- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
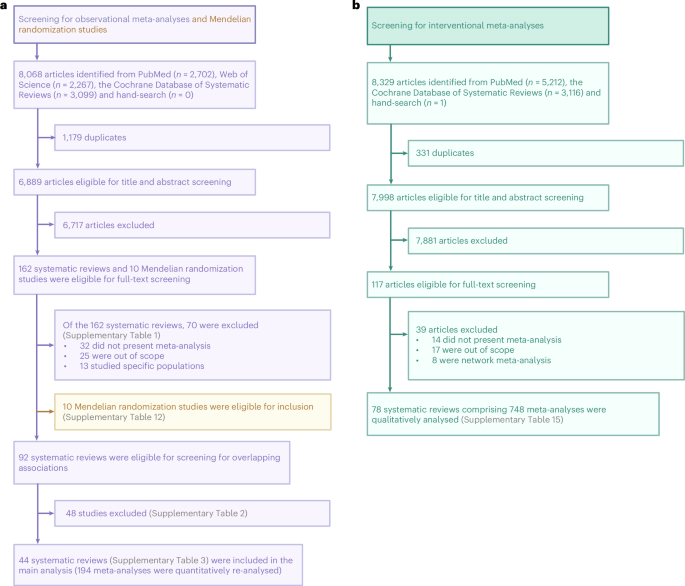
ABSTRACT Maternal adiposity deleteriously affects obstetrical health and has been associated with long-term adverse consequences in offspring. Here we conducted an umbrella review
encompassing 194 observational meta-analyses, 10 Mendelian randomization studies and 748 interventional meta-analyses to appraise the published evidence on the associations between maternal
adiposity and perinatal and offspring outcomes. Evidence grading suggested that 17 (8.8%) observational meta-analyses were supported by convincing evidence for 12 outcomes: maternal
adiposity was associated with an increased risk of caesarean delivery following labour induction, infant mortality, Apgar score <7 at 1 min, antenatal depression, offspring overweight and
obesity, early timing of puberty onset in daughters, attention deficit hyperactivity disorder, cerebral palsy, congenital heart disease and spina bifida (OR/RR ranging from 1.14 to 2.31),
as well as increased offspring body fat percent and fat mass (SMD 0.31 and 0.35, respectively). Among these outcomes, interventional meta-analyses supported that maternal weight loss
interventions significantly reduced the risk of antenatal depression but not low Apgar scores; these interventions also could not reduce offspring fat mass or body fat percent. Evidence from
Mendelian randomization studies supported a causal relationship between maternal adiposity and gestational diabetes mellitus, preeclampsia, birth size and offspring adiposity. Our findings
highlight that while observational meta-analyses reveal associations between maternal adiposity and various adverse perinatal and offspring outcomes, convincing, unbiased evidence or support
from Mendelian randomization studies is limited. Maternal pre-conceptional and prenatal weight loss interventions can reduce some, but not all, of these adverse effects. Access through your
institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution Access Nature and 54 other Nature
Portfolio journals Get Nature+, our best-value online-access subscription $32.99 / 30 days cancel any time Learn more Subscribe to this journal Receive 12 digital issues and online access to
articles $119.00 per year only $9.92 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be subject to local taxes which
are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY
OTHERS THE IMPACT OF MATERNAL OBESITY ON CHILDHOOD NEURODEVELOPMENT Article 28 November 2020 MATERNAL OBESITY AND OFFSPRING CARDIOVASCULAR REMODELLING — THE EFFECT OF PRECONCEPTION AND
ANTENATAL LIFESTYLE INTERVENTIONS: A SYSTEMATIC REVIEW Article Open access 19 June 2024 MODE OF DELIVERY, TYPE OF LABOR, AND MEASURES OF ADIPOSITY FROM CHILDHOOD TO TEENAGE: PROJECT VIVA
Article 16 November 2020 DATA AVAILABILITY The data used to support the findings of this study are collected from already published studies. Data collection form is available at the Open
Science Framework (https://doi.org/10.17605/OSF.IO/97BCS). CODE AVAILABILITY Code is available with open access at the following GitHub repository:
https://github.com/dbyzy/maternal_adiposity_umbrella_review. REFERENCES * Catalano, P. M. & Shankar, K. Obesity and pregnancy: mechanisms of short term and long term adverse consequences
for mother and child. _BMJ_ https://doi.org/10.1136/bmj.j1 (2017). * Flegal, K. M., Kruszon-Moran, D., Carroll, M. D., Fryar, C. D. & Ogden, C. L. Trends in obesity among adults in the
United States, 2005 to 2014. _JAMA_ 315, 2284 (2016). Article CAS PubMed PubMed Central Google Scholar * Creanga, A. A., Catalano, P. M. & Bateman, B. T. Obesity in pregnancy. _N.
