- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT BACKGROUND Residential mobility can introduce exposure misclassification in pediatric epidemiology studies using birth address only. OBJECTIVE We examined whether residential
mobility varies by sociodemographic factors and urbanicity/rurality among children with cancer. METHODS Our study included 400 children born in Pennsylvania during 2002–2015 and diagnosed
with leukemia at ages 2–7 years. Addresses were obtained from state registries at birth and diagnosis. We considered three aspects of mobility between birth and diagnosis: whether a child
moved, whether a mover changed census tract, and distance moved. We evaluated predictors of these aspects in urban- and rural-born children using chi-square, _t_-tests, and regression
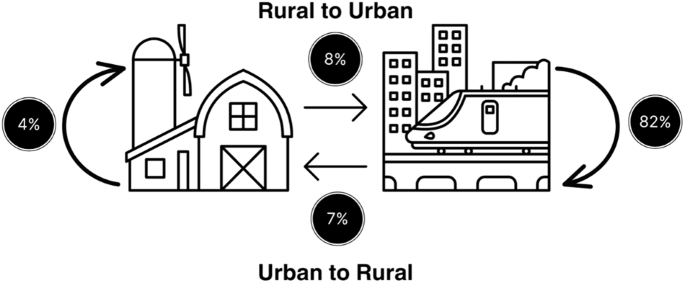
analyses. RESULTS Overall, 58% of children moved between birth and diagnosis; suburban/rural-born children were more likely to move than urban-born children (67% versus 57%). The mean
distance moved was 16.7 km in suburban/rural-born and 14.8 km in urban-born movers. In urban-born children, moving between birth and diagnosis was associated with race, education,
participation in the Nutrition Program for Women, Infants and Children (WIC), and census tract-level income (all χ2 _p_ < 0.01). Urban-born movers tended to be born in a census tract with
a higher Social Vulnerability Index than non-movers (_t_-test _p_ < 0.01). No factors were statistically significantly associated with any of the residential mobility metrics in
suburban/rural-born children, although the sample size was small. IMPACT STATEMENT In this study of a vulnerable population of children with cancer, we found that rural-born children were
more likely to move than urban-born children, however, the frequency of movers changing census tracts was equivalent. Mobility in urban-born children, but not rural-born, was associated with
several social factors, although the sample size for rural-born children was small. Mobility could be an important source of misclassification depending on the spatial heterogeneity and
resolution of the exposure data and whether the social factors are related to exposures or health outcomes. Our results highlight the importance of considering differences in mobility
between urban and rural populations in spatial research. Access through your institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS
OPTIONS Access through your institution Subscribe to this journal Receive 6 print issues and online access $259.00 per year only $43.17 per issue Learn more Buy this article * Purchase on
SpringerLink * Instant access to full article PDF Buy now Prices may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about
institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS GEOGRAPHIC FOOTPRINTS OF LIFE EXPECTANCY INEQUALITIES IN THE STATE OF GENEVA,
SWITZERLAND Article Open access 02 December 2021 GEOGRAPHICAL VARIATION OF COMMON CHILDHOOD ILLNESS AND ITS ASSOCIATED FACTORS AMONG UNDER-FIVE CHILDREN IN ETHIOPIA: SPATIAL AND MULTILEVEL
ANALYSIS Article Open access 17 January 2023 INEQUITIES IN SPATIAL ACCESS TO CHILDBIRTH CARE IN THE GRAND CONAKRY CONURBATION, GUINEA Article Open access 23 April 2025 DATA AVAILABILITY Data
for this study were obtained from the Pennsylvania Cancer Registry and the Pennsylvania Department of Health Bureau of Health Statistics and Registries. The authors do not own these data
and are not permitted to share them. REFERENCES * Bell ML, Banerjee G, Pereira G. Residential mobility of pregnant women and implications for assessment of spatially-varying environmental
exposures. J Expo Sci Environ Epidemiol. 2018;28:470–80. Article PubMed Google Scholar * Bell ML, Belanger K. Review of research on residential mobility during pregnancy: consequences for
assessment of prenatal environmental exposures. J Expo Sci Environ Epidemiol. 2012;22:429–38. Article PubMed PubMed Central Google Scholar * Hodgson S, Lurz PW, Shirley MD, Bythell M,
Rankin J. Exposure misclassification due to residential mobility during pregnancy. Int J Hyg Environ Health. 2015;218:414–21. Article PubMed Google Scholar * Ling C, Heck JE, Cockburn M,
Liew Z, Marcotte E, Ritz B. Residential mobility in early childhood and the impact on misclassification in pesticide exposures. Environ Res. 2019;173:212–20. Article CAS PubMed PubMed
Central Google Scholar * Urayama KY, Von Behren J, Reynolds P, Hertz A, Does M, Buffler PA. Factors Associated With Residential Mobility in Children With Leukemia: Implications For
Assigning Exposures. Ann Epidemiol. 2009;19:834–40. Article PubMed PubMed Central Google Scholar * Barrington-Trimis JL, Cockburn M, Metayer C, Gauderman WJ, Wiemels J, McKean-Cowdin R.
