- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
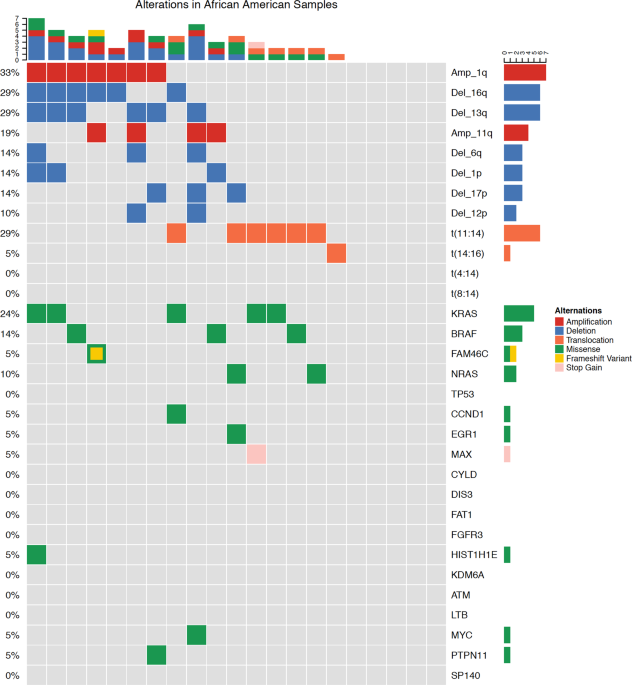
Caucasian Americans (CA) compared with African Americans (AA) have a twofold increased incidence of multiple myeloma (MM) and have an earlier age of diagnosis. However, there is sparse
information regarding underlying biological differences across racial/ethnic groups. We characterized genetic alterations using a targeted next-generation sequencing assay called myTYPE,
developed at MSKCC, allowing capture of somatic mutations, IgH translocations, gains/losses, and hyperdiploidy. Samples were obtained from the NIH Plasma Cell Dyscrasia Racial Disparity
Cohort. In total, 68 patient samples were successfully sequenced and manually curated based on well-established databases. Of the 68 patient samples (47 CA, 21 AA), 84% had at least one type
of genomic alteration. Importantly, the IgH translocation, t(11;14), was observed more frequently in the AA group (0 vs. 29%, p = 0.001). Known oncogenic somatic non-synonymous mutations
were found in 18 genes and indels in 2 genes. KRAS mutations were the most common mutation found in 16% of patients followed by NRAS and BRAF mutations. TP53 somatic mutations appeared to be
more common in CA but lacked significance. This proof-of-principle study indicates the presence of varying underlying tumor biology between racial groups and supports the need of future
prospective trials to capture these molecular characteristics.
Despite advancements in the understanding and treatment of multiple myeloma (MM), a racial disparity in clinical presentation and outcomes remain. Compared with Caucasian Americans (CA),
African Americans (AA) matched for socioeconomics, age, and gender have a twofold increased incidence of MM, have an earlier average age at diagnosis by 5–10 years, and have gained less
benefit from the advent of novel agents in the last decade1,2. These differences have not been shown to be attributable to disparities in access to medical care. In addition, over the past
decade, improvements in survival with the introduction of proteasome inhibitors and immunomodulatory agents is predominantly observed in CA. Costa et al.3 observed improvements in 10-year
relative survival rates (RSRs) in all racial groups