Engl. J. Med._ 387, 248–259 (2022). Article CAS PubMed Google Scholar * Poston, L. et al. Preconceptional and maternal obesity: epidemiology and health consequences. _Lancet Diabetes
Endocrinol._ 4, 1025–1036 (2016). Article PubMed Google Scholar * Kalliala, I. et al. Obesity and gynaecological and obstetric conditions: umbrella review of the literature. _BMJ_
https://doi.org/10.1136/bmj.j4511 (2017). * Kurz, C. F. & König, A. N. The causal influence of maternal obesity on preterm birth. _Lancet Diabetes Endocrinol._ 8, 101–103 (2020). Article
CAS PubMed Google Scholar * Flenady, V. et al. Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. _Lancet_ 377, 1331–1340 (2011). Article
PubMed Google Scholar * Aune, D., Saugstad, O. D., Henriksen, T. & Tonstad, S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review
and meta-analysis. _JAMA_ 311, 1536–1546 (2014). Article CAS PubMed Google Scholar * Razaz, N., Villamor, E., Muraca, G. M., Bonamy, A.-K. E. & Cnattingius, S. Maternal obesity and
risk of cardiovascular diseases in offspring: a population-based cohort and sibling-controlled study. _Lancet Diabetes Endocrinol._ 8, 572–581 (2020). Article PubMed Google Scholar *
Hagström, H. et al. Maternal obesity increases the risk and severity of NAFLD in offspring. _J. Hepatol._ 75, 1042–1048 (2021). Article PubMed Google Scholar * Boney, C. M., Verma, A.,
Tucker, R. & Vohr, B. R. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. _Pediatrics_ 115, e290–e296 (2005). Article
PubMed Google Scholar * Hoffman, D. J., Powell, T. L., Barrett, E. S. & Hardy, D. B. Developmental origins of metabolic diseases. _Physiol. Rev._ 101, 739–795 (2021). Article CAS
PubMed Google Scholar * Sanchez, C. E. et al. Maternal pre-pregnancy obesity and child neurodevelopmental outcomes: a meta-analysis. _Obes. Rev._ 19, 464–484 (2018). Article CAS PubMed
Google Scholar * Heslehurst, N. et al. The association between maternal body mass index and child obesity: a systematic review and meta-analysis. _PLoS Med._ 16, e1002817 (2019). Article
PubMed PubMed Central Google Scholar * Nguyen, G. et al. Association between maternal adiposity measures and infant health outcomes: a systematic review and meta-analysis. _Obes. Rev._
23, e13491 (2022). Article PubMed PubMed Central Google Scholar * Ioannidis, J. P. A. Why most discovered true associations are inflated. _Epidemiology_ 19, 640–648 (2008). Article
PubMed Google Scholar * Ioannidis, J. P. A. Why most published research findings are false. _PLoS Med._ 2, e124 (2005). Article PubMed PubMed Central Google Scholar * Dwan, K., Gamble,
C., Williamson, P. R., Kirkham, J. J. & the Reporting Bias Group Systematic review of the empirical evidence of study publication bias and outcome reporting bias—an updated review.
_PLoS ONE_ 8, e66844 (2013). Article CAS PubMed PubMed Central Google Scholar * Smith, G. D. Mendelian randomization: prospects, potentials, and limitations. _Int. J. Epidemiol._ 33,
30–42 (2004). Article PubMed Google Scholar * Chen, J. et al. Dissecting maternal and fetal genetic effects underlying the associations between maternal phenotypes, birth outcomes, and
adult phenotypes: a Mendelian-randomization and haplotype-based genetic score analysis in 10,734 mother–infant pairs. _PLoS Med._ 17, e1003305 (2020). Article CAS PubMed PubMed Central
Google Scholar * Tyrrell, J. et al. Genetic evidence for causal relationships between maternal obesity-related traits and birth weight. _JAMA_ 315, 1129 (2016). Article CAS PubMed PubMed
Central Google Scholar * Bond, T. A. et al. Exploring the causal effect of maternal pregnancy adiposity on offspring adiposity: Mendelian randomisation using polygenic risk scores. _BMC
Med._ 20, 34 (2022). Article CAS PubMed PubMed Central Google Scholar * Davenport, M. H. et al. Impact of prenatal exercise on neonatal and childhood outcomes: a systematic review and
meta-analysis. _Br. J. Sports Med._ 52, 1386–1396 (2018). Article PubMed Google Scholar * Davenport, M. H. et al. Effects of prenatal exercise on incidence of congenital anomalies and
hyperthermia: a systematic review and meta-analysis. _Br. J. Sports Med._ 53, 116–123 (2019). Article PubMed Google Scholar * Davenport, M. H. et al. Impact of prenatal exercise on both
prenatal and postnatal anxiety and depressive symptoms: a systematic review and meta-analysis. _Br. J. Sports Med._ 52, 1376–1385 (2018). Article PubMed Google Scholar * Teede, H. J. et
al. Association of antenatal diet and physical activity–based interventions with gestational weight gain and pregnancy outcomes: a systematic review and meta-analysis. _JAMA Intern. Med._
182, 106 (2022). Article PubMed Google Scholar * Bain, E. et al. Diet and exercise interventions for preventing gestational diabetes mellitus. _Cochrane Database Syst. Rev._
https://doi.org/10.1002/14651858.CD010443.pub2 (2015). * Martínez-Vizcaíno, V. et al. Exercise during pregnancy for preventing gestational diabetes mellitus and hypertensive disorders: an
umbrella review of randomised controlled trials and an updated meta-analysis. _BJOG_ 130, 264–275 (2023). Article PubMed Google Scholar * Blanco, R., Colombo, A. & Suazo, J. Maternal
obesity is a risk factor for orofacial clefts: a meta-analysis. _Br. J. Oral. Maxillofac. Surg._ 53, 699–704 (2015). Article CAS PubMed Google Scholar * Castillo-Laura, H., Santos, I.
S., Quadros, L. C. M. & Matijasevich, A. Maternal obesity and offspring body composition by indirect methods: a systematic review and meta-analysis. _Cad. Saúde Pública_ 31, 2073–2092
(2015). Article PubMed Google Scholar * Chen, W. et al. Prepregnancy BMI, gestational weight gain and risk of childhood atopic dermatitis: a systematic review and meta-analysis. _Pediatr.
Allergy Immunol._ 32, 892–904 (2021). Article PubMed Google Scholar * den Harink, T. et al. Maternal obesity in pregnancy and children’s cardiac function and structure: a systematic
review and meta-analysis of evidence from human studies. _PLoS ONE_ 17, e0275236 (2022). Article Google Scholar * Adane, A. A. The impact of pre-pregnancy body mass index and gestational
weight gain on placental abruption risk: a systematic review and meta-analysis. _Arch. Gynecol. Obstet._ 300, 1201–1210 (2019). Article PubMed Google Scholar * Eapen, A. et al. Mean
differences in maternal body mass index and recurrent pregnancy loss: a systematic review and meta-analysis of observational studies. _Fertil. Steril._ 116, 1341–1348 (2021). Article PubMed
PubMed Central Google Scholar * Eitmann, S. et al. Maternal overnutrition elevates offspring’s blood pressure—a systematic review and meta-analysis. _Paediatr. Perinat. Epid._ 36,
276–287 (2022). Article Google Scholar * Eitmann, S. et al. Maternal overnutrition impairs offspring’s insulin sensitivity: a systematic review and meta-analysis. _Matern. Child Nutr._ 16,
e13031 (2020). Article PubMed PubMed Central Google Scholar * Ellis, J. A., Brown, C. M., Barger, B. & Carlson, N. S. Influence of maternal obesity on labor induction: a systematic
review and meta-analysis. _J. Midwifery Women’s Health_ 64, 55–67 (2019). Article Google Scholar * Habibi, N. et al. Maternal metabolic factors and the association with gestational
diabetes: a systematic review and meta-analysis. _Diabetes Metab. Res._ 38, e3532 (2022). Article Google Scholar * Heslehurst, N. et al. The impact of maternal BMI status on pregnancy
outcomes with immediate short-term obstetric resource implications: a meta-analysis. _Obes. Rev._ 9, 635–683 (2008). Article CAS PubMed Google Scholar * Heslehurst, N. et al. Maternal
body mass index and post-term birth: a systematic review and meta-analysis: maternal BMI and post-term birth. _Obes. Rev._ 18, 293–308 (2017). Article CAS PubMed PubMed Central Google
Scholar * Heslehurst, N. et al. Association between maternal adiposity measures and adverse maternal outcomes of pregnancy: systematic review and meta-analysis. _Obes. Rev._ 23, e13449
(2022). Article PubMed PubMed Central Google Scholar * Hidayat, K., Zou, S. & Shi, B. The influence of maternal body mass index, maternal diabetes mellitus, and maternal smoking
during pregnancy on the risk of childhood-onset type 1 diabetes mellitus in the offspring: systematic review and meta-analysis of observational studies. _Obes. Rev._ 20, 1106–1120 (2019).