Trends in childhood leukemia incidence over two decades from 1992 to 2013. Int J Cancer. 2017;140:1000–8. Article CAS PubMed Google Scholar * Poole C, Greenland S, Luetters C, Kelsey JL,
Mezei G. Socioeconomic status and childhood leukaemia: a review. Int J Epidemiol. 2006;35:370–84. Article PubMed Google Scholar * Brokamp C, LeMasters GK, Ryan PH. Residential mobility
impacts exposure assessment and community socioeconomic characteristics in longitudinal epidemiology studies. J Expo Sci Environ Epidemiol. 2016;26:428–34. Article PubMed PubMed Central
Google Scholar * Tee Lewis PG, Chen T-Y, Chan W, Symanski E. Predictors of residential mobility and its impact on air pollution exposure among children diagnosed with early childhood
leukemia. J Expo Sci Environ Epidemiol. 2019;29:510–9. Article PubMed PubMed Central Google Scholar * Canfield MA, Ramadhani TA, Langlois PH, Waller DK. Residential mobility patterns and
exposure misclassification in epidemiologic studies of birth defects. J Expo Sci Environ Epidemiol. 2006;16:538–43. Article PubMed Google Scholar * Saucy A, Gehring U, Olmos S, Delpierre
C, de Bont J, Gruzieva O, et al. Effect of residential relocation on environmental exposures in European cohorts: An exposome-wide approach. Environ Int. 2023;173:107849. Article PubMed
Google Scholar * Bennett EE, Lynch KM, Xu X, Park ES, Ying Q, Wei J, et al. Characteristics of movers and predictors of residential mobility in the Atherosclerosis Risk in Communities
(ARIC) cohort. Health Place. 2022;74:102771. Article PubMed PubMed Central Google Scholar * South SJ, Deane GD. Race and Residential Mobility: Individual Determinants and Structural
Constraints. Soc Forces. 1993;72:147–67. Article Google Scholar * James WL. All Rural Places Are Not Created Equal: Revisiting the Rural Mortality Penalty in the United States. Am J Public
Health. 2014;104:2122–9. Article PubMed PubMed Central Google Scholar * Cosby AG, Neaves TT, Cossman RE, Cossman JS, James WL, Feierabend N, et al. Preliminary Evidence for an Emerging
Nonmetropolitan Mortality Penalty in the United States. Am J Public Health. 2008;98:1470–2. Article PubMed PubMed Central Google Scholar * Cossman JS, James WL, Cosby AG, Cossman RE.
Underlying Causes of the Emerging Nonmetropolitan Mortality Penalty. Am J Public Health. 2010;100:1417–9. Article PubMed PubMed Central Google Scholar * Haines MR. The urban mortality
transition in the united states, 1800-1940. Annales de démographie historique. 2001;101:33–64. Article Google Scholar * Pampel FC, Rogers RG. Socioeconomic Status, Smoking, and Health: A
Test of Competing Theories of Cumulative Advantage. J Health Soc Behav. 2004;45:306–21. Article PubMed Google Scholar * Cockerham WC. Health Lifestyle Theory and the Convergence of Agency
and Structure. J Health Soc Behav. 2005;46:51–67. Article PubMed Google Scholar * Hartley D. Rural Health Disparities, Population Health, and Rural Culture. Am J Public Health.
2004;94:1675–8. Article PubMed PubMed Central Google Scholar * Adler NE, Boyce, T, Chesney, MA, Cohen, S, Folkman, S, Kahn, et al. Socioeconomic status and health: The challenge of the
gradient. Am Psychol. 1994;49:15–24. * Clark CJ, Johnson NP, Soriano M, Warren JL, Sorrentino KM, Kadan-Lottick NS, et al. Unconventional Oil and Gas Development Exposure and Risk of
Childhood Acute Lymphoblastic Leukemia: A Case & Control Study in Pennsylvania, 2009-2017. Environ Health Perspect. 2022;130:087001. Article PubMed PubMed Central Google Scholar *
Doerrenberg M, Kloetgen A, Hezaveh K, Wössmann W, Bleckmann K, Stanulla M, et al. T-cell acute lymphoblastic leukemia in infants has distinct genetic and epigenetic features compared to
childhood cases. Genes, Chromosomes Cancer 2017;56:159–67. Article CAS PubMed Google Scholar * Wiemels J. Chromosomal translocations in childhood leukemia: natural history, mechanisms,
and epidemiology. J Natl Cancer Inst Monogr. 2008;39:87–90. * United States Census Bureau. 2000-2010. https://data.census.gov/cedsci/. * Agency for Toxic Substances and Disease Registry
(ATSDR). The social vulnerability index 2021. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html. * United States Department of Agriculture ERS. Rural-Urban Commuting Area Codes. 2020.
https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx. * Salvati L. Residential mobility and the local context: Comparing long-term and short-term spatial trends of
population movements in Greece. Socio-Econ Plan Sci 2020;72:100910. Article Google Scholar * Pui C-H. Acute Lymphoblastic Leukemia. In: Schwab M, editor. Encyclopedia of Cancer. Berlin,
Heidelberg: Springer Berlin Heidelberg; 2011. p. 23-6. Download references ACKNOWLEDGEMENTS This research was supported in part by National Priority Research Project under Assistance
Agreement No. CR839249 awarded by the U.S. Environmental Protection Agency (EPA) to Yale University. The publication has not been formally reviewed by EPA. The views expressed in this
document are solely those of the authors and do not reflect those of the Agency. EPA does not endorse any products or commercial services mentioned in this publication. Research reported in
this publication was supported in part by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number R01MD016054. CJC was
supported by a T32 training grant from the National Cancer Institute (T32 CA250803). The content is solely the responsibility of the authors and does not represent the official views of the
National Institutes of Health. Some data were supplied by the Bureau of Health Statistics & Registries, Pennsylvania Department of Health, Harrisburg, Pennsylvania. The Pennsylvania
Department of Health specifically disclaims responsibility for any analyses, interpretations or conclusions. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Yale School of Public Health,
Department of Environmental Health Sciences, 60 College St., New Haven, CT, 06510, USA Cassandra J. Clark & Nicole C. Deziel * Yale School of Public Health, Department of Biostatistics,
60 College St., New Haven, CT, 06510, USA Joshua L. Warren * Yale School of the Environment, 195 Prospect Street, New Haven, CT, 06511, USA James E. Saiers & Michelle L. Bell * Yale
School of Public Health, Department of Chronic Disease Epidemiology, 60 College St., New Haven, CT, 06510, USA Xiaomei Ma Authors * Cassandra J. Clark View author publications You can also
search for this author inPubMed Google Scholar * Joshua L. Warren View author publications You can also search for this author inPubMed Google Scholar * James E. Saiers View author
publications You can also search for this author inPubMed Google Scholar * Xiaomei Ma View author publications You can also search for this author inPubMed Google Scholar * Michelle L. Bell
View author publications You can also search for this author inPubMed Google Scholar * Nicole C. Deziel View author publications You can also search for this author inPubMed Google Scholar
CONTRIBUTIONS CJC: Conceptualization, funding acquisition, formal analysis, visualization, writing—original draft and review and editing; JLW: Conceptualization, methodology, writing: review
and editing, MLB: Methodology, writing: review and editing, JES: Writing: review and editing, funding acquisition, XM: Supervision, writing: review and editing, funding acquisition, and
NCD: Conceptualization, supervision, writing—review and editing, funding acquisition. CORRESPONDING AUTHOR Correspondence to Cassandra J. Clark. ETHICS DECLARATIONS COMPETING INTERESTS The
authors declare no competing interests. ETHICAL APPROVAL The study protocol was approved by the Institutional Review Board of Yale University (HIC #2000021809) and the Pennsylvania
Department of Health (IF-0430) and reviewed and approved by the US Environmental Protection Agency (HSR-001162). ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with
regard to jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION RIGHTS AND PERMISSIONS Springer Nature or its licensor
(e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted
manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Clark, C.J.,
Warren, J.L., Saiers, J.E. _et al._ Predictors of early life residential mobility in urban and rural Pennsylvania children with acute lymphoblastic leukemia and implications for
environmental exposure assessment. _J Expo Sci Environ Epidemiol_ 34, 990–999 (2024). https://doi.org/10.1038/s41370-023-00636-9 Download citation * Received: 04 May 2023 * Revised: 08
December 2023 * Accepted: 12 December 2023 * Published: 26 December 2023 * Issue Date: November 2024 * DOI: https://doi.org/10.1038/s41370-023-00636-9 SHARE THIS ARTICLE Anyone you share the
following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative







