spectrometry and Proteomics Resource of the W.M. Keck Foundation Biotechnology Resource Laboratory at Yale University). The authors would like to
thank the NHLBI GO Exome Sequencing Project and its ongoing studies, which produced and provided exome variant calls for comparison: the Lung GO Sequencing Project (HL-102923), the WHI
Sequencing Project (HL-102924), the Broad GO Sequencing Project (HL-102925), the Seattle GO Sequencing Project (HL-102926) and the Heart GO Sequencing Project (HL-103010). AUTHOR INFORMATION
AUTHORS AND AFFILIATIONS * Department of Internal Medicine, Yale School of Medicine, New Haven, CT, USA Fatemehsadat Esteghamat, James S. Broughton, Emily Smith, Rebecca Cardone, Tarun
Tyagi, Mateus Guerra, Nelson Ugwu, Mitra V. Mani, Bani Azari, Gerald Kayingo, Sunny Chung, Mohsen Fathzadeh, Jeffrey Bender, Michael H. Nathanson, Fred S. Gorelick, John Hwa, Renata
Belfort-DeAguiar, Richard G. Kibbey & Arya Mani * Center for Exocrine Disorders, Department of Molecular and Cell Biology, Boston University Henry M. Goldman School of Dental Medicine,
Boston, MA, USA András Szabó & Miklós Sahin-Tóth * Department of Medicine, NYU Medical Center, New York, NY, USA Ephraim Weiss * Department of Genetics, Yale School of Medicine, New
Haven, CT, USA Shrikant Mane & Arya Mani * Laboratory of Human Genetics and Genomics, The Rockefeller University, New York, NY, USA Richard P. Lifton * Department of Pathology, Yale
School of Medicine, New Haven, CT, USA Adebowale Adeniran Authors * Fatemehsadat Esteghamat View author publications You can also search for this author inPubMed Google Scholar * James S.
Broughton View author publications You can also search for this author inPubMed Google Scholar * Emily Smith View author publications You can also search for this author inPubMed Google
Scholar * Rebecca Cardone View author publications You can also search for this author inPubMed Google Scholar * Tarun Tyagi View author publications You can also search for this author
inPubMed Google Scholar * Mateus Guerra View author publications You can also search for this author inPubMed Google Scholar * András Szabó View author publications You can also search for
this author inPubMed Google Scholar * Nelson Ugwu View author publications You can also search for this author inPubMed Google Scholar * Mitra V. Mani View author publications You can also
search for this author inPubMed Google Scholar * Bani Azari View author publications You can also search for this author inPubMed Google Scholar * Gerald Kayingo View author publications You
can also search for this author inPubMed Google Scholar * Sunny Chung View author publications You can also search for this author inPubMed Google Scholar * Mohsen Fathzadeh View author
publications You can also search for this author inPubMed Google Scholar * Ephraim Weiss View author publications You can also search for this author inPubMed Google Scholar * Jeffrey Bender
View author publications You can also search for this author inPubMed Google Scholar * Shrikant Mane View author publications You can also search for this author inPubMed Google Scholar *
Richard P. Lifton View author publications You can also search for this author inPubMed Google Scholar * Adebowale Adeniran View author publications You can also search for this author
inPubMed Google Scholar * Michael H. Nathanson View author publications You can also search for this author inPubMed Google Scholar * Fred S. Gorelick View author publications You can also
search for this author inPubMed Google Scholar * John Hwa View author publications You can also search for this author inPubMed Google Scholar * Miklós Sahin-Tóth View author publications
You can also search for this author inPubMed Google Scholar * Renata Belfort-DeAguiar View author publications You can also search for this author inPubMed Google Scholar * Richard G. Kibbey
View author publications You can also search for this author inPubMed Google Scholar * Arya Mani View author publications You can also search for this author inPubMed Google Scholar
CONTRIBUTIONS F.E. contributed primarily to designing and performing the experiments, as well as to preparing the figures and manuscript. J.S.B., R.C., T.T., A.S., N.U., M.V.M., M.G., B.A.,
S.C., M.F. and A.A. were involved with performing the experiments. S.M., R.P.L., M.H.N., J.H., M.S.-T. and R.G.K. were involved in the design and supervision of certain aspects of the
project. G.K., E.W., J.B. and E.S. were involved in patient recruitment and clinical characterizations. R.B.-D. carried out all of the OGTT and hyperglycemic clamp studies. N.U. was involved
in the analysis of the genetic data. F.S.G. was involved in the design and supervision of aspects of the project, and participated in manuscript writing. A.M. designed the study and oversaw
its implementation, supervised all aspects of the project from performing the experiments to the analysis of all data, and wrote the manuscript. CORRESPONDING AUTHOR Correspondence to Arya
Mani. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE: Springer Nature remains neutral with regard to
jurisdictional claims in published maps and institutional affiliations. INTEGRATED SUPPLEMENTARY INFORMATION SUPPLEMENTARY FIGURE 1 SELECTED LABORATORY AND CLINICAL DATA IN P.D121N CARRIERS
VS. NON-CARRIERS OF THE KINDRED CAD-2001. A, Plasma TG levels (mg/dl; mean ± s.e.m.; _n_ = 14 non-carriers vs. n = 10 carriers; Student’s _t_-test, two-sided at **_P_ < 0.0001). B, BMI
(kg/m2) (mean ± s.e.m. ; _n_ = 14 non-carriers vs. n = 13 carriers; Student’s _t_-test, two-sided at **_P_ = 0.002). C, Plasma cortisol levels (μg/ml; mean ± s.e.m.; _n_ = 8 non-carriers vs.
