- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT In Asian countries, a major source of salt intake is from seasoning or table salt added at home. However, little is known about the adverse effects of salt intake evaluated
according to household unit. We investigated the relationship between household salt intake level and mortality from all-cause and cardiovascular diseases (CVDs). Participants included 8702
individuals (56% women) who were living with someone else and who were aged 30–79 years and enrolled in the National Nutritional Survey of Japan in 1980 with a 24-year follow-up. Household
nutrient intake was evaluated using a 3-day weighing record method in which all foods and beverages consumed by any of the household members were recorded. The household salt intake level
was defined as the amount of salt consumed (g) per 1000 kcal of total energy intake in each household, and its average was 6.25 (2.02) g/1000 kcal. During the follow-up, there were 2360
deaths (787 CVD, 168 coronary heart disease [CHD], and 361 stroke). Cox proportional hazard ratios (HRs) for an increment of 2 g/1000 kcal in household salt intake were calculated and
adjusting for sex, age, body mass index, smoking status, alcohol consumption status, self-reported work exertion level, household potassium intake, household saturated fatty acid intake, and
household long-chain n-3 polyunsaturated fatty acid intake. The HRs (95% confidence intervals) were 1.07 (1.02, 1.12) for all-cause mortality, 1.11 (1.03, 1.19) for CVD, 1.25 (1.08, 1.44)
for CHD, and 1.12 (1.00, 1.25) for stroke. The household salt intake level was significantly associated with long-term risk of all-cause, CVD, CHD, and stroke mortality in a representative
Japanese population. You have full access to this article via your institution. Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS ASSOCIATION BETWEEN SALT INTAKE AND BLOOD PRESSURE AMONG
COMMUNITY-DWELLING OLDER ADULTS BASED ON THEIR PHYSICAL FRAILTY STATUS Article Open access 17 January 2025 ADDING SALT TO FOODS AND HAZARDS OF MICROVASCULAR, CEREBROVASCULAR AND
CARDIOVASCULAR DISEASES Article 14 October 2023 DIETARY PATTERNS AND CARDIOVASCULAR DISEASE RISK AMONG CHINESE ADULTS: A PROSPECTIVE COHORT STUDY Article 06 June 2020 INTRODUCTION Many
studies have clearly shown that excessive salt intake is associated with the elevated blood pressure (BP) [1,2,3] and cardiovascular disease (CVD) risks [4,5,6,7,8,9,10,11], and evidence
from randomized controlled trials has shown that low-salt diets lower BP [5, 12], thereby reducing the risks of CVD and long-term mortality [13]. As such, the World Health Organization
recommends a reduction in salt intake to <5 g/day [14]. However, the average salt intake in most countries remains higher than the recommended level [15]. To reduce salt intake in the
population, the perspective of family members on salt intake might be important because members of the same household often eat similar foods in the home environment. For example, hot pot
dishes are usually cooked at home and are consumed by all household members in Asian countries, including Japan. On the other hand, the main source of salt in western countries is processed
foods [16, 17]. In any case, household members cannot modify the amount of salt that has already been added to a meal. Moreover, salt taste sensitivity develops early in life [18], and salt
taste preference is reported to be acquired via exposure to salty foods [19]. Several studies have reported an association of the salt intake among families [20, 21]. In Japan, salt taste
preference among adults is associated with salt intake and the frequency of salty-food intake [22, 23]. However, there are few reports on the adverse effects of salt intake, evaluated
according to household unit. In the National Nutrition Survey in Japan (NNSJ), salt intake was evaluated by household unit using the dietary weighing record method. In the present study, we
investigated the relationship between the household salt intake levels and long-term mortality from all-cause, CVD, coronary heart disease (CHD), and stroke in a representative Japanese
cohort based on the NNSJ. METHODS STUDY COHORT AND ETHICS The national integrated project for prospective observation of non-communicable disease and its trend in aged 1980 (NIPPON DATA80)
is a cohort study based on the NNSJ and the National Survey on Circulatory Disorders in Japan conducted by the Japanese government in 1980. The details of the cohort are provided elsewhere
[24,25,26,27]. Briefly, 300 survey districts were randomly selected throughout Japan, and a total of 10,546 individuals aged 30 years and over participated in the baseline survey, with a
participation rate of 77%. Baseline data consisted of a nutritional survey, medical examinations including BP measurement and blood tests, and a self-administered questionnaire on
health-related status and medical history. The present study was conducted in accordance with the Ethics Committee of Shiga University of Medical Science (R2005-021). PARTICIPANTS For the
present analysis, we selected 10,147 participants who were living with someone else, such as another family member, at baseline. Among the participants, 92 were excluded due to extreme
values of simple mean energy intake among household members [<0.5th percentile (1062 kcal/day) and >99.5th percentile (3520 kcal/day)]. Another 1353 participants were excluded for the
following reasons: age 80 years or older (_n_ = 164), history of myocardial infarction (_n_ = 48) or stroke (_n_ = 101), missing baseline information from the nutritional survey (_n_ = 114)
and/or self-administered questionnaire (_n_ = 36) and/or medical examinations (_n_ = 14), and loss to follow-up (_n_ = 886). The remaining 8702 participants were included in the analysis.