Article PubMed Google Scholar * Huang, H.-Y., Chen, H.-L. & Feng, L.-P. Maternal obesity and the risk of neural tube defects in offspring: a meta-analysis. _Obes. Res. Clin. Pract._
11, 188–197 (2017). Article PubMed Google Scholar * Huo, N. et al. Association of maternal body mass index with risk of infant mortality: a dose-response meta-analysis. _Front. Pediatr._
9, 650413 (2021). Article PubMed PubMed Central Google Scholar * Iacovelli, A. et al. Risk factors for abnormally invasive placenta: a systematic review and meta-analysis. _J.
Matern.-Fetal Neonatal Med._ 33, 471–481 (2020). Article PubMed Google Scholar * Jadresić, L. Pre-pregnancy obesity and risk of congenital abnormalities of the kidney and urinary tract
(CAKUT)—systematic review, meta-analysis and ecological study. _Pediatr. Nephrol._ 36, 119–132 (2021). Article PubMed Google Scholar * Lei, X.-Y., Li, Y.-J., Ou, J.-J. & Li, Y.-M.
Association between parental body mass index and autism spectrum disorder: a systematic review and meta-analysis. _Eur. Child Adolesc. Psychiatry_ 28, 933–947 (2019). Article PubMed Google
Scholar * Li, L. et al. Maternal pre-pregnancy overweight/obesity and the risk of attention-deficit/hyperactivity disorder in offspring: a systematic review, meta-analysis and
quasi-experimental family-based study. _Int. J. Epidemiol._ 49, 857–875 (2020). Article PubMed PubMed Central Google Scholar * Marley, A. R., Domingues, A., Ghosh, T., Turcotte, L. M.
& Spector, L. G. Maternal body mass index, diabetes, and gestational weight gain and risk for pediatric cancer in offspring: a systematic review and meta-analysis. _JNCI Cancer Spectr._
6, pkac020 (2022). Article PubMed PubMed Central Google Scholar * Masson, W. et al. Association between maternal epicardial adipose tissue, gestational diabetes mellitus, and
pregnancy-related hypertensive disorders: a systematic review and meta-analysis. _Arch. Gynecol. Obstet._ 308, 1057–1066 (2023). Article PubMed Google Scholar * Miao, J. et al. Maternal
body mass index, gestational weight gain, and risk of cancer in offspring: a systematic review and meta-analysis. _Nutrients_ 15, 1601 (2023). Article PubMed PubMed Central Google Scholar
* Molyneaux, E., Poston, L., Ashurst-Williams, S. & Howard, L. M. Obesity and mental disorders during pregnancy and postpartum: a systematic review and meta-analysis. _Obstet.
Gynecol._ 123, 857–867 (2014). Article PubMed PubMed Central Google Scholar * Ng, K. Y. B. et al. Systematic review and meta-analysis of female lifestyle factors and risk of recurrent
pregnancy loss. _Sci. Rep._ 11, 7081 (2021). Article CAS PubMed PubMed Central Google Scholar * Yu, Z. et al. Pre-pregnancy body mass index in relation to infant birth weight and
offspring overweight/obesity: a systematic review and meta-analysis. _PLoS ONE_ 8, e61627 (2013). Article CAS PubMed PubMed Central Google Scholar * Putra, I. C. S., Irianto, C. B.,
Raffaello, W. M., Suciadi, L. P. & Prameswari, H. S. Pre-pregnancy obesity and the risk of peripartum cardiomyopathy: a systematic review and meta-analysis. _Indian Heart J._ 74, 235–238
(2022). Article PubMed PubMed Central Google Scholar * Rahnemaei, F. A. et al. Association of body composition in early pregnancy with gestational diabetes mellitus: a meta-analysis.
_PLoS ONE_ 17, e0271068 (2022). Article CAS PubMed PubMed Central Google Scholar * Stockman, J. A. Maternal overweight and obesity and the risk of congenital anomalies: a systematic
review and meta-analysis. _Yearb. Pediatr._ 2010, 451–453 (2010). Article Google Scholar * Uyl, N., De Jonge, E., Uyl-de Groot, C., Van Der Marel, C. & Duvekot, J. Difficult epidural
placement in obese and non-obese pregnant women: a systematic review and meta-analysis. _Int. J. Obstet. Anesthesia_ 40, 52–61 (2019). Article CAS Google Scholar * Vats, H., Saxena, R.,
Sachdeva, M. P., Walia, G. K. & Gupta, V. Impact of maternal pre-pregnancy body mass index on maternal, fetal and neonatal adverse outcomes in the worldwide populations: a systematic
review and meta-analysis. _Obes. Res. Clin. Pract._ 15, 536–545 (2021). Article PubMed Google Scholar * Vena, F. et al. Risk of neural tube defects according to maternal body mass index:
a systematic review and meta-analysis. _J. Matern.-Fetal Neonatal Med._ 35, 7296–7305 (2022). Article PubMed Google Scholar * Wu, L., Li, N. & Liu, Y. Association between maternal
factors and risk of congenital heart disease in offspring: a systematic review and meta-analysis. _Matern. Child Health J._ 27, 29–48 (2023). Article PubMed Google Scholar * Xiao, D. et
al. Association between maternal overweight or obesity and cerebral palsy in children: a meta-analysis. _PLoS ONE_ 13, e0205733 (2018). Article PubMed PubMed Central Google Scholar *
Yao, D. et al. Relationship between maternal central obesity and the risk of gestational diabetes mellitus: a systematic review and meta-analysis of cohort studies. _J. Diabetes Res._ 2020,
6303820 (2020). Article PubMed PubMed Central Google Scholar * Zhang, L. et al. Maternal gestational smoking, diabetes, alcohol drinking, pre-pregnancy obesity and the risk of
cryptorchidism: a systematic review and meta-analysis of observational studies. _PLoS ONE_ 10, e0119006 (2015). Article PubMed PubMed Central Google Scholar * Zhang, C., Wu, Y., Li, S.
& Zhang, D. Maternal prepregnancy obesity and the risk of shoulder dystocia: a meta-analysis. _BJOG_ 125, 407–413 (2018). Article CAS PubMed Google Scholar * Zhang, S., Lin, T.,
Zhang, Y., Liu, X. & Huang, H. Effects of parental overweight and obesity on offspring’s mental health: a meta-analysis of observational studies. _PLoS ONE_ 17, e0276469 (2022). Article
CAS PubMed PubMed Central Google Scholar * Zheng, Z. et al. Increased maternal body mass index is associated with congenital heart defects: an updated meta-analysis of observational
studies. _Int. J. Cardiol._ 273, 112–120 (2018). Article PubMed Google Scholar * Zhou, J. et al. Maternal pre-pregnancy body mass index, gestational weight gain, and pubertal timing in
daughters: a systematic review and meta-analysis of cohort studies. _Obes. Rev._ 23, e13418 (2022). Article PubMed Google Scholar * Zhu, T., Tang, J., Zhao, F., Qu, Y. & Mu, D.
Association between maternal obesity and offspring Apgar score or cord pH: a systematic review and meta-analysis. _Sci. Rep._ 5, 18386 (2015). Article CAS PubMed PubMed Central Google
Scholar * Zhu, S.-M., He, Y.-C., Zhang, C., Wu, Y.-T. & Huang, H.-F. Associations of prepregnancy body mass index, gestational weight gain, and intelligence in offspring: a systematic
review and meta-analysis. _Reprod. Dev. Med._ 5, 247–256 (2021). Article Google Scholar * Sterne, J. A. C. et al. Recommendations for examining and interpreting funnel plot asymmetry in
meta-analyses of randomised controlled trials. _Brit. Med. J._ 343, d4002 (2011). Article PubMed Google Scholar * Taylor, K. et al. The effect of maternal BMI, smoking and alcohol on
congenital heart diseases: a Mendelian randomisation study. _BMC Med._ 21, 35 (2023). Article PubMed PubMed Central Google Scholar * Xiao, B. et al. Inference of causal relationships
between genetic risk factors for cardiometabolic phenotypes and female-specific health conditions. _JAHA_ 12, e026561 (2023). Article PubMed PubMed Central Google Scholar * Geng, T.-T.
& Huang, T. Maternal central obesity and birth size: a Mendelian randomization analysis. _Lipids Health Dis._ 17, 181 (2018). Article PubMed PubMed Central Google Scholar * Song, X.,
Wang, C., Wang, T., Zhang, S. & Qin, J. Obesity and risk of gestational diabetes mellitus: a two-sample Mendelian randomization study. _Diabetes Res. Clin. Pract._ 197, 110561 (2023).
Article PubMed Google Scholar * Richmond, R. C. et al. Using genetic variation to explore the causal effect of maternal pregnancy adiposity on future offspring adiposity: a Mendelian
randomisation study. _PLoS Med._ 14, e1002221 (2017). Article PubMed PubMed Central Google Scholar * Venkatesh, S. S. et al. Obesity and risk of female reproductive conditions: a
Mendelian randomisation study. _PLoS Med._ 19, e1003679 (2022). Article PubMed PubMed Central Google Scholar * Ardissino, M. et al. Maternal hypertension increases risk of preeclampsia
and low fetal birthweight: genetic evidence from a Mendelian randomization study. _Hypertension_ 79, 588–598 (2022). Article CAS PubMed Google Scholar * Kim, M. S. et al. Association
between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies. _Eur. Heart J._ 42, 3388–3403 (2021). Article
PubMed PubMed Central Google Scholar * Kyrgiou, M. et al. Adiposity and cancer at major anatomical sites: umbrella review of the literature. _BMJ_ https://doi.org/10.1136/bmj.j477 (2017).
* Tsiros, M. D. et al. Obesity, the new childhood disability? An umbrella review on the association between adiposity and physical function. _Obes. Rev._ 21, e13121 (2020). Article PubMed
Google Scholar * Pulit, S. L. et al. Meta-analysis of genome-wide association studies for body fat distribution in 694 649 individuals of European ancestry. _Hum. Mol. Genet._ 28, 166–174
(2019). Article CAS PubMed Google Scholar * Bray, G. A. et al. Relation of central adiposity and body mass index to the development of diabetes in the Diabetes Prevention Program. _Am.
J. Clin. Nutr._ 87, 1212–1218 (2008). Article CAS PubMed Google Scholar * Muhlhausler, B. S. & Ong, Z. Y. The fetal origins of obesity: early origins of altered food intake. _EMIDDT_
11, 189–197 (2011). Article CAS Google Scholar * Yu, Z. B. et al. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. _Obes. Rev._ 12, 525–542 (2011).
Article CAS PubMed Google Scholar * Tsur, A., Sergienko, R., Wiznitzer, A., Zlotnik, A. & Sheiner, E. Critical analysis of risk factors for shoulder dystocia. _Arch. Gynecol.
Obstet._ 285, 1225–1229 (2012). Article PubMed Google Scholar * Araujo Júnior, E., Peixoto, A. B., Zamarian, A. C. P., Elito Júnior, J. & Tonni, G. Macrosomia. _Best Pract. Res. Clin.
Obstet. Gynaecol._ 38, 83–96 (2017). Article PubMed Google Scholar * Tanvig, M. et al. Anthropometrics and body composition by dual energy X-ray in children of obese women: a follow-up
of a randomized controlled trial (the Lifestyle in Pregnancy and Offspring [LiPO] Study). _PLoS ONE_ 9, e89590 (2014). Article PubMed PubMed Central Google Scholar * Castillo, H.,
Santos, I. S. & Matijasevich, A. Relationship between maternal pre-pregnancy body mass index, gestational weight gain and childhood fatness at 6–7 years by air displacement
plethysmography. _Matern. Child Nutr._ 11, 606–617 (2015). Article PubMed PubMed Central Google Scholar * Chen, Q. et al. Maternal pre-pregnancy body mass index and offspring attention
deficit hyperactivity disorder: a population-based cohort study using a sibling-comparison design. _Int. J. Epidemiol._ 43, 83–90 (2014). Article CAS PubMed Google Scholar * Musser, E.
D. et al. Maternal prepregnancy body mass index and offspring attention-deficit/hyperactivity disorder: a quasi-experimental sibling-comparison, population-based design. _J. Child Psychol.
Psychiatry_ 58, 240–247 (2017). Article PubMed Google Scholar * Huang, L. et al. Maternal prepregnancy obesity and child neurodevelopment in the Collaborative Perinatal Project. _Int. J.
Epidemiol._ 43, 783–792 (2014). Article PubMed Google Scholar * Gardner, R. M. et al. Maternal body mass index during early pregnancy, gestational weight gain, and risk of autism spectrum
disorders: results from a Swedish total population and discordant sibling study. _Int. J. Epidemiol._ 44, 870–883 (2015). Article PubMed PubMed Central Google Scholar * Taylor, K. et
al. Effect of maternal prepregnancy/early-pregnancy body mass index and pregnancy smoking and alcohol on congenital heart diseases: a parental negative control study. _JAHA_ 10, e020051
(2021). Article PubMed PubMed Central Google Scholar * Liu, X. et al. Maternal body mass index and risk of congenital heart defects in infants: a dose-response meta-analysis. _BioMed
Res. Int._ 2019, 1–14 (2019). Google Scholar * Persson, M., Razaz, N., Edstedt Bonamy, A.-K., Villamor, E. & Cnattingius, S. Maternal overweight and obesity and risk of congenital heart
defects. _J. Am. Coll. Cardiol._ 73, 44–53 (2019). Article PubMed Google Scholar * Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews.
