- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
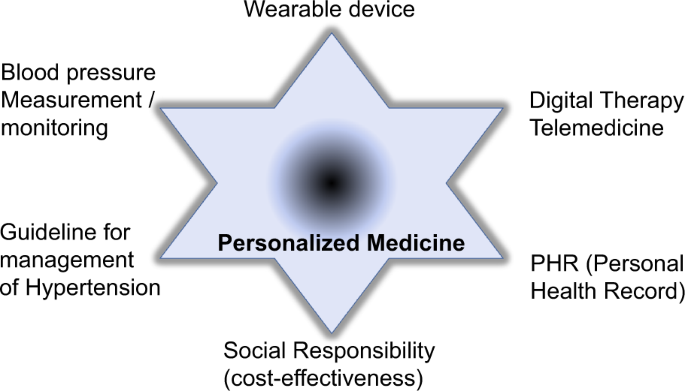
Digital hypertension management is defined as a new information and communication technology-based research field in digital health care [1]. This includes not only the utilization of
wearable devices, telemedicine, and personal health records (PHRs) but also contributions to develop blood pressure (BP) monitoring and guide the management of hypertension (Fig. 1). The
popularization of digital platforms, such as smartphone applications, accelerates the accumulation of PHRs by self-measurements of body weight, physical activity, and pulse rate. In
addition, during periods of infectious disease pandemics, PHRs can be increasingly utilized in medical care, and telemedicine can be recommended to reduce human contact worldwide. A new wave
of exponential progression in digital health is coming to the health care field, including sensor technology (i.e., continuous blood sugar measurements) and therapeutic devices (i.e.,
portable electrocardiograms). In terms of the field of hypertension, several cuff-less BP monitoring devices are also available on the market; however, most of them are not recommended for
clinical use due to their limited accuracy for BP measurements. BP shows beat-by-beat variations, orthostatic variations, and diurnal variations in the short term and intervisit variations,
seasonal variations, and secular variations in the long term. Ambulatory BP monitoring at predetermined intervals can detect variations, and early morning, midday, and nocturnal hypertension
have been noted as masked hypertension, which can occur even when office BP is under control. However, when factors such as mental stress, physical activity, smoking, and sleep disturbances
occur during these hours, BP rises further, leading to events such as plaque disruption and bleeding [2]. Recently, the wristwatch-type oscillometric device was developed with defined
validation, which can allow us to monitor BP by self-measurement. Tomitani et al. utilized a wearable watch-type blood pressure monitor to measure BP under different conditions, such as
different emotions, different locations, and stress-induced BP elevation [3]. There was a significant increase in systolic BP (SBP) when a participant’s BP was measured at a time when they
reported feeling angry, tense, anxious or sad (9.8, 4.6, 4.2, and 11.1 mmHg, respectively), and a significant decrease was observed when they reported feeling calm (−2.4 mmHg). Regarding the
degree of stress as a variable, SBP measurements under moderate and high stress conditions were higher than those measured under nonstress conditions (6.8 and 13.1 mmHg, respectively). The
increase in BP due to emotional factors and the intensity of stress was larger than that due to location (worksite measurement of 3.2 mmHg). In another study using the same wearable BP
monitor, a 7.9 mmHg increase was also found while participants were experiencing negative emotions (anxiety, tension) compared to positive emotions (happiness, calm); a 4.6 mmHg increase was
found while participants were at work compared to home; and a 4.5 mmHg increase was found while participants were performing moderate or intense exercise compared to being at rest [4]. Of
importance, it has already been reported that the peak value of BP measurements recorded using a wearable daytime BP monitor was correlated with the left ventricular mass index [5], which
suggests that increases in self-measured BP recorded using a wearable BP monitor are a risk factor for cardiovascular diseases. Thus, to prevent BP surges that can trigger cardiovascular
disease, psychological stress or emotional stress should be considered, especially for patients at high risk of cardiovascular diseases. BP might be affected by various stressors, including
the thermal environment as well as mental stress or emotional status. BP quickly increases at cold temperatures because blood vessels constrict to suppress heat dissipation to maintain a
constant core body temperature. Although rapid BP increases at cold temperatures cannot be detected in real time, self-measurements of BP will allow us to evaluate BP changes in thermal
environments and know the suitable indoor temperature for BP management. The WHO Housing and Health Guidelines recommend a minimum indoor temperature of 18 °C to prevent cold-related
diseases [6]. In a recent cross-sectional analysis in Japan, the average temperature in living rooms and bedrooms was 16.8 °C and 12.8 °C, respectively [7]. In contrast, in homes in the UK,
the average living room and bedroom temperatures in winter were 19.3 °C and 18.9 °C, respectively [8]. We should pay more attention to the thermal environment at home, and self-measurements
of BP will assist in determining individual comfortable environments. It may also contribute to preventing BP surges to prevent cardiovascular events in high-risk patients. The last piece of
the digital hypertension management concept is to evaluate its cost-effectiveness in the field of hypertension management. In clinical studies, the efficacy and safety of novel therapies
are usually evaluated as endpoints. However, cost-effectiveness will also be important to effectively allocate medical resources in the real world. Nomura et al. analyzed the
cost-effectiveness of prescription digital therapeutics (DTx) [9]. To assess the cost-effectiveness of essential hypertension, they developed an economic model using quality-adjusted
life-years (QALYs) and compared the cost of DTx plus guideline-based lifestyle modification consultation treatment as usual (TAU) with TAU alone with a lifetime horizon based on their phase
3 clinical trial, the HERB-DH1 pivotal trial [10]. Of importance, in the incremental cost-effective ratio per QALY (the benchmark for cost-effectiveness), the monthly cost and attribution
rate of DTx had a significant impact on hypertension. The DTx+TAU strategy was more cost-effective than the TAU-only strategy. Although the economic model to evaluate cost-effectiveness
might be different for each disease, a few approaches have been reported for patients with hypertension [11, 12] and for patients with other diseases [13,14,15]. DTx for opioid use disorder
and for low back pain were cost-effective in a relatively short time horizon (12 weeks to 3 years). In contrast, Nomura et al. showed that the benefit of the BP-lowering effect persisted for
more than 3 years, resulting in the prevention of CVD, left ventricular hypertrophy, vascular events, heart failure, etc. Thus, in the evaluation of cost-effectiveness for lifestyle-related
diseases, a long-term analysis would be valuable in considering the practical effect of DTx. In the future, a subanalysis of cost-effectiveness might need to be analyzed based on RCTs for
hypertension or other diseases, which would help in identifying better therapy for patients and help society from the perspective of medical expenses. The Japanese Society of Hypertension
(JSH) proposed that digital hypertension management is a new science that includes the development of new technologies such as sensors, information processing and machine learning. The
exponential progression of digital health will encourage significant developments in the approach to hypertension. Future medicine might integrate a multidimensional time series for each
individual to prevent cardiovascular events by effective intervention, leading to personalized medicine (Fig. 1). REFERENCES * Kario K, Harada N, Okura A. State-of-the-art rapid review of
the current landscape of digital hypertension. Conn Health. 2022;1:46–58. Google Scholar * Kario K. Management of hypertension in the digital era: small wearable monitoring devices for
remote blood pressure monitoring. Hypertension. 2020;76:640–50. Article CAS Google Scholar * Tomitani N, Kanegae H, Kario K. Self-monitoring of psychological stress-induced blood pressure
in daily life with a wearable watch-type oscillometric device in working hypertensives. Hypertens Res. 2022. https://doi.org/10.1038/s41440-022-00946-9. Online ahead of print. * Tomintani
N, Kanegae H, Suzuki Y, Kuwabara M, Kario K. Stress-induced blood pressure elevation self-measured by a wearable watch-type device. Am J Hypertens. 2021;34:377–82. Article Google Scholar *
Kario K, Tomitani N, Morimoto T, kanegae H, lacy P, Williams B. Relationship between blood pressure repeatedly measured by a wrist-cuff oscillometric wearable blood pressure monitoring
device and left ventricular mass index in working hypertensive patients. Hypertens Res. 2022;45:87–96. Article Google Scholar * World Health Organization. Housing and health guidelines.
2018. https://apps.who.int/iris/bitst ream/handl e/10665 /27600 1/9789241550 376-eng.pdf. * Umishio W, Ikaga T, Fujino Y, Ando S, Kubo T, Nakajima Y, et al. Disparities of indoor temperature
in winter: a cross-sectional analysis of the Nationwide Smart Wellness Housing Survey in Japan. Indoor Air. 2020;30:1317–28. Article Google Scholar * Building Research Establishment.
Energy Follow-Up Survey 2011: Report 2: Mean household temperatures; BRE report number 283078. 2013.
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/274770/2_Mean_Household_Temperatures.pdf. * Nomura A, Tanigawa T, Kario K, Igarashi A.
Cost-effectiveness of digital therapeutics for essential hypertension. Hypertens Res. 2022. https://doi.org/10.1038/s41440-022-00952-x. Online ahead of print. * Kario K, Nomura A, Harada N,
Okura A, Nakagawa K, Tanigawa T, Hida E. Efficacy of a digital therapeutics system in the management of essential hypertension: the HERB-DH1 pivotal trial. Eur Heart J. 2021;42:4111–22.
Article Google Scholar * Nordyke RJ, Appelbaum K, Berman MA. Estimating the impact of novel digital therapeutics in type 2 diabetes and hypertension: health economic analysis. J Med
Internet Res. 2019;21:e15814. Article Google Scholar * Guthrie NL, Berman MA, Edwards KL, Appelbaum KJ, Dey S, Carpenter J, et al. Achieving rapid blood pressure control with digital
therapeutics: retrospective cohort and machine learning study. JMIR Cardio. 2019;3:e13030. Article Google Scholar * Wang W, Gellings Lowe N, Jalali A, Murphy SM. Economic modeling of
reSET-O, a prescription digital therapeutic for patients with opioid use disorder. J Med Econ. 2021;24:61–68. Article Google Scholar * Velez FF, Malone DC. Cost-effectiveness analysis of a
prescription digital therapeutic for the treatment of opioid use disorder. J Mark Access Health Policy. 2021;9:1966187. Article Google Scholar * Lewkowicz D, Wohlbrandt AM, Bottinger E.
Digital therapeutic care apps with decision-support interventions for people with low back pain in germany: cost-effectiveness analysis. JMIR Mhealth Uhealth. 2022;10:e35042. Article Google
Scholar Download references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Health Development and Medicine, Graduate School of Medicine, Osaka University, 2-2 Yamada-oka,
Suita, Osaka, Japan Hironori Nakagami Authors * Hironori Nakagami View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to
Hironori Nakagami. ETHICS DECLARATIONS CONFLICT OF INTEREST The Department of Health Development and Medicine is an endowed department supported by Anges, Daicel, and FunPep. ADDITIONAL
INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS Reprints and
permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Nakagami, H. New wave of digital hypertension management for clinical applications. _Hypertens Res_ 45, 1549–1551 (2022).
https://doi.org/10.1038/s41440-022-00977-2 Download citation * Received: 19 May 2022 * Revised: 31 May 2022 * Accepted: 05 June 2022 * Published: 20 July 2022 * Issue Date: October 2022 *
DOI: https://doi.org/10.1038/s41440-022-00977-2 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is
not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * Digital Hypertension * BP measurement *
Cost-effectiveness