DEFINITION OF HOUSEHOLD SALT INTAKE LEVEL AND OTHER NUTRIENTS In the NNSJ of 1980, dietary records for an entire household were collected for three consecutive days, excluding Saturday,
Sunday, and national holidays, using a weighing food record method. Trained dietitians visited the home of participants at least once during the survey, asked to weigh all foods and
beverages, and recorded the amounts consumed by any of the household members during the 3 days. The dietitians reviewed and confirmed the accuracy of the data and assigned food codes using
standard food tables. The dietary records were then used to calculate nutrient and food group intakes for each household [28, 29]. In the present study, we used a simple density of salt as
the household salt intake level (g/1000 kcal). Specifically, we obtained the simple salt density by dividing the total salt consumption (g) by the total energy intake (per 1000 kcal).
Similarly, we used densities to assess other nutrients. For energy-supplying nutrients, intake was calculated as the % of total energy intake (% kcal); other nutrients were calculated as
g/1000 kcal or mg/1000 kcal. OTHER MEASUREMENTS Details of the baseline medical examination are described elsewhere [24,25,26,27]. Body mass index (BMI) was calculated as weight in kilograms
divided by the square of height in meters. Trained observers measured baseline BP using a standard mercury sphygmomanometer. Nonfasting blood samples were obtained and centrifuged soon
after collection. Concentrations of total cholesterol and glucose were measured enzymatically. Information on medical history, smoking status (never, past, and current), alcohol consumption
status (none, occasional, and daily) was collected using a self-administered questionnaire. We used self-reported work exertion level (heavy, relatively heavy, moderate, relatively mild, and
mild) as a proxy for daily physical activity. FOLLOW-UP SURVEY Participants were followed until 2004. The survival status of participants was followed up using registration records required
under the Family Registration Law in the municipalities where participants resided. National Vital Statistics were used to identify causes of death, with permission from the Management and
Coordination Agency of the Japanese government. The underlying causes of mortality in the National Vital Statistics were coded according to the International Classification of Diseases, 9th
Revision (ICD-9) until the end of 1994, and the International Classification of Diseases, 10th Revision (ICD-10) from the beginning of 1995. The details of classification are described
elsewhere [26]. The corresponding ICD-9 and ICD-10 codes used in the present study were as follows: CVD mortality included 393–459 (ICD-9) and I00–I99 (ICD-10), CHD mortality included
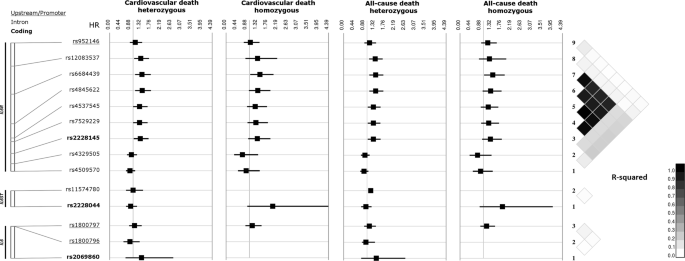
410–414 (ICD-9) and I20–I25 (ICD-10), and stroke mortality included 430–438 (ICD-9) and I60–I69 (ICD-10). STATISTICAL ANALYSIS Hazard ratios (HRs) with 95% confidence intervals (CIs) were
calculated using a Cox proportional hazards model to evaluate the relationship between household salt intake level and all-cause mortality, CVD mortality, CHD mortality, and stroke
mortality. First, we treated household salt intake level as a continuous variable and calculated HRs per 2 g/1000 kcal increment in household salt intake level; one standard deviation of
household salt intake level was 2.02 g/1000 kcal. Second, we calculated HRs for quartiles of household salt intake level, using the lowest quartile as the reference group. For both analyses,
we ran three models: model 1 was adjusted for sex and age; model 2 was adjusted for sex, age, BMI, smoking status, alcohol consumption status, and work exertion level; and model 3 was
adjusted for variables in model 2 plus household intake density of potassium, saturated fatty acids, and long-chain n-3 polyunsaturated fatty acids (the sum of eicosapentaenoic acid and
docosapentaenoic acid) [27]. In considering covariates, we did not include BP in the above three models because we considered that salt intake was a factor that modifies BP. As a sensitivity
analysis, we performed the same analysis excluding those participants who reported the use of antihypertensive medication at baseline. In addition, for CHD mortality, we tested a model in
which serum total cholesterol was adjusted instead of nutrients that effect lipid metabolism, as well as a model in which BMI was not adjusted. We ran all models to calculate _p_ values for
trends, using household salt intake level as a continuous variable. All analyses were performed as sex-combined analyses because the interaction by sex was not significant in most of the
analyses. All data were analyzed using IBM SPSS version 22 (IBM Japan Ltd., Tokyo, Japan). All reported _p_ values are two-tailed; _p_ < 0.05 was considered to indicate statistical
significance. RESULTS The mean age (standard deviation) of the 8702 participants was 49.4 (12.6) years, and 44.4% of participants were men. Table 1 summarizes the baseline characteristics of
the participants. Sixty-three percent of participants belonged to households consisting of three to five people. The mean household salt intake level (standard deviation) was 6.25 (2.02)
g/1000 kcal. The proportion of participants taking antihypertensive medication was 10.3%. During the 186,186 person-years of follow-up (mean follow-up period, 21.4 years), there were 2360
deaths; of these, 33.3% (_n_ = 787) were due to CVD, 7.0% (_n_ = 168) were due to CHD, and 15.3% (_n_ = 361) were due to stroke. As shown in Table 2, the HRs for a 2.0 g/1000 kcal increment
in household salt intake level were significantly higher for all-cause mortality, CVD mortality, and CHD mortality in model 1. The association was similar after adjusting for BMI, smoking
status, alcohol consumption status, and work exertion level in model 2. When we adjusted for the intakes of other nutrients in model 3, the positive association also became significant for
stroke mortality; the HRs (95% CIs) for a 2.0 g/1000 kcal increment in household salt intake level were 1.07 (1.02, 1.12) for all-cause mortality, 1.11 (1.03, 1.19) for CVD mortality, 1.25
(1.08, 1.44) for CHD mortality, and 1.12 (1.00, 1.25) for stroke mortality. The results were similar after adjustment for systolic BP at baseline (data not shown). The results were also
similar when we used a multilevel analysis including household as a random effect (data not shown). When we conducted the same analysis after excluding 893 participants with antihypertensive
medication use at baseline, the results were similar (Supplementary Table 1). In addition, in the sensitivity analysis for CHD mortality, the results were similar in the model where serum
total cholesterol was adjusted instead of nutrients affecting lipid metabolism and in the model where BMI was not adjusted (data not shown). DISCUSSION In the present study, we found a
considerable association between household salt intake level and the risk of all-cause, CVD, CHD, and stroke mortality in a long-term cohort study of a representative Japanese population
from a national survey. The relationship was significant and independent of other confounding factors, including sex, age, BMI, smoking and alcohol consumption status, work exertion level,
and the intake of several other nutrients. To our knowledge, this is the first study examining the effect of household salt intake level on long-term mortality risk. We could perform
household-based analysis by using the NNSJ as a baseline assessment of salt intake level, in which all foods and beverages consumed by any household member were assessed as a household unit.
Another strength lies in the methods of the baseline survey. Participants were enrolled from 300 survey districts randomly selected from across Japan. Dietary data obtained for 3 days were
reviewed by trained dieticians using weighed food dietary records, a standardized method applied in the NNSJ. Regarding individual salt intake, many cohort studies and meta-analyses have
clearly shown the adverse effect of excessive salt intake on cause-specific mortality [4, 5, 7]. In Japan, where the salt intake is far above the recommended levels [29], cohort studies have
reported a positive relationship between individual salt intake and CVD events [6], CVD mortality [9], and stroke mortality [8], although these findings were obtained using food frequency
questionnaires. However, we could not find any studies focusing on the effect of household salt intake levels. Therefore, we could not simply compare our findings with previous studies.