_BMJ_ https://doi.org/10.1136/bmj.n71 (2021). * Smith, V., Devane, D., Begley, C. M. & Clarke, M. Methodology in conducting a systematic review of systematic reviews of healthcare
interventions. _BMC Med. Res. Methodol._ 11, 15 (2011). Article PubMed PubMed Central Google Scholar * Song, J. W. & Chung, K. C. Observational studies: cohort and case-control
studies. _Plast. Reconstr. Surg._ 126, 2234–2242 (2010). Article CAS PubMed PubMed Central Google Scholar * Mann, C. J. Observational research methods. Research design II: cohort, cross
sectional, and case-control studies. _Emerg. Med. J._ 20, 54–60 (2003). Article CAS PubMed PubMed Central Google Scholar * Egger, M., Smith, G. D., Schneider, M. & Minder, C. Bias
in meta-analysis detected by a simple, graphical test. _Brit. Med. J._ 315, 629–634 (1997). Article CAS PubMed PubMed Central Google Scholar * Higgins, J. P. T., Thompson, S. G. &
Spiegelhalter, D. J. A re-evaluation of random-effects meta-analysis. _J. R. Stat. Soc. Ser. A Stat. Soc._ 172, 137–159 (2009). Article PubMed PubMed Central Google Scholar * Salanti, G.
& Ioannidis, J. P. A. Synthesis of observational studies should consider credibility ceilings. _J. Clin. Epidemiol._ 62, 115–122 (2009). Article PubMed Google Scholar *
Papatheodorou, S. I., Tsilidis, K. K., Evangelou, E. & Ioannidis, J. P. A. Application of credibility ceilings probes the robustness of meta-analyses of biomarkers and cancer risk. _J.
Clin. Epidemiol._ 68, 163–174 (2015). Article PubMed Google Scholar * Ioannidis, J. P. & Trikalinos, T. A. An exploratory test for an excess of significant findings. _Clin. Trials_ 4,
245–253 (2007). Article PubMed Google Scholar * Viechtbauer, W. Conducting meta-analyses in R with the metafor package. _J. Stat. Soft._ 36, 1–48 (2010). Article Google Scholar *
Balduzzi, S., Rücker, G. & Schwarzer, G. How to perform a meta-analysis with R: a practical tutorial. _Evid. Based Ment. Health_ 22, 153–160 (2019). Article PubMed PubMed Central
Google Scholar * Shea, B. J. et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. _BMJ_
https://doi.org/10.1136/bmj.j4008 (2017). * Larsson, S. C. & Burgess, S. Causal role of high body mass index in multiple chronic diseases: a systematic review and meta-analysis of
Mendelian randomization studies. _BMC Med._ 19, 320 (2021). Article PubMed PubMed Central Google Scholar * Skrivankova, V. W. et al. Strengthening the reporting of observational studies
in epidemiology using Mendelian randomization: the STROBE-MR statement. _JAMA_ 326, 1614–1621 (2021). Article PubMed Google Scholar * Belbasis, L., Bellou, V., Evangelou, E., Ioannidis,
J. P. A. & Tzoulaki, I. Environmental risk factors and multiple sclerosis: an umbrella review of systematic reviews and meta-analyses. _Lancet Neurol._ 14, 263–273 (2015). Article
PubMed Google Scholar * Bellou, V. et al. Systematic evaluation of the associations between environmental risk factors and dementia: an umbrella review of systematic reviews and
meta-analyses. _Alzheimers_ _Dement._ 13, 406–418 (2017). Article Google Scholar * Kim, J. Y. et al. Environmental risk factors and biomarkers for autism spectrum disorder: an umbrella
review of the evidence. _Lancet Psychiatry_ 6, 590–600 (2019). Article PubMed Google Scholar * Kim, J. H. et al. Environmental risk factors, protective factors, and peripheral biomarkers
for ADHD: an umbrella review. _Lancet Psychiatry_ 7, 955–970 (2020). Article PubMed Google Scholar * Markozannes, G. et al. Systematic review of Mendelian randomization studies on risk of
cancer. _BMC Med._ 20, 41 (2022). Article PubMed PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS This study was supported by the National Key Research and Development
Program of China (2021YFC2700400 (H.Z.) and 2021YFC2700701 (S.Z.)), the Basic Science Center Program of NSFC (31988101) (Z.-J.C.), the National Natural Science Foundation of China (32370916
(S.Z.), 82071606 (S.Z.), 82101707 (X.G.) and 82192874 (H.Z.)), the CAMS Innovation Fund for Medical Sciences (2021-I2M-5-001) (Z.-J.C.), the Shandong Provincial Key Research and Development
Program (2020ZLYS02) (Z.-J.C.), the Natural Science Foundation of Shandong Province for Excellent Youth Scholars (ZR2023YQ061) (S.Z.), the Program for Chang Jiang Scholars (Q2022144)
(S.Z.), the Taishan Scholars Program of Shandong Province (ts20190988) (H.Z.), the Innovative Research Team of High-level Local Universities in Shanghai (SHSMU-ZLCX20210200) (Z.-J.C.) and
the Fundamental Research Funds of Shandong University (2023QNTD004) (S.Z.). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the
paper. AUTHOR INFORMATION Author notes * These authors contributed equally: Ziyi Yang, Gengchen Feng, Xueying Gao. AUTHORS AND AFFILIATIONS * State Key Laboratory of Reproductive Medicine
and Offspring Health, Center for Reproductive Medicine, Institute of Women, Children and Reproductive Health, Shandong University, Jinan, China Ziyi Yang, Gengchen Feng, Xueqi Yan, Yimeng
Li, Yuteng Wang, Yonghui Jiang, Shigang Zhao, Han Zhao & Zi-Jiang Chen * National Research Center for Assisted Reproductive Technology and Reproductive Genetics, Shandong University,
Jinan, China Xueying Gao, Shumin Li, Shigang Zhao, Han Zhao & Zi-Jiang Chen * Department of Reproductive Medicine, Ren Ji Hospital, Shanghai Jiao Tong University School of Medicine,
Shanghai, China Xueying Gao, Shumin Li & Zi-Jiang Chen * Shanghai Key Laboratory for Assisted Reproduction and Reproductive Genetics, Shanghai, China Xueying Gao, Shumin Li &
Zi-Jiang Chen * Key Laboratory of Reproductive Endocrinology (Shandong University), Ministry of Education, Jinan, China Shigang Zhao, Han Zhao & Zi-Jiang Chen * Shandong Technology
Innovation Center for Reproductive Health, Jinan, China Shigang Zhao, Han Zhao & Zi-Jiang Chen * Shandong Provincial Clinical Research Center for Reproductive Health, Jinan, China
Shigang Zhao, Han Zhao & Zi-Jiang Chen * Shandong Key Laboratory of Reproductive Medicine, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
Shigang Zhao, Han Zhao & Zi-Jiang Chen * Research Unit of Gametogenesis and Health of ART-Offspring, Chinese Academy of Medical Sciences, Jinan, China Shigang Zhao, Han Zhao &
Zi-Jiang Chen Authors * Ziyi Yang View author publications You can also search for this author inPubMed Google Scholar * Gengchen Feng View author publications You can also search for this
author inPubMed Google Scholar * Xueying Gao View author publications You can also search for this author inPubMed Google Scholar * Xueqi Yan View author publications You can also search for
this author inPubMed Google Scholar * Yimeng Li View author publications You can also search for this author inPubMed Google Scholar * Yuteng Wang View author publications You can also
search for this author inPubMed Google Scholar * Shumin Li View author publications You can also search for this author inPubMed Google Scholar * Yonghui Jiang View author publications You
can also search for this author inPubMed Google Scholar * Shigang Zhao View author publications You can also search for this author inPubMed Google Scholar * Han Zhao View author
publications You can also search for this author inPubMed Google Scholar * Zi-Jiang Chen View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS
Z.Y., S.Z., H.Z. and Z.-J.C. were involved in the original conceptualization. Z.Y., G.F., X.G., S.Z., H.Z. and Z.-J.C. were responsible for developing the study methodology. Z.Y., G.F. and
X.G. did the literature search. Z.Y., G.F., X.G., X.Y., Y.L., Y.W., Y.J. and S.L. were responsible for data curation. Z.Y., G.F. and X.G. did the formal statistical analysis. Z.Y., G.F. and
X.G. wrote the original draft. All authors edited and reviewed the paper. CORRESPONDING AUTHORS Correspondence to Shigang Zhao, Han Zhao or Zi-Jiang Chen. ETHICS DECLARATIONS COMPETING
INTERESTS The authors declare no competing interests. PEER REVIEW PEER REVIEW INFORMATION _Nature Human Behaviour_ thanks Ilkka Kalliala, Mai-Lei Woo Kinshella and the other, anonymous,
reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard
to jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION Supplementary Tables 1–16, Appendices 1–3 and PRIOR checklist.
REPORTING SUMMARY PEER REVIEW FILE RIGHTS AND PERMISSIONS Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing
agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement
and applicable law. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Yang, Z., Feng, G., Gao, X. _et al._ Maternal adiposity and perinatal and offspring outcomes: an umbrella
review. _Nat Hum Behav_ 8, 2406–2422 (2024). https://doi.org/10.1038/s41562-024-01994-6 Download citation * Received: 25 March 2024 * Accepted: 30 August 2024 * Published: 11 October 2024 *
Issue Date: December 2024 * DOI: https://doi.org/10.1038/s41562-024-01994-6 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link
Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative







