- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Alzheimer disease is more than a pure proteopathy. Chronic neuroinflammation stands out during the pathogenesis of the disease and in turn modulates disease progression. The central
nervous system (CNS) is separated from the blood circulation by the blood–brain barrier. In Alzheimer disease, neuroinflammation heavily relies on innate immune responses that are primarily
mediated by CNS-resident microglia. _APOE_ (which encodes apolipoprotein E) is the strongest genetic risk factor for Alzheimer disease, and APOE was recently shown to affect the disease in
part through its immunomodulatory function. This function of APOE is likely linked to triggering receptor expressed on myeloid cells 2 (TREM2), which is expressed by microglia in the CNS.
Here, we review the rapidly growing literature on the role of disease-associated microglia, TREM2 and APOE in the pathogenesis of Alzheimer disease and present an integrated view of innate
immune function in Alzheimer disease. Access through your institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through
your institution Access Nature and 54 other Nature Portfolio journals Get Nature+, our best-value online-access subscription $32.99 / 30 days cancel any time Learn more Subscribe to this
journal Receive 12 print issues and online access $209.00 per year only $17.42 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now
Prices may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer
support SIMILAR CONTENT BEING VIEWED BY OTHERS NEUROINFLAMMATION IN ALZHEIMER DISEASE Article 09 December 2024 IMMUNE MECHANISMS AND SHARED IMMUNE TARGETS IN NEURODEGENERATIVE DISEASES
Article 16 December 2024 MONOCYTE-DERIVED MACROPHAGES ACT AS REINFORCEMENTS WHEN MICROGLIA FALL SHORT IN ALZHEIMER’S DISEASE Article 06 January 2025 REFERENCES * Alzheimer, A. Über eine
eigenartige Erkrankung der Hirnrinde. _Allg. Z. Psychiatr._ 64, 146–148 (1907). Google Scholar * Jack, C. R. Jr. et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s
pathological cascade. _Lancet Neurol._ 9, 119–128 (2010). CAS PubMed PubMed Central Google Scholar * Bateman, R. J. et al. Clinical and biomarker changes in dominantly inherited
Alzheimer’s disease. _N. Engl. J. Med._ 367, 795–804 (2012). CAS PubMed PubMed Central Google Scholar * Hardy, J. & Selkoe, D. J. The amyloid hypothesis of Alzheimer’s disease:
progress and problems on the road to therapeutics. _Science_ 297, 353–356 (2002). CAS PubMed Google Scholar * Holtzman, D. M., Morris, J. C. & Goate, A. M. Alzheimer’s disease: the
challenge of the second century. _Sci. Transl Med._ 3, 77sr71 (2011). Google Scholar * Pimenova, A. A., Raj, T. & Goate, A. M. Untangling genetic risk for Alzheimer’s disease. _Biol.
Psychiatry_ 83, 300–310 (2017). PubMed PubMed Central Google Scholar * Gjoneska, E. et al. Conserved epigenomic signals in mice and humans reveal immune basis of Alzheimer’s disease.
_Nature_ 518, 365–369 (2015). CAS PubMed PubMed Central Google Scholar * Brown, G. C. & Neher, J. J. Microglial phagocytosis of live neurons. _Nat. Rev. Neurosci._ 15, 209–216
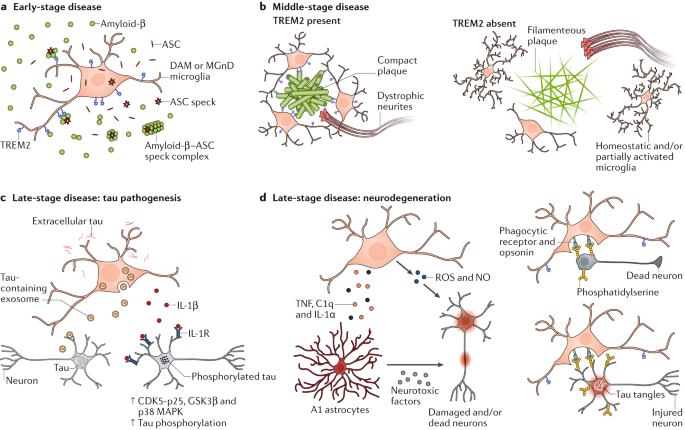
(2014). CAS PubMed Google Scholar * Liddelow, S. A. et al. Neurotoxic reactive astrocytes are induced by activated microglia. _Nature_ 541, 481–487 (2017). THIS STUDY DEFINES THE ROLES OF
A1 ASTROCYTES IN NEURODEGENERATIVE DISEASES AND DEMONSTRATES AN ESSENTIAL ROLE OF MICROGLIA–ASTROCYTES CROSSTALK IN A1 ASTROCYTIC ACTIVATION. CAS PubMed PubMed Central Google Scholar *
Kaushal, V. et al. Neuronal NLRP1 inflammasome activation of Caspase-1 coordinately regulates inflammatory interleukin-1-β production and axonal degeneration-associated caspase-6 activation.