Considering our results, the HRs for a 2.0 g/1000 kcal increment in household salt intake level were higher in model 3 in which we added household intake density of potassium and long-chain
n-3 polyunsaturated fatty acids as covariates. In Japan, a considerable amount of salt was consumed as salted pickles, miso soup, salted fish, and boiled foods [30]. Participants in
households with a high salt intake level may consume many vegetables and fish, and the adjustment of the intakes of the nutrients contained in these foods would have increased the HRs
because these nutrient intakes have been reported to be inversely associated with CVD risk [27, 31]. In our analysis, the results were similar after adjustment for systolic BP at baseline,
even though BP was considered to be an important mediator between salt intake and mortality [1,2,3]. This finding can be explained as follows: Participants who belonged to a household with a
high salt intake level would consume a large amount of salt regularly, which might cause long-term BP increase during the follow-up period. Therefore, the relationship between household
salt intake and long-term mortality could not be significantly adjusted for only BP at baseline. When we excluded the participants with antihypertensive medication use at baseline, the
results were also similar but appeared to be clearer than those of the main analysis. This may be due to a reverse causality that, in households with treated participants, salt intake level
may have already been reduced or salt intake level would decrease during the follow-up period. In Asian countries such as Japan, a main source of salt is seasoning used in cooking, including
salt, soy sauce, miso paste, and table salt used at home [16, 17, 32]. In Japan, eating out is not very common. According to the results of the NNSJ in 2016, ~80% of participants ate
breakfast and dinner at home, and ~60% also ate lunch at home [33]. Women in Japan spend much more time engaged in food management (1.5 h/day) than men (0.2 h/day); [34] therefore, women
generally prepare meals for household members. Hot pot dishes such as miso soup and _nimono_ (simmered dishes, mostly seasoned with soy sauce) are usually cooked at home and consumed by all
household members. Furthermore, household members share table salt and self-serve soy sauce in the same dining environment. Under these circumstances, Michikawa et al. reported that a
woman’s salt taste influenced her husband’s BP [35]. Therefore, it is important to understand the effect of household salt intake in countries where meals cooked at home are most frequently
consumed. In many Western countries, the main source of salt is salt added to processed foods produced by the food industry [16, 36]. A public health intervention in the United Kingdom to
reduce the amount of salt in bread led to successfully lowering salt intake among the population that consumed commercially prepared bread [37, 38]. It has been suggested that the preference
for salty taste begins to develop around the age of 4 months [18], but the preference for salt can be lowered after ~3 months on a low-salt diet, even in adults [19]. Household members
cannot modify the amount of salt that has already been added to a meal. Therefore, the perspective of the household is important in Western countries as well as in other regions. Further
investigation of household salt intake levels is needed among different populations. Several limitations of our study need to be considered. First, in the evaluation of household salt intake
level, table salt added by household members themselves and salt added to foods consumed when eating out could not be accurately assessed. However, household members usually use salt and
other condiments on the same table, and the proportion of the Japanese population that consumed meals outside the home in 1980 was not high. Second, household salt intake level and other
variables were assessed only at baseline in 1980; we did not consider the changes in household and dietary habits, although the number of single-person households has been increasing [39]
and the consumption of processed foods and eating out has been increasing especially in the younger generation during the long follow-up period [17]. Third, we did not adjust for alcohol
intake in the multivariate-adjusted models. Fourth, we did not consider other factors of the household, such as family members with similar genetic factors and socioeconomic status.
CONCLUSION In the present 24-year cohort study of a representative Japanese population, we found a positive linear association between household salt intake level and all-cause, CVD, CHD,
and stroke mortality. Our findings highlight the importance of considering the entire household to improve health interventions for salt reduction. Further investigation is needed among
different populations to confirm our results. REFERENCES * Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, et al. Intersalt revisited: further analyses of 24 h sodium
excretion and blood pressure within and across populations. Intersalt Cooperative Research Group. Br Med J. 1996;312:1249–53. https://doi.org/10.1136/bmj.312.7041.1249. Article CAS Google
Scholar * He FJ, Li J, MacGregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomised trials. Br Med J.
2013;346:f1325–f1325. https://doi.org/10.1136/bmj.f1325. Article Google Scholar * Miura K, Okuda N, Turin TC, Takashima N, Nakagawa H, Nakamura K, et al. Dietary salt intake and blood
pressure in a representative Japanese population: baseline analyses of NIPPON DATA80. J Epidemiol. 2010;20 Suppl 3:S524–30. Article PubMed PubMed Central Google Scholar * Strazzullo P,
D’Elia L, Kandala N-B, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. Br Med J. 2009;339:b4567–b4567. https://doi.org/10.1136/bmj.b4567.
Article Google Scholar * Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med.