_n_ = 8 carriers; Student’s _t_-test, two-sided at *_P_ = 0.011). D, Plasma GLP1 levels (pm/L; mean ± s.e.m; _n_ = 8 non-carriers vs. _n_ = 8 carriers; Student’s _t_-test, two-sided, _P_ =
n.s). E, Plasma globular adiponectin levels (ng/ml; mean ± s.e.m.; _n_ = 8 non-carriers vs. _n_ = 7 carriers, Student’s _t_-test, two-sided; _P_ = n.s). TG, triglycerides; BMI, body mass
index; GLP1, Glucagon-like peptide 1. SUPPLEMENTARY FIGURE 2 VALIDATION OF CELA2A ANTIBODY USED IN WESTERN BLOT ANALYSIS AND IMMUNOHISTOCHEMISTRY. A, Western blot image of different
quantities of rCela2a using CELA2A-specific antibody and CELA2A antibody (Sigma-Aldrich, SAB1104798) pre-blocked with rCela2a (MyBiosource, MBS1246487). The 25-kDa rCela2a bands are almost
invisible in the western blot carried out using pre-blocked antibody (_n_ = 2 independent experiments). B, Western blot analysis using the supernatants of the 293T cells overexpressing
either empty vector, WT-CELA2A or p.D121N His-CELA2A. The 25-kDa and 75-kDa His-CELA2A bands are no longer visible in the western blot carried out using pre-blocked antibody; the MW marker
(middle) has been greatly overexposed to allow visualization of the CELA2A bands (_n_ = 2 independent experiments). C, Immunohistochemistry staining of mouse skeletal muscle for CELA2A in WT
mice injected with rCela2a vs. saline. IgG staining was used as negative control (_n_ = 5 independent experiments). D, Validation of the ELISA kit assay for human CELA2A using known
concentrations of purified WT-CELA2A and p.D121N-CELA2A represented as bar charts with mean ± s.e.m. The vehicle served as a negative control (_n_ = 3 independent experiments; triplicates of
one experiments have been represented). E, Whole membrane of the western blot for Cela2a, shown in Fig. 3b. SUPPLEMENTARY FIGURE 3 TISSUE DISTRIBUTION OF CELA2A. A-C, Immunohistochemical
staining of mouse adrenal gland cortex and medulla (A) (_n_ = 3 independent experiments), small intestine (B) (_n_ = 3 independent experiments), and exocrine pancreas (C) (_n_ = 5
independent experiments). Scale bar, 100 μm. Arrows indicate lymphoid follicles in the small intestine. Different zones in the adrenal gland are shown. D, Western blot analysis of CELA2A in
human cadaveric liver, white adipose tissue (WAT) and pancreas. SUPPLEMENTARY FIGURE 4 EXPRESSION OF CELA2A IN DISEASE STATES FROM GENE EXPRESSION OMNIBUS (GEO) DATASETS AND INSULIN, GLUCOSE
AND GLUCAGON LEVELS BEFORE AND AFTER THE MEAL IN HUMAN SUBJECTS. A, Relative expression of CELA2A mRNA in vastus lateralis muscle samples from insulin-resistant obese (_n_ = 5) and insulin
sensitive (_n_ = 5) Pima Indians. B, Beta-cell enriched pancreatic tissues obtained from subjects with T2D (_n_ = 10) and without T2D (_n_ = 10), shown as dot plots (mean ± s.e.m). Data were
derived from GEO database (see the references in the text). Statistical analyses were carried out using two-sided Student’s _t_-test; _P_ = 0.0115 and _P_ = 0.0150, respectively. C,
Glucagon level (pg/dl; mean ± s.e.m) in p.D121N-CELA2A carriers compared to controls (_n_ = 7 control samples vs. 8 p.D121N-carriers). Statistical analyses were carried out using two-sided