_Cell Death Differ._ 22, 1676–1686 (2015). CAS PubMed PubMed Central Google Scholar * Tan, M. S. et al. Amyloid-β induces NLRP1-dependent neuronal pyroptosis in models of Alzheimer’s
disease. _Cell Death Dis._ 5, e1382 (2014). CAS PubMed PubMed Central Google Scholar * Ginhoux, F. et al. Fate mapping analysis reveals that adult microglia derive from primitive
macrophages. _Science_ 330, 841–845 (2010). CAS PubMed PubMed Central Google Scholar * Ajami, B., Bennett, J. L., Krieger, C., Tetzlaff, W. & Rossi, F. M. Local self-renewal can
sustain CNS microglia maintenance and function throughout adult life. _Nat. Neurosci._ 10, 1538–1543 (2007). CAS PubMed Google Scholar * Paolicelli, R. C. et al. Synaptic pruning by
microglia is necessary for normal brain development. _Science_ 333, 1456–1458 (2011). CAS PubMed Google Scholar * Stevens, B. et al. The classical complement cascade mediates CNS synapse
elimination. _Cell_ 131, 1164–1178 (2007). CAS PubMed Google Scholar * Cunningham, C. L., Martinez-Cerdeno, V. & Noctor, S. C. Microglia regulate the number of neural precursor cells
in the developing cerebral cortex. _J. Neurosci._ 33, 4216–4233 (2013). CAS PubMed PubMed Central Google Scholar * Wakselman, S. et al. Developmental neuronal death in hippocampus
requires the microglial CD11b integrin and DAP12 immunoreceptor. _J. Neurosci._ 28, 8138–8143 (2008). CAS PubMed PubMed Central Google Scholar * Marin-Teva, J. L. et al. Microglia
promote the death of developing Purkinje cells. _Neuron_ 41, 535–547 (2004). CAS PubMed Google Scholar * Davalos, D. et al. ATP mediates rapid microglial response to local brain injury in
vivo. _Nat. Neurosci._ 8, 752–758 (2005). CAS PubMed Google Scholar * Nimmerjahn, A., Kirchhoff, F. & Helmchen, F. Resting microglial cells are highly dynamic surveillants of brain
parenchyma in vivo. _Science_ 308, 1314–1318 (2005). CAS PubMed Google Scholar * Kettenmann, H., Hanisch, U.-K., Noda, M. & Verkhratsky, A. Physiology of microglia. _Physiol. Rev._
91, 461–553 (2011). CAS PubMed Google Scholar * Wu, Y., Dissing-Olesen, L., MacVicar, B. A. & Stevens, B. Microglia: dynamic mediators of synapse development and plasticity. _Trends
Immunol._ 36, 605–613 (2015). PubMed PubMed Central Google Scholar * Martinez, F. O. & Gordon, S. The M1 and M2 paradigm of macrophage activation: time for reassessment. _F1000Prime
Rep._ 6, 13 (2014). PubMed PubMed Central Google Scholar * Boche, D., Perry, V. H. & Nicoll, J. A. Review: activation patterns of microglia and their identification in the human
brain. _Neuropathol. Appl. Neurobiol._ 39, 3–18 (2013). CAS PubMed Google Scholar * Mosser, D. M. & Edwards, J. P. Exploring the full spectrum of macrophage activation. _Nat. Rev.
Immunol._ 8, 958–969 (2008). CAS PubMed PubMed Central Google Scholar * Murray, P. J. et al. Macrophage activation and polarization: nomenclature and experimental guidelines. _Immunity_
41, 14–20 (2014). CAS PubMed PubMed Central Google Scholar * Keren-Shaul, H. et al. A Unique microglia type associated with restricting development of Alzheimer’s disease. _Cell_ 169,
1276–1290 (2017). CAS PubMed Google Scholar * Krasemann, S. et al. The TREM2-APOE pathway drives the transcriptional phenotype of dysfunctional microglia in neurodegenerative diseases.
_Immunity_ 47, 566–581 (2017). THIS WORK AND REFERENCE 27 RAISE THE CONCEPT OF A NEURODEGENERATIVE MICROGLIAL PHENOTYPE. THEY DEFINE THE MOLECULAR SIGNATURES OF THE PHENOTYPE AND DEMONSTRATE
THE REQUIREMENT OF TREM2 AND APOE FOR ITS ACTIVATION. CAS PubMed PubMed Central Google Scholar * Chakrabarty, P., Herring, A., Ceballos-Diaz, C., Das, P. & Golde, T. E. Hippocampal
expression of murine TNFα results in attenuation of amyloid deposition in vivo. _Mol. Neurodegener._ 6, 16 (2011). CAS PubMed PubMed Central Google Scholar * Chakrabarty, P. et al.
IFN-gamma promotes complement expression and attenuates amyloid plaque deposition in amyloid β precursor protein transgenic mice. _J. Immunol._ 184, 5333–5343 (2010). CAS PubMed Google
Scholar * Chakrabarty, P. et al. Massive gliosis induced by interleukin-6 suppresses Aβ deposition in vivo: evidence against inflammation as a driving force for amyloid deposition. _FASEB
J._ 24, 548–559 (2010). CAS PubMed PubMed Central Google Scholar * Guillot-Sestier, M. V. et al. Il10 deficiency rebalances innate immunity to mitigate Alzheimer-like pathology. _Neuron_
85, 534–548 (2015). CAS PubMed PubMed Central Google Scholar * Chakrabarty, P. et al. IL-10 alters immunoproteostasis in APP mice, increasing plaque burden and worsening cognitive
behavior. _Neuron_ 85, 519–533 (2015). CAS PubMed PubMed Central Google Scholar * Chakrabarty, P. et al. Hippocampal expression of murine IL-4 results in exacerbation of amyloid
deposition. _Mol. Neurodegener._ 7, 36 (2012). CAS PubMed PubMed Central Google Scholar * Vom Berg, J. et al. Inhibition of IL-12/IL-23 signaling reduces Alzheimer’s disease-like
pathology and cognitive decline. _Nat. Med._ 18, 1812–1819 (2012). CAS PubMed Google Scholar * Kiyota, T. et al. CNS expression of anti-inflammatory cytokine interleukin-4 attenuates
Alzheimer’s disease-like pathogenesis in APP+PS1 bigenic mice. _FASEB J._ 24, 3093–3102 (2010). CAS PubMed PubMed Central Google Scholar * Qiao, X., Cummins, D. J. & Paul, S. M.
Neuroinflammation-induced acceleration of amyloid deposition in the APPV717F transgenic mouse. _Eur. J. Neurosci._ 14, 474–482 (2001). CAS PubMed Google Scholar * Spangenberg, E. E. et
al. Eliminating microglia in Alzheimer’s mice prevents neuronal loss without modulating amyloid-β pathology. _Brain_ 139, 1265–1281 (2016). PubMed PubMed Central Google Scholar *
Grathwohl, S. A. et al. Formation and maintenance of Alzheimer’s disease β-amyloid plaques in the absence of microglia. _Nat. Neurosci._ 12, 1361–1363 (2009). CAS PubMed PubMed Central
Google Scholar * Sosna, J. et al. Early long-term administration of the CSF1R inhibitor PLX3397 ablates microglia and reduces accumulation of intraneuronal amyloid, neuritic plaque
deposition and pre-fibrillar oligomers in 5XFAD mouse model of Alzheimer’s disease. _Mol. Neurodegener._ 13, 11 (2018). PubMed PubMed Central Google Scholar * Venegas, C. et al.
Microglia-derived ASC specks cross-seed amyloid-β in Alzheimer’s disease. _Nature_ 552, 355–361 (2017). THIS WORK SHOWS THAT ACTIVATED MICROGLIA PROMOTE AMYLOID-Β SEEDING VIA SECRETING
ADAPTOR PROTEIN ASC SPECKS THAT CROSS-SEED AMYLOID-Β. THIS STUDY TOGETHER WITH REFERENCE 39 SUGGESTS THAT MICROGLIA PARTICIPATE IN THE INITIATION STAGE OF PLAQUE FORMATION BY AFFECTING
AMYLOID-Β SEEDING. CAS PubMed Google Scholar * Baik, S. H., Kang, S., Son, S. M. & Mook-Jung, I. Microglia contributes to plaque growth by cell death due to uptake of amyloid β in the
brain of Alzheimer’s disease mouse model. _Glia_ 64, 2274–2290 (2016). PubMed Google Scholar * Yin, Z. et al. Immune hyperreactivity of Aβ plaque-associated microglia in Alzheimer’s
disease. _Neurobiol. Aging_ 55, 115–122 (2017). CAS PubMed Google Scholar * Ulrich, J. D. et al. Altered microglial response to Aβ plaques in APPPS1-21 mice heterozygous for TREM2. _Mol.
Neurodegener._ 9, 20 (2014). PubMed PubMed Central Google Scholar * Jay, T. R. et al. TREM2 deficiency eliminates TREM2+ inflammatory macrophages and ameliorates pathology in Alzheimer’s
disease mouse models. _J. Exp. Med._ 212, 287–295 (2015). CAS PubMed PubMed Central Google Scholar * Wang, Y. et al. TREM2 lipid sensing sustains the microglial response in an
Alzheimer’s disease model. _Cell_ 160, 1061–1071 (2015). CAS PubMed PubMed Central Google Scholar * Jay, T. R. et al. Disease progression-dependent effects of TREM2 deficiency in a mouse
model of Alzheimer’s disease. _J. Neurosci._ 37, 637–647 (2017). REFERENCES 44–47 SHOW THAT TREM2 PROMOTES MICROGLIAL CLUSTERING AROUND AMYLOID-Β PLAQUES AND DEMONSTRATE A DISEASE
STAGE-DEPENDENT EFFECT OF TREM2 DEFICIENCY ON AMYLOID-Β PATHOLOGY. CAS PubMed PubMed Central Google Scholar * Wang, Y. et al. TREM2-mediated early microglial response limits diffusion
and toxicity of amyloid plaques. _J. Exp. Med._ 213, 667–675 (2016). CAS PubMed PubMed Central Google Scholar * Yuan, P. et al. TREM2 haplodeficiency in mice and humans impairs the
microglia barrier function leading to decreased amyloid compaction and severe axonal dystrophy. _Neuron_ 90, 724–739 (2016). REFERENCES 48 AND 49 DEMONSTRATE A MAJOR TREM2-DEPENDENT FUNCTION
OF PLAQUE-ASSOCIATED MICROGLIA TO TRIM AND COMPACT PLAQUES AND TO SERVE AS A BARRIER TO REDUCE NEURITIC DYSTROPHY. CAS PubMed PubMed Central Google Scholar * Zhao, Y. et al. TREM2 is a
receptor for β-amyloid that mediates microglial function. _Neuron_ 97, 1023–1031 (2018). CAS PubMed PubMed Central Google Scholar * Zhang, Y. et al. An RNA-sequencing transcriptome and
splicing database of glia, neurons, and vascular cells of the cerebral cortex. _J. Neurosci._ 34, 11929–11947 (2014). CAS PubMed PubMed Central Google Scholar * Lee, C. Y. D. et al.
Elevated TREM2 gene dosage reprograms microglia responsivity and ameliorates pathological phenotypes in Alzheimer’s disease models. _Neuron_ 97, 1032–1048 (2018). CAS PubMed PubMed Central
Google Scholar * Yamada, K. et al. In vivo microdialysis reveals age-dependent decrease of brain interstitial fluid tau levels in P301S human tau transgenic mice. _J. Neurosci._ 31,
13110–13117 (2011). CAS PubMed PubMed Central Google Scholar * Clavaguera, F., Hench, J., Goedert, M. & Tolnay, M. Invited review: Prion-like transmission and spreading of tau
pathology. _Neuropathol. Appl. Neurobiol._ 41, 47–58 (2015). CAS PubMed Google Scholar * Takeda, S. et al. Neuronal uptake and propagation of a rare phosphorylated high-molecular-weight
tau derived from Alzheimer’s disease brain. _Nat. Commun._ 6, 8490 (2015). CAS PubMed Google Scholar * Bolos, M. et al. Direct evidence of internalization of tau by microglia in vitro and
in vivo. _J. Alzheimers Dis._ 50, 77–87 (2016). CAS PubMed Google Scholar * Asai, H. et al. Depletion of microglia and inhibition of exosome synthesis halt tau propagation. _Nat.
Neurosci._ 18, 1584–1593 (2015). CAS PubMed PubMed Central Google Scholar * Yoshiyama, Y. et al. Synapse loss and microglial activation precede tangles in a P301S tauopathy mouse model.
_Neuron_ 53, 337–351 (2007). CAS PubMed Google Scholar * Kitazawa, M., Oddo, S., Yamasaki, T. R., Green, K. N. & LaFerla, F. M. Lipopolysaccharide-induced inflammation exacerbates tau
pathology by a cyclin-dependent kinase 5-mediated pathway in a transgenic model of Alzheimer’s disease. _J. Neurosci._ 25, 8843–8853 (2005). CAS PubMed PubMed Central Google Scholar *
Li, Y., Liu, L., Barger, S. W. & Griffin, W. S. Interleukin-1 mediates pathological effects of microglia on tau phosphorylation and on synaptophysin synthesis in cortical neurons through
a p38-MAPK pathway. _J. Neurosci._ 23, 1605–1611 (2003). CAS PubMed PubMed Central Google Scholar * Kitazawa, M. et al. Blocking IL-1 signaling rescues cognition, attenuates tau
pathology, and restores neuronal β-catenin pathway function in an Alzheimer’s disease model. _J. Immunol._ 187, 6539–6549 (2011). CAS PubMed Google Scholar * Bhaskar, K. et al. Regulation
of tau pathology by the microglial fractalkine receptor. _Neuron_ 68, 19–31 (2010). CAS PubMed PubMed Central Google Scholar * Maphis, N. et al. Reactive microglia drive tau pathology
and contribute to the spreading of pathological tau in the brain. _Brain_ 138, 1738–1755 (2015). PubMed PubMed Central Google Scholar * Nash, K. R. et al. Fractalkine overexpression
suppresses tau pathology in a mouse model of tauopathy. _Neurobiol. Aging_ 34, 1540–1548 (2013). CAS PubMed PubMed Central Google Scholar * Bemiller, S. M. et al. TREM2 deficiency
exacerbates tau pathology through dysregulated kinase signaling in a mouse model of tauopathy. _Mol. Neurodegener._ 12, 74 (2017). PubMed PubMed Central Google Scholar * Jiang, T. et al.
Silencing of TREM2 exacerbates tau pathology, neurodegenerative changes, and spatial learning deficits in P301S tau transgenic mice. _Neurobiol. Aging_ 36, 3176–3186 (2015). CAS PubMed
Google Scholar * Leyns, C. E. G. et al. TREM2 deficiency attenuates neuroinflammation and protects against neurodegeneration in a mouse model of tauopathy. _Proc. Natl Acad. Sci. USA_ 114,
11524–11529 (2017). THIS WORK SHOWS THAT DAMPENING NEURODEGENERATIVE MICROGLIAL ACTIVATION VIA TREM2 DELETION REDUCES NEURODEGENERATION AT AN ADVANCED DISEASE STAGE IN A TAUOPATHY MOUSE
MODEL, SUPPORTING A ROLE OF MICROGLIA IN MODULATING NEURODEGENERATION. CAS PubMed PubMed Central Google Scholar * Jiang, T. et al. TREM2 modifies microglial phenotype and provides
neuroprotection in P301S tau transgenic mice. _Neuropharmacology_ 105, 196–206 (2016). CAS PubMed Google Scholar * Shi, Y. et al. ApoE4 markedly exacerbates tau-mediated neurodegeneration
in a mouse model of tauopathy. _Nature_ 549, 523–527 (2017). THIS STUDY DEMONSTRATES AN AMYLOID-Β-INDEPENDENT ROLE OF APOE IN REGULATING NEURODEGENERATION AND NEUROINFLAMMATION IN THE
SETTING OF A TAUOPATHY. THE PROTECTIVE EFFECT OF APOE DEFICIENCY ON NEURODEGENERATION IS IN LINE WITH THAT OF TREM2. PubMed PubMed Central Google Scholar * Kraft, A. W. et al. Attenuating
astrocyte activation accelerates plaque pathogenesis in APP/PS1 mice. _FASEB J._ 27, 187–198 (2013). CAS PubMed PubMed Central Google Scholar * Liddelow, S. A. & Barres, B. A.
Reactive astrocytes: production, function, and therapeutic potential. _Immunity_ 46, 957–967 (2017). CAS PubMed Google Scholar * Zhang, Y. & Barres, B. A. Astrocyte heterogeneity: an
underappreciated topic in neurobiology. _Curr. Opin. Neurobiol._ 20, 588–594 (2010). CAS PubMed Google Scholar * Vainchtein, I. D. et al. Astrocyte-derived interleukin-33 promotes
microglial synapse engulfment and neural circuit development. _Science_ 359, 1269–1273 (2018). CAS PubMed PubMed Central Google Scholar * Chung, W. S. et al. Astrocytes mediate synapse
elimination through MEGF10 and MERTK pathways. _Nature_ 504, 394–400 (2013). CAS PubMed PubMed Central Google Scholar * Chung, W. S. et al. Novel allele-dependent role for APOE in
controlling the rate of synapse pruning by astrocytes. _Proc. Natl Acad. Sci. USA_ 113, 10186–10191 (2016). CAS PubMed PubMed Central Google Scholar * Sofroniew, M. V. Astrocyte barriers
to neurotoxic inflammation. _Nat. Rev. Neurosci._ 16, 249–263 (2015). CAS PubMed PubMed Central Google Scholar * Zamanian, J. L. et al. Genomic analysis of reactive astrogliosis. _J.
Neurosci._ 32, 6391–6410 (2012). CAS PubMed PubMed Central Google Scholar * Lian, H. et al. NFκB-activated astroglial release of complement C3 compromises neuronal morphology and
function associated with Alzheimer’s disease. _Neuron_ 85, 101–115 (2015). CAS PubMed Google Scholar * Lian, H. et al. Astrocyte-microglia cross talk through complement activation
modulates amyloid pathology in mouse models of Alzheimer’s disease. _J. Neurosci._ 36, 577–589 (2016). CAS PubMed PubMed Central Google Scholar * Li, Q. & Barres, B. A. Microglia and
macrophages in brain homeostasis and disease. _Nat. Rev. Immunol._ 18, 225–242 (2017). CAS PubMed Google Scholar * Varvel, N. H. et al. Microglial repopulation model reveals a robust
homeostatic process for replacing CNS myeloid cells. _Proc. Natl Acad. Sci. USA_ 109, 18150–18155 (2012). CAS PubMed PubMed Central Google Scholar * Prokop, S. et al. Impact of
peripheral myeloid cells on amyloid-β pathology in Alzheimer’s disease-like mice. _J. Exp. Med._ 212, 1811–1818 (2015). CAS PubMed PubMed Central Google Scholar * Varvel, N. H. et al.
Replacement of brain-resident myeloid cells does not alter cerebral amyloid-β deposition in mouse models of Alzheimer’s disease. _J. Exp. Med._ 212, 1803–1809 (2015). CAS PubMed PubMed
Central Google Scholar * Michaud, J. P., Bellavance, M. A., Prefontaine, P. & Rivest, S. Real-time in vivo imaging reveals the ability of monocytes to clear vascular amyloid β. _Cell
Rep._ 5, 646–653 (2013). CAS PubMed Google Scholar * Baik, S. H. et al. Migration of neutrophils targeting amyloid plaques in Alzheimer’s disease mouse model. _Neurobiol. Aging_ 35,
1286–1292 (2014). CAS PubMed PubMed Central Google Scholar * Zenaro, E. et al. Neutrophils promote Alzheimer’s disease-like pathology and cognitive decline via LFA-1 integrin. _Nat.
Med._ 21, 880–886 (2015). CAS PubMed Google Scholar * Kumar, D. K. et al. Amyloid-β peptide protects against microbial infection in mouse and worm models of Alzheimer’s disease. _Sci.
Transl Med._ 8, 340ra372 (2016). Google Scholar * Holtzman, D. M., Herz, J. & Bu, G. Apolipoprotein E and apolipoprotein E receptors: normal biology and roles in Alzheimer disease.
_Cold Spring Harbor Persp. Med._ 2, a006312 (2012). Google Scholar * Bu, G. Apolipoprotein E and its receptors in Alzheimer’s disease: pathways, pathogenesis and therapy. _Nat. Rev.
Neurosci._ 10, 333–344 (2009). CAS PubMed PubMed Central Google Scholar * Boyles, J. K., Pitas, R. E., Wilson, E., Mahley, R. W. & Taylor, J. M. Apolipoprotein E associated with
astrocytic glia of the central nervous system and with nonmyelinating glia of the peripheral nervous system. _J. Clin. Invest._ 76, 1501–1513 (1985). CAS PubMed PubMed Central Google
Scholar * Uchihara, T. et al. ApoE immunoreactivity and microglial cells in Alzheimer’s disease brain. _Neurosci. Lett._ 195, 5–8 (1995). CAS PubMed Google Scholar * Corder, E. H. et al.
Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. _Science_ 261, 921–923 (1993). CAS PubMed Google Scholar * Schmechel, D. E. et al.
Increased amyloid β-peptide deposition in cerebral cortex as a consequence of apolipoprotein E genotype in late-onset Alzheimer disease. _Proc. Natl Acad. Sci. USA_ 90, 9649–9653 (1993).
CAS PubMed PubMed Central Google Scholar * Agosta, F. et al. Apolipoprotein E ε4 is associated with disease-specific effects on brain atrophy in Alzheimer’s disease and frontotemporal
dementia. _Proc. Natl Acad. Sci. USA_ 106, 2018–2022 (2009). CAS PubMed PubMed Central Google Scholar * Strittmatter, W. J. et al. Apolipoprotein E: high-avidity binding to β-amyloid and
increased frequency of type 4 allele in late-onset familial Alzheimer disease. _Proc. Natl Acad. Sci. USA_ 90, 1977–1981 (1993). CAS PubMed PubMed Central Google Scholar * Bales, K. R.
et al. Lack of apolipoprotein E dramatically reduces amyloid β-peptide deposition. _Nat. Genet._ 17, 263–264 (1997). CAS PubMed Google Scholar * Kim, J. et al. Haploinsufficiency of human
APOE reduces amyloid deposition in a mouse model of amyloid-β amyloidosis. _J. Neurosci._ 31, 18007–18012 (2011). CAS PubMed PubMed Central Google Scholar * Holtzman, D. M. et al.
Apolipoprotein E isoform-dependent amyloid deposition and neuritic degeneration in a mouse model of Alzheimer’s disease. _Proc. Natl Acad. Sci. USA_ 97, 2892–2897 (2000). CAS PubMed PubMed
Central Google Scholar * Fagan, A. M. et al. Human and murine ApoE markedly alters Aβ metabolism before and after plaque formation in a mouse model of Alzheimer’s disease. _Neurobiol.
Dis._ 9, 305–318 (2002). CAS PubMed Google Scholar * Castellano, J. M. et al. Human apoE isoforms differentially regulate brain amyloid-peptide clearance. _Sci. Transl Med._ 3, 89ra57
(2011). CAS PubMed PubMed Central Google Scholar * Huynh, T. V., Davis, A. A., Ulrich, J. D. & Holtzman, D. M. Apolipoprotein E and Alzheimer’s disease: the influence of
apolipoprotein E on amyloid-β and other amyloidogenic proteins. _J. Lipid Res._ 58, 824–836 (2017). CAS PubMed PubMed Central Google Scholar * Strittmatter, W. J. et al. Isoform-specific
interactions of apolipoprotein E with microtubule-associated protein tau: implications for Alzheimer disease. _Proc. Natl Acad. Sci. USA_ 91, 11183–11186 (1994). CAS PubMed PubMed Central
Google Scholar * Fleming, L. M., Weisgraber, K. H., Strittmatter, W. J., Troncoso, J. C. & Johnson, G. V. W. Differential binding of apolipoprotein E isoforms to tau and other
cytoskeletal proteins. _Exp. Neurol._ 138, 252–260 (1996). CAS PubMed Google Scholar * Mishra, A. et al. Gene-based association studies report genetic links for clinical subtypes of
frontotemporal dementia. _Brain_ 140, 1437–1446 (2017). PubMed Google Scholar * Tsuang, D. et al. APOE ε4 increases risk for dementia in pure synucleinopathies. _JAMA Neurol._ 70, 223–228
(2013). PubMed PubMed Central Google Scholar * Gallardo, G., Schluter, O. M. & Sudhof, T. C. A molecular pathway of neurodegeneration linking α-synuclein to ApoE and Aβ peptides.
_Nat. Neurosci._ 11, 301–308 (2008). CAS PubMed Google Scholar * Shin, S. et al. Apolipoprotein E mediation of neuro-inflammation in a murine model of multiple sclerosis. _J.
Neuroimmunol._ 271, 8–17 (2014). CAS PubMed PubMed Central Google Scholar * Gale, S. C. et al. APOE4 is associated with enhanced in vivo innate immune responses in human subjects. _J.
Allergy Clin. Immunol._ 134, 127–134 (2014). CAS PubMed PubMed Central Google Scholar * Vitek, M. P., Brown, C. M. & Colton, C. A. APOE genotype-specific differences in the innate
immune response. _Neurobiol. Aging_ 30, 1350–1360 (2009). CAS PubMed Google Scholar * Zhu, Y. et al. APOE genotype alters glial activation and loss of synaptic markers in mice. _Glia_ 60,
559–569 (2012). PubMed PubMed Central Google Scholar * Fessler, M. B. & Parks, J. S. Intracellular lipid flux and membrane microdomains as organizing principles in inflammatory cell
signaling. _J. Immunol._ 187, 1529–1535 (2011). CAS PubMed Google Scholar * Yvan-Charvet, L. et al. ATP-binding cassette transporters and HDL suppress hematopoietic stem cell
proliferation. _Science_ 328, 1689–1693 (2010). CAS PubMed PubMed Central Google Scholar * Murphy, A. J. et al. ApoE regulates hematopoietic stem cell proliferation, monocytosis, and
monocyte accumulation in atherosclerotic lesions in mice. _J. Clin. Invest._ 121, 4138–4149 (2011). CAS PubMed PubMed Central Google Scholar * Okoro, E. U. et al. Apolipoprotein E4 is
deficient in inducing macrophage ABCA1 expression and stimulating the Sp1 signaling pathway. _PLoS ONE_ 7, e44430 (2012). CAS PubMed PubMed Central Google Scholar * Atagi, Y. et al.
Apolipoprotein E is a ligand for triggering receptor expressed on myeloid cells 2 (TREM2). _J. Biol. Chem._ 290, 26043–26050 (2015). THIS WORK DEMONSTRATES THAT APOE IS A RECEPTOR FOR TREM2
AND SHOWS THAT APOE BINDS TO APOPTOTIC NEURONAL CELL SURFACES AND INCREASES TREM2-MEDIATED PHAGOCYTOSIS BY MICROGLIA IN VITRO, SUPPORTING THE APOE OPSONIZATION HYPOTHESIS. CAS PubMed
PubMed Central Google Scholar * Bailey, C. C., DeVaux, L. B. & Farzan, M. The triggering receptor expressed on myeloid cells 2 binds apolipoprotein E. _J. Biol. Chem._ 290, 26033–26042
(2015). CAS PubMed PubMed Central Google Scholar * Jendresen, C., Arskog, V., Daws, M. R. & Nilsson, L. N. The Alzheimer’s disease risk factors apolipoprotein E and TREM2 are linked
in a receptor signaling pathway. _J. Neuroinflamm._ 14, 59 (2017). Google Scholar * Yeh, F. L., Wang, Y., Tom, I., Gonzalez, L. C. & Sheng, M. TREM2 binds to apolipoproteins, including
APOE and CLU/APOJ, and thereby facilitates uptake of amyloid-β by microglia. _Neuron_ 91, 328–340 (2016). CAS PubMed Google Scholar * Ulrich, J. D. et al. ApoE facilitates the microglial
response to amyloid plaque pathology. _J. Exp. Med._ 215, 1047–1058 (2018). THIS WORK DEMONSTRATES THAT APOE IS REQUIRED FOR MICROGLIAL ASSOCIATION WITH PLAQUES TO PERFORM A PLAQUE-TRIMMING
FUNCTION SIMILAR TO THAT OF TREM2, SUPPORTING AN APOE–TREM2 AXIS IN MEDIATING MICROGLIAL FUNCTION. CAS PubMed PubMed Central Google Scholar * Huynh, T. V. et al. Age-dependent effects
of apoE reduction using antisense oligonucleotides in a model of β-amyloidosis. _Neuron_ 96, 1013–1023 (2017). CAS PubMed PubMed Central Google Scholar * Liu, C. C. et al. ApoE4
accelerates early seeding of amyloid pathology. _Neuron_ 96, 1024–1032 (2017). REFERENCES 121 AND 122 SHOW THAT APOE IS ESSENTIAL FOR PLAQUE FORMATION DURING THE INITIAL SEEDING STAGE. CAS
PubMed PubMed Central Google Scholar * Namba, Y., Tomonaga, M., Kawasaki, H., Otomo, E. & Ikeda, K. Apolipoprotein E immunoreactivity in cerebral amyloid deposits and neurofibrillary
tangles in Alzheimer’s disease and kuru plaque amyloid in Creutzfeldt-Jakob disease. _Brain Res._ 541, 163–166 (1991). CAS PubMed Google Scholar * Wisniewski, T. & Frangione, B.
Apolipoprotein E: a pathological chaperone protein in patients with cerebral and systemic amyloid. _Neurosci. Lett._ 135, 235–238 (1992). CAS PubMed Google Scholar * Rodriguez, G.a., Tai,
L. M., LaDu, M. J. & Rebeck, G. W. Human APOE4 increases microglia reactivity at Aβ plaques in a mouse model of Aβ deposition. _J. Neuroinflamm._ 11, 111–111 (2014). Google Scholar *
Huang, Y. et al. Apolipoprotein E fragments present in Alzheimer’s disease brains induce neurofibrillary tangle-like intracellular inclusions in neurons. _Proc. Natl Acad. Sci. USA_ 98,
8838–8843 (2001). CAS PubMed PubMed Central Google Scholar * Farrer, L. A. et al. Allele ε4 of apolipoprotein E shows a dose effect on age at onset of Pick disease. _Exp. Neurol._ 136,
162–170 (1995). CAS PubMed Google Scholar * Brecht, W. J. Neuron-specific apolipoprotein E4 proteolysis is associated with increased tau phosphorylation in brains of transgenic mice. _J.