2014;371:624–34. https://doi.org/10.1056/NEJMoa1304127. Article PubMed Google Scholar * Takachi R, Inoue M, Shimazu T, Sasazuki S, Ishihara J, Sawada N, et al. Consumption of sodium and
salted foods in relation to cancer and cardiovascular disease: The Japan public health center-based prospective study. Am J Clin Nutr. 2010;91:456–64.
https://doi.org/10.3945/ajcn.2009.28587. Article CAS PubMed Google Scholar * Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on
health: systematic review and meta-analyses. Br Med J. 2013;346:1–20. https://doi.org/10.1136/bmj.f1326. Article Google Scholar * Nagata C, Takatsuka N, Shimizu N, Shimizu H. Sodium intake
and risk of death from stroke in Japanese men and women. Stroke. 2004;35:1543–7. https://doi.org/10.1161/01.STR.0000130425.50441.b0. Article PubMed Google Scholar * Umesawa M, Iso H,
Date C, Yamamoto A, Toyoshima H, Watanabe Y, et al. Relations between dietary sodium and potassium intakes and mortality from cardiovascular disease: the Japan Collaborative Cohort study for
evaluation of cancer risks. Am J Clin Nutr. 2008;88:195–202. https://doi.org/10.1093/ajcn/88.1.195 Article CAS PubMed Google Scholar * Cook NR, Appel LJ, Whelton PK. Sodium intake and
all-cause mortality over 20 years in the trials of hypertension prevention. J Am Coll Cardiol. 2016;68:1609–17. https://doi.org/10.1016/j.jacc.2016.07.745. Article CAS PubMed PubMed
Central Google Scholar * Liu H, Gao X, Zhou L, Wu Y, Li Y, Mai J, et al. Urinary sodium excretion and risk of cardiovascular disease in the Chinese population: a prospective study.
Hypertens Res. 2018;41:849–55. https://doi.org/10.1038/s41440-018-0091-8. Article CAS PubMed Google Scholar * Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al.
DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research
Group. N Engl J Med. 2001;344:3–10. https://doi.org/10.1056/NEJM200101043440101. Article CAS PubMed Google Scholar * Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK,
et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). Br Med J. 2007;334:885–8.
https://doi.org/10.1136/bmj.39147.604896.55. Article Google Scholar * World Health Organization (WHO). Guideline: Sodium intake for adults and children. Geneva, Switzerland, 2012. 1–46.
http://www.who.int/nutrition/publications/guidelines/sodium_intake/en/. * Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global, regional and national sodium intakes in
1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3. https://doi.org/10.1136/bmjopen-2013-003733. Article PubMed PubMed
Central Google Scholar * Anderson CAM, Appel LJ, Okuda N, Brown IJ, Chan Q, Zhao L, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and
men aged 40 to 59 years: the INTERMAP Study. J Am Diet Assoc. 2010;110:736–45. https://doi.org/10.1016/j.jada.2010.02.007. Article CAS PubMed PubMed Central Google Scholar * Asakura K,
Uechi K, Masayasu S, Sasaki S. Sodium sources in the Japanese diet: difference between generations and sexes. Public Health Nutr. 2016;19:2011–23. https://doi.org/10.1017/S1368980015003249.
Article PubMed Google Scholar * Beauchamp GK, Cowart BJ, Mennella JA, Marsh RR. Infant salt taste: developmental, methodological, and contextual factors. Dev Psychobiol. 1994;27:353–65.
https://doi.org/10.1002/dev.420270604. Article CAS PubMed Google Scholar * Mattes RD. The taste for salt in humans. Am J Clin Nutr. 1997;65:692S–697S.
https://doi.org/10.1093/ajcn/65.2.692S. Article CAS PubMed Google Scholar * Service C, Grimes C, Riddell L, He F, Campbell K, Nowson C. Association between parent and child dietary
sodium and potassium intakes as assessed by 24-h urinary excretion. Nutrients. 2016;8:191 https://doi.org/10.3390/nu8040191. Article CAS PubMed PubMed Central Google Scholar * Patterson
TL, Rupp JW, Sallis JF, Atkins CJ, Nader PR. Aggregation of dietary calories, fats, and sodium in Mexican-American and Anglo families. Am J Prev Med. 1988;4:75–82.
http://www.ncbi.nlm.nih.gov/pubmed/3395494. Article CAS PubMed Google Scholar * Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Inaba Y, et al. Salt preference and mortality from stroke
and coronary heart disease for Japanese men and women: the JACC study. Prev Med. 2012;54:32–7. https://doi.org/10.1016/j.ypmed.2011.10.013. Article PubMed Google Scholar * Takachi R,
Ishihara J, Iwasaki M, Ishii Y, Tsugane S. Self-reported taste preference can be a proxy for daily sodium intake in middle-aged Japanese adults. J Acad Nutr Diet. 2014;114:781–7.
https://doi.org/10.1016/j.jand.2013.07.043. Article PubMed Google Scholar * Ueshima H, Choudhury SR, Okayama A, Hayakawa T, Kita Y, Kadowaki T, et al. Cigarette smoking as a risk factor
for stroke death in Japan NIPPON DATA80. Stroke. 2004;35:1836–41. https://doi.org/10.1161/01.STR.0000131747.84423.74. Article CAS PubMed Google Scholar * Okuda N, Miura K, Yoshita K,
Matsumura Y, Okayama A, Nakamura Y, et al. Integration of Data from NIPPON DATA80/90 and National Nutrition Survey in Japan: for cohort studies of representative Japanese oN Nutrition. J
Epidemiol. 2010;20:S506–S514. https://doi.org/10.2188/jea.JE20090218. Article PubMed PubMed Central Google Scholar * Okamura T, Hayakawa T, Kadowaki T, Kita Y, Okayama A, Elliott P, et
al. Resting heart rate and cause-specific death in a 16.5-year cohort study of the Japanese general population. Am Heart J. 2004;147:1024–32. https://doi.org/10.1016/j.ahj.2003.12.020.
Article PubMed Google Scholar * Miyagawa N, Miura K, Okuda N, Kadowaki T, Takashima N, Nagasawa S, et al. Long-chain n-3 polyunsaturated fatty acids intake and cardiovascular disease
mortality risk in Japanese: A 24-year follow-up of NIPPON DATA80. Atherosclerosis. 2014;232:384–9. https://doi.org/10.1016/j.atherosclerosis.2013.11.073. Article CAS PubMed Google Scholar
* Yoshiike N, Matsumura Y, Iwaya M, Sugiyama M, Yamaguchi M. National Nutrition Survey in Japan. J Epidemiol. 1996;6:S189–200. https://doi.org/10.2188/jea.6.3sup_189. Article CAS PubMed
Google Scholar * Saito A, Imai S, Htun NC, Okada E, Yoshita K, Yoshiike N, et al. The trends in total energy, macronutrients and sodium intake among Japanese: findings from the 1995-2016
National Health and Nutrition Survey. Br J Nutr. 2018;120:424–34. https://doi.org/10.1017/S0007114518001162. Article CAS PubMed Google Scholar * Okuda N, Okayama A, Miura K, Yoshita K,
Saito S, Nakagawa H, et al. Food sources of dietary sodium in the Japanese adult population: the international study of macro-/micronutrients and blood pressure (INTERMAP). Eur J Nutr.
2017;56:1269–80. https://doi.org/10.1007/s00394-016-1177-1. Article CAS PubMed Google Scholar * Larsson SC, Orsini N, Wolk A. Dietary potassium intake and risk of stroke. Stroke.
2011;42:2746–50. https://doi.org/10.1161/strokeaha.111.622142. Article CAS PubMed Google Scholar * Zhao F, Zhang P, Zhang L, Niu W, Gao J, Lu L, et al. Consumption and sources of dietary
salt in family members in Beijing. Nutrients. 2015;7:2719–30. https://doi.org/10.3390/nu7042719. Article CAS PubMed PubMed Central Google Scholar * Ministry of Health, Labor and
Welfare. The National Health and Nutrition Survey in Japan, 2017. Ministry of Health, Labor and Welfare; 2018. https://www.mhlw.go.jp/stf/houdou/0000177189_00001.html. Accessed 20 June 2019.
* Ministry of Internal Affairs and Communications. Survey on Time Use and Leisure Activities (2016b). Ministry of Internal Affairs and Communications; 2017.
https://www.stat.go.jp/data/shakai/2016/kekka.html. Accessed 20 June 2019. * Michikawa T, Nishiwaki Y, Okamura T, Asakura K, Nakano M, Takebayashi T. The taste of salt measured by a simple
test and blood pressure in Japanese women and men. Hypertens Res. 2009;32:399–403. https://doi.org/10.1038/hr.2009.31. Article PubMed Google Scholar * Brown IJ, Tzoulaki I, Candeias V,
Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol. 2009;38:791–813. https://doi.org/10.1093/ije/dyp139. Article PubMed Google Scholar * He FJ,
Brinsden HC, Macgregor GA. Salt reduction in the United Kingdom: a successful experiment in public health. J Hum Hypertens. 2014;28:345–52. https://doi.org/10.1038/jhh.2013.105. Article CAS
PubMed Google Scholar * Brinsden HC, He FJ, Jenner KH, MacGregor GA. Surveys of the salt content in UK bread: progress made and further reductions possible. BMJ Open. 2013;3:1–8.