Student’s _t_-test, _P_ = 0.033. D,E, Plasma glucagon levels (pg/dl; mean ± s.e.m) in fast/fed healthy individuals and correlation with plasma CELA2A in healthy subjects before and after
meal (_n_ = 8 samples). Statistical analyses were carried out using two-sided Student’s _t_-test; _P_ = 0.049. Correlation coefficient (_r_2 = -0.72) for E was performed using GraphPad. F,
CELA2A to glucose ratios (mean ± s.e.m) at 60 min hyperglycemic clamp and OGTT represented as bar chart (_n_ = 5 samples, Student’s _t_-test, two-sided, _P_ = n.s.). G,H, Average values of
CELA2A and glucagon (pg/dl; mean ± s.e.m) during hyperglycemic clamp and OGTT studies (_n_ = 5 samples). OGTT, oral glucose tolerance test. AU, arbitrary units. All human studies were
performed only once. SUPPLEMENTARY FIGURE 5 RCELA2A ADMINISTRATION IN VIVO AND IN HUMAN ISLETS. A,B, Plasma insulin and glucose levels (mean ± s.e.m.) after intravenous administration of
rCela2a to normoglycemic wild-type C57BL/6 mice (_n_ = 5 in each group). Statistical analyses were carried out using two-sided Student’s _t_-test. *_P_ < 0.05. C,D, Insulin and C-peptide
secretion of human islets in response to WT-CELA2A. Response to KCl is used as a positive control and test of viability. Violin plots represent median, minimum and maximum. Statistical
analyses were carried out using two-sided Student’s _t_-test per condition (_n_ = 4). **_P_ <0.01. E, Insulin secretion of human islets in response to WT-CELA2A (human) compared to
rCela2a (mouse) represented in bar charts (mean ± s.e.m; _n_ = 4 samples). Statistical analyses were carried out using two-sided Student’s _t_-test per conditions (***_P_ <0.001).
Response to KCl is used as a positive control and test of viability. SUPPLEMENTARY FIGURE 6 QUANTIFICATION OF INSULIN SIGNALING ACTIVATION BY WT-CELA2A AND P.D121N-CELA2A PROTEIN. A-E, Plots
show relative intensities compared to controls for the phosphoproteins in the western blots shown in Fig. 5g displayed as bar charts (mean ± s.e.m.; _n_ = 2 independent experiments).
Statistical analyses were performed using one-way ANOVA. *_P_ < 0.05, **_P_ < 0.001. SUPPLEMENTARY FIGURE 7 WHOLE BLOT FIGURES USED IN THE STUDY. Whole blots from western blot analysis
of CELA2A in human serum in Fig. 3d; insulin/mTOR signaling pathways in 3T3L1 cells treated with insulin, WT- or p.D121N-CELA2A, and predigested insulin with WT- or p.D121N-CELA2A in Fig.
3g; Coomassie blue and western blot of GPIIb/IIIa in Fig. 6e, f. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION Supplementary Figs. 1–7 and Supplementary Tables 1–6 REPORTING SUMMARY
RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Esteghamat, F., Broughton, J.S., Smith, E. _et al._ _CELA2A_ mutations predispose to early-onset
atherosclerosis and metabolic syndrome and affect plasma insulin and platelet activation. _Nat Genet_ 51, 1233–1243 (2019). https://doi.org/10.1038/s41588-019-0470-3 Download citation *
Received: 01 May 2018 * Accepted: 20 June 2019 * Published: 29 July 2019 * Issue Date: August 2019 * DOI: https://doi.org/10.1038/s41588-019-0470-3 SHARE THIS ARTICLE Anyone you share the
following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative






