- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
Autoreactive B cells have a major function in autoimmunity. A small subset of B cells expressing two distinct B-cell-antigen-receptors (B2R cells) is elevated in many patients with
systematic lupus erythematosus (SLE) and in the MRL(/lpr) mouse model of lupus, and is often autoreactive. Here we show, using RNAseq and in vitro and in vivo analyses, signals that are
required for promoting B2R cell numbers and effector function in autoimmune mice. Compared with conventional B cells, B2R cells are more responsive to Toll-like receptor 7/9 and type I/II
interferon treatment, display higher levels of MHCII and co-receptors, and depend on IL-21 for their homeostasis; moreover they expand better upon T cell-dependent antigen stimulation, and
mount a more robust memory response, which are characteristics essential for enhanced (auto)immune responses. Our findings thus provide insights on the stimuli for the expansion of an
autoreactive B cell subset that may contribute to the etiology of SLE.
A hallmark of systemic lupus erythematosus (SLE) is a breach in B cell tolerance that results in the production of autoantibodies. Autoantibody-producing B cells play additional pathogenic
roles in the progression of SLE by secreting inflammatory cytokines and directly activating pathogenic T cells1,2,3. Autoreactive B cells originate from the bone marrow via expression of
newly rearranged germline immunoglobulin (Ig) genes but also arise from peripheral lymphoid tissue subsequent to the somatic hypermutation of Ig genes. During the development of B cells in
the bone marrow, random Ig gene rearrangements generate a large number of autoreactive B cells4,5. However, at least half of these cells are immediately eliminated by receptor editing (i.e.,
secondary Ig gene recombination) or clonal deletion6,7,8. Receptor editing most often results in the elimination of the autoreactive specificity displayed by the B cell antigen receptor
(BCR) and the expression of a new nonautoreactive BCR. However, receptor editing can also lead to the generation of dual-reactive (B2R) B cells: B cells co-expressing two different heavy (H)
or light (L, κ or λ) Ig chains9 and, thus, two different BCRs. These BCRs are comprised of the initial autoreactive antigen receptor and a new nonautoreactive receptor most often based on
the association of the original H chain with a new L chain. B2R cells have a demonstrated ability to bypass tolerance checkpoints and escape to the periphery where they are more or less
regulated by mechanisms of peripheral tolerance, depending on the genetic background and the level of autoreactivity of the B cell clone10,11,12,13,14,15,16. Elegant recent studies indicate
that many of the B cells that participate in disease flares in lupus patients are naive B cells with germline Igs17 and they are therefore generated from de novo B cell development, as
opposed to arising from a germinal center (GC) reaction. Thus, the establishment of central (bone marrow) B cell tolerance is of vital importance for the prevention and/or control of
autoimmunity in humans.
B2R cells are observed in both healthy mice and humans at a frequency of less than 3% of all B cells14,18,19,20,21,22. Our previous findings have shown that the fate of B2R cells can be
different in an autoimmune background; here these cells expand with disease and show high level of activation23. To study B2R cells we have employed the use of congenic mice bearing a gene
targeted human Ig Cκ allele24 on a healthy (CB17) or an autoimmune (MRL) genetic background23. These Igkm/h mice allow for the detection of B cells co-expressing two different κ chains
(dual-κ) within a wild-type Ig repertoire. We have previously found that dual-κ B cells accumulate in both MRL and MRL/lpr mice with age, while this is not observed in the non-autoimmune
CB17 mice23. Furthermore, dual-κ B cell enrichment in MRL(/lpr) mice correlates with disease progression and with the appearance of autoantibodies. These B2R cells are particularly enriched
in the effector plasmablast and IgG+ memory B cell compartments of MRL(/lpr) mice, where they represent up to 50% of cells in older mice. Overall, dual-κ B cells are more autoreactive,
express higher levels of activation markers, and secrete larger amounts of autoantibodies than single-κ B cells23. Interestingly, dual-κ B cells do not display these characteristics in
NZB/NZW lupus mice25 and, thus, their association with lupus-like disease is likely dependent on genetic polymorphisms. Similar to what has been described in lupus mice, a recent study found
that B2R cells co-expressing κ and λ, are expanded in a subset (about 40%) of SLE patients26. This suggests B2R cells are a significant player of SLE pathogenesis and that, gaining a better
understanding of their biology, is important.
