- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
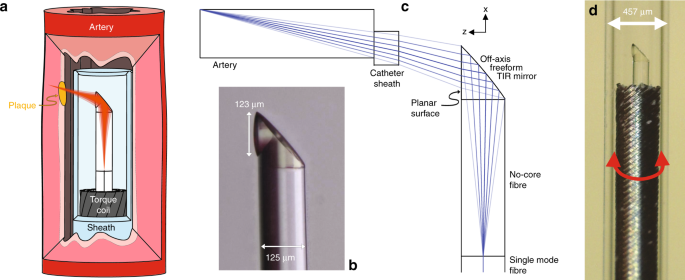
Preclinical and clinical diagnostics increasingly rely on techniques to visualize internal organs at high resolution via endoscopes. Miniaturized endoscopic probes are necessary for imaging
small luminal or delicate organs without causing trauma to tissue. However, current fabrication methods limit the imaging performance of highly miniaturized probes, restricting their
widespread application. To overcome this limitation, we developed a novel ultrathin probe fabrication technique that utilizes 3D microprinting to reliably create side-facing freeform
micro-optics (410,000 patients to improve clinical outcomes5. In addition, OCT has become a widely used tool for assessments in preclinical animal models6,7.
Despite these advances, there remains a practical but unmet need for miniaturized high-resolution probes that not only enable the imaging of delicate narrow luminal organs and small animals
but also prevent the potentially severe adverse events from trauma arising from endoscope insertion1,4,7. Specifically, a high resolution and a large depth of focus are necessary for the
effective surveillance of pathological changes6,7,8 but are extremely challenging to achieve with a miniaturized probe2,8,9,10,11,12. For example, mouse models are a commonly used animal
model for cardiovascular disease13, and a miniaturized probe with a 483 µm diameter was reported for intravascular mouse imaging7. However, the reported probe was not able to image
microstructures deeper than 100 μm owing to its short depth of focus and lacked the resolution to provide a visualization of the relevant structures such as adipose cells14, cholesterol
crystals (CCs)15,16, and connective tissue7, which are on the scale of tens of microns.
Current probe fabrication techniques are limited when used for highly miniaturized probes, resulting in spherical aberration, low resolution, or a shallow depth of focus2,9,10,11,12. In
optical design, there is a traditional trade-off of high resolution (large numerical aperture, NA), resulting in a rapidly diverging light beam with a small depth of focus and poor
resolution (small NA) used to achieve a large depth of focus. Good designs have been attempted to find the optimal compromise between sufficient resolution and depth of focus10,11,12,17.
Unfortunately, with miniaturized probes, the physical aperture of the probe is very small, and no appropriate compromise may exist. The small scale of the optics also makes it very
challenging to correct for spherical aberration, which can further degrade the resolution and depth of focus10. Usually, the correction of the spherical aberration of a single lens is only
possible by using an aspherical lens profile (described by a polynomial instead of a circle equation). This shape, however, is difficult to realize on a fiber tip where lenses are often made
using a melting process (e.g., creating a spherical ball lens with a profile described by a circle equation).
In OCT imaging, these issues are exacerbated because endoscopic and intravascular probes are deployed within a transparent catheter sheath, both to protect the animal or patient from trauma
as the probe is rotated to perform scanning and to prevent cross-contamination when re-used across multiple animals. Optically, this transparent sheath corresponds to a negative cylindrical
lens and causes astigmatism2,10,18. Astigmatism increases the decay of the lateral resolution of a miniaturized probe18. As a result, the correction of these nonchromatic aberrations is
critical to achieve the best possible resolution over the desired depth of focus with a miniaturized probe9,18.
Current methods of micro-optic fabrication lack the capability to mitigate these nonchromatic aberrations10. Miniaturized OCT probes have been fabricated either by assembling the probe from
discrete micro-optical elements (e.g., prisms and lenses)1,2 or by splicing fiber lenses, such as gradient-index (GRIN) fiber or fiber-based ball lenses, directly onto the fiber8,9,19,20.
However, restrictions in the index profile of the GRIN lens/fiber elements10 (parabolic profile inherently causing aberrations) and in the shape of ball lenses lead to spherical aberrations
and limit the ability to correct astigmatism, resulting in probes that fail to achieve a high resolution over a large depth of focus10,18. Ultrafast laser nanostructuring of
photopolymers21,22,23 is a viable alternative to create micro-optical components with complex shapes, high accuracy, low surface roughness, and sub-µm precise alignment24,25,26,27. In
earlier work, we showed the potential of this approach to fabricate a discrete optical element that may be glued to an optical fiber to enable OCT imaging28. However, this preliminary work
did not explore the potential of the technology to correct aberrations, which limit the performance of micro-optics. In addition, the requirement to attach a discrete optical element to the
end of an optical fiber presents additional challenges in scaling the manufacture of these probes. The full potential of this technology in the field of endoscopic OCT has not been exploited
thus far.
Here, we have developed an ultrathin monolithic OCT endoscope that overcomes the aforementioned limitations by using two-photon polymerization to 3D print 125-μm-diameter micro-optics
directly onto the optical fiber (Fig. 1). Freeform micro-optics have been created for correcting the nonchromatic aberrations of highly miniaturized probes, which cannot be fabricated using
traditional techniques. The ultrathin OCT endoscope achieved a measured full width at half maximum (FWHM) focal spot size of 12.4 μm and effective depths of focus (the depth range in which
FWHM