https://doi.org/10.1136/bmjopen-2013-002936. Article Google Scholar * Ministry of Health, Labor and Welfare. Graphical Review of Japanese Household: From Comprehensive Survey of Living
Conditions 2016. Tokyo, Japan, 2018. https://www.mhlw.go.jp/toukei/list/dl/20-21-h28.pdf. Download references ACKNOWLEDGEMENTS The authors are deeply indebted to public health centers that
cooperated in this study and the staff members of the NIPPON DATA80 research group. We also thank Analisa Avila, ELS, of Edanz Group (www.edanzediting.com/ac) for editing a draft of this
manuscript. FOR THE NIPPON DATA80 RESEARCH GROUP Hirotsugu Ueshima1,3, Akira Okayama9, Tomonori Okamura8, Shigeyuki Saitoh10, Kiyomi Sakata11, Atsushi Hozawa12, Takehito Hayakawa13, Yosikazu
Nakamura14, Nobuo Nishi4, Nagako Okuda5, Takayoshi Ohkubo15, Fumiyoshi Kasagi16, Yoshitaka Murakami17, Toru Izumi18, Yasuhiro Matsumura19, Toshiyuki Ojima20, Koji Tamakoshi21, Hideaki
Nakagawa22, Yoshikuni Kita23, Katsuyuki Miura1,3, Aya Kadota1, Akira Fujiyoshi7, Naomi Miyamatsu2, Yasuyuki Nakamura24, Katsushi Yoshita6, Yoshihiro Miyamoto25, Kazunori Kodama26 and Yutaka
Kiyohara27 FUNDING This study was supported by a grant-in-aid from the Ministry of Health, Labor and Welfare, under the auspices of the Japanese Association for Cerebro-cardiovascular
Disease Control; a Research Grant for Cardiovascular Diseases (7A-2) from the Ministry of Health, Labor and Welfare; Health and Labor Sciences Research Grants, Japan (Comprehensive Research
on Aging and Health) [H11-Chouju-046, H14-Chouju-003, H17-Chouju-012, H19-Chouju-Ippan-014]; and Comprehensive Research on Lifestyle Related Diseases, including Cardiovascular Diseases and
Diabetes Mellitus [H22-Junkankitou-Seishuu-Sitei-017, H25-Junkankitou-Seishuu-Sitei-022, H30-Junkankitou-Seishuu-Sitei-002]). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of
Public Health, Shiga University of Medical Science, Shiga, Japan Azusa Shima, Katsuyuki Miura, Aya Kadota, Keiko Kondo, Hirotsugu Ueshima, Hirotsugu Ueshima, Katsuyuki Miura & Aya Kadota
* Department of Clinical Nursing, Shiga University of Medical Science, Shiga, Japan Naomi Miyamatsu & Naomi Miyamatsu * Center for Epidemiologic Research in Asia, Shiga University of
Medical Science, Shiga, Japan Katsuyuki Miura, Hirotsugu Ueshima, Hirotsugu Ueshima & Katsuyuki Miura * International Center for Nutrition and Information, National Institute of
Biomedical Innovation, Health and Nutrition, Tokyo, Japan Naoko Miyagawa & Nobuo Nishi * Department of Health and Nutrition, University of Human Arts and Sciences, Saitama, Japan Nagako
Okuda & Nagako Okuda * Department of Food and Human Health Science, Osaka City University, Graduate School of Human Life Science, Osaka, Japan Katsushi Yoshita & Katsushi Yoshita *
Department of Hygiene, Wakayama Medical University, Wakayama, Japan Harumitsu Suzuki & Akira Fujiyoshi * Department of Preventive Medicine and Public Health, Keio University School of
Medicine, Tokyo, Japan Tomonori Okamura & Tomonori Okamura * Research Institute of Strategy for Prevention, Tokyo, Japan Akira Okayama & Akira Okayama * School of Health Sciences,
Sapporo Medical University, Sapporo, Hokkaido, Japan Shigeyuki Saitoh * Department of Hygiene and Preventive Medicine, Iwate Medical University, Morioka, Iwate, Japan Kiyomi Sakata *
Department of Preventive Medicine and Epidemiology, Tohoku Medical Megabank Organization, Tohoku University, Sendai, Miyagi, Japan Atsushi Hozawa * Kinugasa Research Organization,
Ritsumeikan University, Kyoto, Japan Takehito Hayakawa * Department of Public Health, Jichi Medical University, Shimotsuke, Tochigi, Japan Yosikazu Nakamura * Department of Hygiene and
Public Health Teikyo University School of Medicine, Tokyo, Japan Takayoshi Ohkubo * Institute of Radiation Epidemiology, Radiation Effects Association, Tokyo, Japan Fumiyoshi Kasagi *
Department of Medical Statistics, Toho University, Tokyo, Japan Yoshitaka Murakami * Kitasato University, Sagamihara, Kanagawa, Japan Toru Izumi * Faculty of Health and Nutrition, Bunkyo
University, Chigasaki, Kanagawa, Japan Yasuhiro Matsumura * Department of Community Health and Preventive Medicine, Hamamatsu University School of Medicine, Hamamatsu, Shizuoka, Japan
Toshiyuki Ojima * Department of Public Health and Health Information Dynamics, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan Koji Tamakoshi * Medical Research
Institute, Kanazawa Medical University, Kanazawa, Ishikawa, Japan Hideaki Nakagawa * Faculty of Nursing Science, Tsuruga Nursing University, Tsuruga, Fukui, Japan Yoshikuni Kita * Department
of Food Science and Human Nutrition, Ryukoku University, Otsu, Shiga, Japan Yasuyuki Nakamura * Department of Preventive Cardiology, National Cerebral and Cardiovascular Center, Suita,
Osaka, Japan Yoshihiro Miyamoto * Radiation Effects Research Foundation, Hiroshima, Japan Kazunori Kodama * Hisayama Research Institute for Lifestyle Diseases, Hisayama-cho, Fukuoka, Japan
Yutaka Kiyohara Authors * Azusa Shima View author publications You can also search for this author inPubMed Google Scholar * Naomi Miyamatsu View author publications You can also search for
this author inPubMed Google Scholar * Katsuyuki Miura View author publications You can also search for this author inPubMed Google Scholar * Naoko Miyagawa View author publications You can
also search for this author inPubMed Google Scholar * Nagako Okuda View author publications You can also search for this author inPubMed Google Scholar * Katsushi Yoshita View author
publications You can also search for this author inPubMed Google Scholar * Aya Kadota View author publications You can also search for this author inPubMed Google Scholar * Harumitsu Suzuki
View author publications You can also search for this author inPubMed Google Scholar * Keiko Kondo View author publications You can also search for this author inPubMed Google Scholar *
Tomonori Okamura View author publications You can also search for this author inPubMed Google Scholar * Akira Okayama View author publications You can also search for this author inPubMed
Google Scholar * Hirotsugu Ueshima View author publications You can also search for this author inPubMed Google Scholar CONSORTIA FOR THE NIPPON DATA80 RESEARCH GROUP * Hirotsugu Ueshima * ,
Akira Okayama * , Tomonori Okamura * , Shigeyuki Saitoh * , Kiyomi Sakata * , Atsushi Hozawa * , Takehito Hayakawa * , Yosikazu Nakamura * , Nobuo Nishi * , Nagako Okuda * , Takayoshi
Ohkubo * , Fumiyoshi Kasagi * , Yoshitaka Murakami * , Toru Izumi * , Yasuhiro Matsumura * , Toshiyuki Ojima * , Koji Tamakoshi * , Hideaki Nakagawa * , Yoshikuni Kita * , Katsuyuki Miura *
, Aya Kadota * , Akira Fujiyoshi * , Naomi Miyamatsu * , Yasuyuki Nakamura * , Katsushi Yoshita * , Yoshihiro Miyamoto * , Kazunori Kodama * & Yutaka Kiyohara CORRESPONDING AUTHOR
Correspondence to Katsuyuki Miura. ETHICS DECLARATIONS CONFLICT OF INTEREST The authors declare that they have no conflict of interest. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer
Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Members of the NIPPON DATA80 Research Group are listed below Acknowledgement.
SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Shima, A., Miyamatsu, N., Miura, K. _et al._
Relationship of household salt intake level with long-term all-cause and cardiovascular disease mortality in Japan: NIPPON DATA80. _Hypertens Res_ 43, 132–139 (2020).
https://doi.org/10.1038/s41440-019-0349-9 Download citation * Received: 03 July 2019 * Revised: 05 September 2019 * Accepted: 06 September 2019 * Published: 21 November 2019 * Issue Date:
February 2020 * DOI: https://doi.org/10.1038/s41440-019-0349-9 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * Household * Salt intake *
Cardiovascular diseases * Cohort study