Neurosci._ 24, 2527–2534 (2004). CAS PubMed PubMed Central Google Scholar * Harris, F. M., Brecht, W. J., Xu, Q., Mahley, R. W. & Huang, Y. Increased tau phosphorylation in
apolipoprotein E4 transgenic mice is associated with activation of extracellular signal-regulated kinase: modulation by zinc. _J. Biol. Chem._ 279, 44795–44801 (2004). CAS PubMed Google
Scholar * Zhou, M. et al. APOE4 induces site-specific tau phosphorylation through calpain-CDK5 signaling pathway in EFAD-Tg mice. _Curr. Alzheimer Res._ 13, 1048–1055 (2016). CAS PubMed
Google Scholar * Pericak-Vance, M. A. et al. Linkage studies in familial Alzheimer disease: evidence for chromosome 19 linkage. _Am. J. Hum. Genet._ 48, 1034–1050 (1991). CAS PubMed
PubMed Central Google Scholar * Neyen, C. D. & Gordon, S. in _eLS_ (John Wiley & Sons, Ltd, 2001). * de Jong, A. Activation of human T cells by CD1 and self-lipids. _Immunol. Rev._
267, 16–29 (2015). PubMed PubMed Central Google Scholar * de Pablo, M. A. & Alvarez de Cienfuegos, G. Modulatory effects of dietary lipids on immune system functions. _Immunol. Cell
Biol._ 78, 31–39 (2000). PubMed Google Scholar * Jonsson, T. et al. Variant of TREM2 associated with the risk of Alzheimer’s disease. _N. Engl. J. Med._ 368, 107–116 (2013). CAS PubMed
Google Scholar * Guerreiro, R. et al. TREM2 variants in Alzheimer’s disease. _N. Engl. J. Med._ 368, 117–127 (2013). CAS PubMed Google Scholar * Colonna, M. & Wang, Y. TREM2
variants: new keys to decipher Alzheimer disease pathogenesis. _Nat. Rev. Neurosci._ 17, 201–207 (2016). CAS PubMed Google Scholar * Ulland, T. K. et al. TREM2 maintains microglial
metabolic fitness in Alzheimer’s disease. _Cell_ 170, 649–663 (2017). CAS PubMed PubMed Central Google Scholar * Poliani, P. L. et al. TREM2 sustains microglial expansion during aging
and response to demyelination. _J. Clin. Invest._ 125, 2161–2170 (2015). PubMed PubMed Central Google Scholar * Takahashi, K., Rochford, C. D. & Neumann, H. Clearance of apoptotic
neurons without inflammation by microglial triggering receptor expressed on myeloid cells-2. _J. Exp. Med._ 201, 647–657 (2005). CAS PubMed PubMed Central Google Scholar * Yeh, F. L.,
Hansen, D. V. & Sheng, M. TREM2, microglia, and neurodegenerative diseases. _Trends Mol. Med._ 23, 512–533 (2017). CAS PubMed Google Scholar * Ulrich, J. D., Ulland, T. K., Colonna,
M. & Holtzman, D. M. Elucidating the role of TREM2 in Alzheimer’s disease. _Neuron_ 94, 237–248 (2017). CAS PubMed Google Scholar * Zheng, H. et al. Opposing roles of the triggering
receptor expressed on myeloid cells 2 and triggering receptor expressed on myeloid cells-like transcript 2 in microglia activation. _Neurobiol. Aging_ 42, 132–141 (2016). CAS PubMed PubMed
Central Google Scholar * Benitez, B. A. et al. Missense variant in TREML2 protects against Alzheimer’s disease. _Neurobiol. Aging_ 35, 1510.e19–1510.e26 (2014). CAS Google Scholar *
Jehle, A. W. et al. ATP-binding cassette transporter A7 enhances phagocytosis of apoptotic cells and associated ERK signaling in macrophages. _J. Cell Biol._ 174, 547–556 (2006). CAS PubMed
PubMed Central Google Scholar * Kim, W. S. et al. Deletion of Abca7 increases cerebral amyloid-β accumulation in the J20 mouse model of Alzheimer’s disease. _J. Neurosci._ 33, 4387–4394
(2013). CAS PubMed PubMed Central Google Scholar * Sakae, N. et al. ABCA7 deficiency accelerates amyloid-β generation and Alzheimer’s neuronal pathology. _J. Neurosci._ 36, 3848–3859
(2016). CAS PubMed PubMed Central Google Scholar * Crehan, H. et al. Complement receptor 1 (CR1) and Alzheimer’s disease. _Immunobiology_ 217, 244–250 (2012). CAS PubMed Google Scholar
* Cunin, P. et al. Clusterin facilitates apoptotic cell clearance and prevents apoptotic cell-induced autoimmune responses. _Cell Death Dis._ 7, e2215 (2016). CAS PubMed PubMed Central
Google Scholar * Huang, K. L. et al. A common haplotype lowers PU.1 expression in myeloid cells and delays onset of Alzheimer’s disease. _Nat. Neurosci._ 20, 1052–1061 (2017). CAS PubMed
PubMed Central Google Scholar * Bradshaw, E. M. et al. CD33 Alzheimer’s disease locus: altered monocyte function and amyloid biology. _Nat. Neurosci._ 16, 848–850 (2013). CAS PubMed
PubMed Central Google Scholar * Griciuc, A. et al. Alzheimer’s disease risk gene CD33 inhibits microglial uptake of amyloid β. _Neuron_ 78, 631–643 (2013). CAS PubMed PubMed Central
Google Scholar * Halle, A. et al. The NALP3 inflammasome is involved in the innate immune response to amyloid-β. _Nat. Immunol._ 9, 857–865 (2008). CAS PubMed PubMed Central Google
Scholar * He, Y., Hara, H. & Nunez, G. Mechanism and regulation of NLRP3 inflammasome activation. _Trends Biochem. Sci._ 41, 1012–1021 (2016). CAS PubMed PubMed Central Google
Scholar * Walsh, J. G., Muruve, D. A. & Power, C. Inflammasomes in the CNS. _Nat. Rev. Neurosci._ 15, 1–14 (2014). Google Scholar * Jablonski, K. A. et al. Novel markers to delineate
murine M1 and M2 macrophages. _PLOS ONE_ 10, e0145342 (2015). PubMed PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS This work was funded by US National Institutes of
Health grants R01AG047644, R01NS090934 and R01NS034467 and support from the JPB Foundation, the Tau Consortium and the Cure Alzheimer Disease Fund to D.M.H. REVIEWER INFORMATION _Nature
Reviews Immunology_ thanks O. Butovsky and M. Heneka for their assistance with the peer review of this manuscript. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Neurology, Hope
Center for Neurological Disorders, Charles F. and Joanne Knight Alzheimer’s Disease Research Center, Washington University School of Medicine, St. Louis, MO, USA Yang Shi & David M.
Holtzman Authors * Yang Shi View author publications You can also search for this author inPubMed Google Scholar * David M. Holtzman View author publications You can also search for this
author inPubMed Google Scholar CONTRIBUTIONS Y.S. wrote the draft of the manuscript. D.M.H. reviewed and edited the manuscript. CORRESPONDING AUTHOR Correspondence to David M. Holtzman.
ETHICS DECLARATIONS COMPETING INTERESTS D.M.H. co-founded and is on the scientific advisory board of C2N Diagnostics. D.M.H. is on the scientific advisory board of Denali, Genentech and
Proclara. D.M.H. consults for AbbVie and Eli Lilly. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and
institutional affiliations. GLOSSARY * Amyloid-β A small peptide that is a major component of amyloid deposits in the brain and cerebrovasculature. It is generated from cleavage of amyloid
precursor protein (APP). Depending on the carboxy-terminal cleavage site, amyloid-β peptides of varying lengths (36–43 amino acids; denoted as Aβ36–Aβ43) can be generated, among which Aβ40
and Aβ42 are the most prevalent species. * Tau A microtubule-binding protein synthesized primarily in neurons. Under normal conditions, tau is most abundantly located in axons and serves to
stabilize microtubules. In Alzheimer disease, tau becomes hyperphosphorylated, dissociates from microtubules, translocates from axons to neuronal cell bodies and dendrites and
self-aggregates to form neurofibrillary tangles. * Aβ42/Aβ40 ratio Aβ42 is more fibrillogenic than Aβ40. The level of Aβ42 produced relative to Aβ40 determines the propensity of amyloid
plaque formation. * Kainic acid A potent neuroexcitatory amino acid that serves as an agonist for kainate-class ionotropic glutamate receptors. High doses of kainic acid induce neuronal
death by overexcitation of neurons. * 5XFAD mice An amyloid-β-depositing mouse model that overexpresses mutant human amyloid precursor protein (APP) carrying the Swedish (K670N and M671L),
Florida (I716V) and London (V717I) mutations linked to familial Alzheimer disease along with human presenilin 1 (PS1) carrying the M146L and L286V mutations. Both transgenes are controlled
under the _Thy1_ promoter. These mice accumulate high levels of intraneuronal Aβ42 around 6 weeks of age, followed by plaque deposition around 2 months of age. * APPSwePSEN1dE9 mice An
amyloid-β-depositing mouse model that expresses a chimeric mouse–human _APP_ transgene carrying the Swedish mutations (K670N and M671L) and a mutant _PSEN1_ transgene lacking exon 9 (dE9)
under the prion promoter. These mice begin to develop amyloid-β pathology around 6 months of age. * Ionized calcium-binding adaptor molecule 1 (IBA1). A microglia marker protein in the
central nervous system that binds calcium and actin. It is involved in RAC GTPase-dependent membrane ruffling and phagocytosis during microglial cell activation. * 3xTg-AD mice A mouse model
that harbours three mutant human genes (_APP_ K670N,M671L, _PSEN1_M146V and _MAPT_ P301L) and sequentially develops amyloid-β pathology and tau pathology starting at 6 months of age. * htau
mice A mouse model that expresses all six human tau isoforms, including 3R and 4R tau, under the endogenous human _MAPT_ promoter and expresses no murine tau. These mice start to develop
tau pathology around 9 months of age. * rTg4510 mice A tauopathy mouse model overexpressing the 0N4R human tau isoform carrying the P301L mutation linked to familial frontotemporal dementia.
Tau transgene expression is largely restricted to the forebrain by the _Camk2a_ promoter and is regulatable by doxycycline. These mice develop tau pathology around 3–4 months of age and
show substantial neuronal loss by 6 months of age. * P301S mice A tauopathy mouse model overexpressing the 1N4R human tau isoform carrying the P301S mutation found in patients with
frontotemporal dementia. These mice begin to accumulate tau pathology at 4–5 months of age and develop severe brain atrophy at 9 months of age. * APOE-targeted replacement mice (APOE-TR
mice). These mice express human apolipoprotein E (APOE) in place of the murine APOE under the endogenous murine _Apoe_ promoter. Therefore, the expression level and pattern of human APOE are
maintained in a physiological form. * APPPS1-21 mice An amyloid-β-depositing mouse model that harbours mutant human transgenes of _APP_ (K670N and M671L) and _PSEN1_ (L166P), which are both
under the control of the _Thy1_ promoter. These mice begin to develop amyloid plaques in the neocortex at approximately 6 weeks of age, followed by deposits in the hippocampus at 3–4 months
of age. * Superoxide dismutase 1 mice (SOD1 mice). A mouse model for amyotrophic lateral sclerosis (ALS) that overexpresses human SOD1 carrying the G93A mutation. These mice recapitulate
phenotypes in human patients with ALS, showing motor neuron loss in the spinal cord and paralysis in one or more limbs. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE
CITE THIS ARTICLE Shi, Y., Holtzman, D.M. Interplay between innate immunity and Alzheimer disease: APOE and TREM2 in the spotlight. _Nat Rev Immunol_ 18, 759–772 (2018).
https://doi.org/10.1038/s41577-018-0051-1 Download citation * Published: 23 August 2018 * Issue Date: December 2018 * DOI: https://doi.org/10.1038/s41577-018-0051-1 SHARE THIS ARTICLE Anyone
you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by
the Springer Nature SharedIt content-sharing initiative