In this study we exploited our dual-κ autoimmune mouse model (MRL/lpr-Igkm/h) to identify molecular pathways that can drive the accumulation and activation of B2R cells in murine lupus. We
show that a significant difference exists between single and dual-κ B cells both functionally and at the transcriptome level. Overall, our data indicate that both T cell-mediated signals and
innate stimuli, together and independently, play a role in the enrichment, activation, and differentiation of dual-κ B cells during lupus-like disease in MRL/lpr mice.
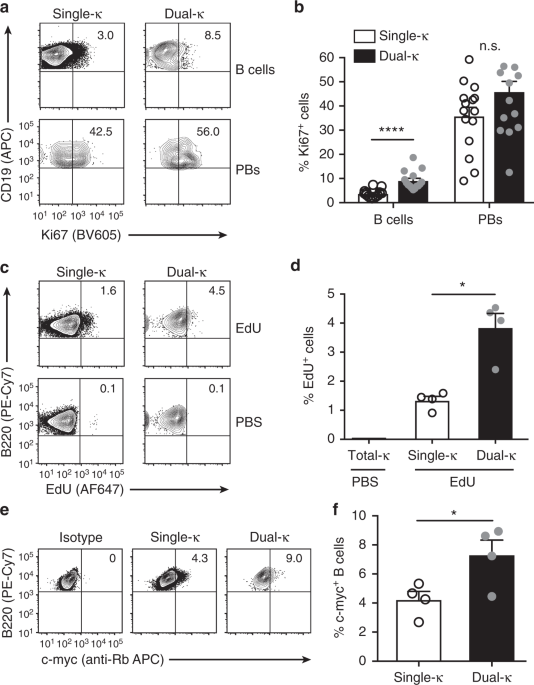
We have previously shown that dual-κ B cells from MRL and MRL/lpr lupus mice are enriched in the plasmablast cell compartment23, which is a stage at which cells are actively proliferating.
To evaluate whether this plasmablast enrichment is due to an increased proliferative ability of dual-κ relative to single-κ B cells, we analyzed the expression of the proliferation marker
Ki67 and the frequency of EdU incorporation, as readouts for active cell division. The frequency of Ki67+ dual-κ CD138– B cells was 2–3-fold greater than that of single-κ cells in the spleen
of naive MRL/lpr-Igkm/h mice, while it was similar in the CD138+ plasmablast compartment (Fig. 1a, b and Supplementary Fig. 1a, b). Furthermore, 24 h after the injection of EdU, the
frequency of EdU+ dual-κ splenic B cells was 3-fold higher than that of single-κ B cells (Fig. 1c, d and Supplementary Fig. 1a–c), thus indicating enhanced active proliferation of dual-κ B
cells in vivo.
Splenic dual-κ B cells display higher proliferation rates than single-κ B cells. a Representative flow cytometric contour plots showing frequency of Ki67+ single and dual-κ cells within
B220+CD19+ CD138– B cells (top) and CD138+CD44high plasmablasts (PBs, bottom), gated as shown in Fig. S1a, b. b Mean frequency of Ki67+ cells within single (white bar) or dual-κ (black bar)
B cells and PBs described in a. Data are combined from three independent experiments using 9–16-wk-old MRL/lpr-Igkm/h mice (N = 15 total). c Representative contour plots showing the
frequency of EdU+ single and dual-κ cells within CD3–B220+ B cells (gated as in Supplementary Fig. 1a–c) 24 h after either EdU (top row) or PBS (bottom row) injection in MRL/lpr-Igkm/h mice.
d Mean frequency of EdU incorporation by splenic single-κ (white bar) or dual-κ (black bar) B cells (gated as described in c), after EdU injection in 12–14-wk-old MRL/lpr-Igkm/h mice. Data
from one untreated MRL/lpr-Igkm/h mouse indicate EdU background staining in total Igκ+ B cells. Representative data from one out of three experiments is shown with N = 4 in each experiment.
e Representative flow cytometric analysis to measure the frequency of c-Myc-positive cells within splenic CD3–B220+ single-κ (middle panel) or dual-κ B cells (far right panel), gated as
shown in Supplementary Fig. 1a–d. Far left panel shows Igκ+ B cells stained with an isotype control. f Mean frequency of c-Myc+ cells within single or dual-κ B cell subsets described in e in
13-wk-old MRL/lpr-Igkm/h mice. N = 4 from one experiment. *P 4.53) were role of pattern recognition receptors in recognition of bacteria and viruses, complement system, IL-6 signaling, and
toll-like receptor signaling. Thus, while there was overlap in the RNAseq data from FO and MZ B cells, there were also some distinctions.
Results from these gene expression analyses suggest dual-κ B cells from MRL/lpr mice possess a differential ability to respond to T cell-dependent and independent signals relative to
single-κ B cells.
The TLR and IFN I and II pathways are of particular relevance for the onset and progression of lupus disease2,30,31. Based on the RNAseq analysis, dual-κ FO B cells displayed differential
expression of 21 out of 76 genes and 14 out of 36 genes in the TLR signaling and the interferon signaling pathways, respectively (Fig. 3a). To validate these results, we investigated in
vitro responses of single and dual-κ B cells to these innate stimuli.
Innate stimuli expand and activate dual-κ B cells. a Relative expression of genes in dual-κ and single-κ FO B cells in the Toll-like Receptor (TLR, left; differential expression of 21 out of
76 genes) or Interferon (IFN, right; differential expression of 14 out of 36 genes) signaling pathways identified in the RNAseq data described in Fig. 2 (FDR ≤ 0.1). The heat maps colors
are explained in Fig. 2a. Data are from three independent biological replicates analyzed in one experiment. b, c Mean frequency of dual-κ B cells (b) and fold change of CD69 expression (MFI)
on dual-κ relative to single-κ cells (c) within CD43– B cells cultured for 48 h in media or with CpG for TLR9, R848 for TLR7, LPS for TLR4. Gating strategy for this analysis and subtraction
of background events are described in Supplementary Fig. 3a, b. Data are combined from two independent experiments using 14–15-wk-old MRL/lpr-Igkm/h mice (N = 7 total). Data in c are not
significant. d, e Untouched (CD43–) B cells were stimulated for 24 h with IFNα or IFNγ. Bar graphs show MFI of CD69 on dual-κ cells as a fold change relative to amounts on single-κ cells
(d), or the mean frequency of dual-κ B cells (e), within the CD19+Igκ+ cell population gated as in Supplementary Fig. 3a. Data are combined from two independent experiments (N = 6 total)
using 12-wk-old MRL/lpr-Igkm/h mice. f, g Untouched naive B cells (magnetic selection of CD43–CD80–CD86– cells, Supplementary Fig. 4c) were stimulated for 48 h with CpG, R848, or IFNα. Shown
are the mean frequencies of dual-κ B cells (f) or the MFI of CD69 (g) within the CD19+Igκ+ cells gated as in Supplementary Fig. 3a. Data were obtained using 12-wk-old MRL/lpr-Igkm/h mice (N
= 4) in one experiment. In panels (c, d–g), the CD69 MFI values of cells cultured in media were subtracted from those in stimulated samples. *P






.jpg?rect=0%2C0%2C1778%2C933)


