- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Misato 1, mitochondrial distribution and morphology regulator (encoded by the _MSTO1_ gene), is involved in mitochondrial distribution and morphology. Recently, _MSTO1_ mutations
have been shown to cause clinical manifestations suggestive of mitochondrial dysfunction, such as muscle weakness, short stature, motor developmental delay, and cerebellar atrophy. Both
autosomal dominant and recessive modes of inheritance have been suggested. We performed whole-exome sequencing in two unrelated patients showing cerebellar atrophy, intellectual disability,
and pigmentary retinopathy. Three novel mutations were identified: c.836 G > A (p.Arg279His), c.1099-1 G > A (p.Val367Trpfs*2), and c.79 C > T (p.Gln27*). Both patients had compound
heterozygous mutations with a combination of protein-truncation mutation and missense mutation, the latter shared by them both. This survey of two patients with recessive and novel _MSTO1_
mutations provides additional clinical and genetic information on the pathogenicity of _MSTO1_ in humans. You have full access to this article via your institution. Download PDF SIMILAR
CONTENT BEING VIEWED BY OTHERS _OTUD6B_-ASSOCIATED INTELLECTUAL DISABILITY: NOVEL VARIANTS AND GENETIC EXCLUSION OF RETINAL DEGENERATION AS PART OF A REFINED PHENOTYPE Article 05 August 2021
MITOCHONDRIAL DNA MUTATIONS IN KOREAN PATIENTS WITH LEBER’S HEREDITARY OPTIC NEUROPATHY Article Open access 08 March 2024 A NOVEL MUTATION LOCATED IN THE INTERMEMBRANE SPACE DOMAIN OF
_AFG3L2_ CAUSES DOMINANT OPTIC ATROPHY THROUGH DECREASING THE STABILITY OF THE ENCODED PROTEIN Article Open access 15 August 2022 INTRODUCTION Mitochondria are present in most somatic cells
(except for red blood cells) and important in a wide range of cellular processes, such as the production of cellular ATP, calcium homeostasis, and apoptosis [1, 2]. Mitochondrial diseases
are characterized by multiple-organ involvement, especially in tissues and organs with high energy demands. Cerebellar ataxia, peripheral neuropathy, muscle weakness, cognitive disorders,
epilepsy, and small stature have been clinically reported to be common neurological symptoms in mitochondrial diseases [1]. Defects in 36 mitochondrial and 245 nuclear genes have been
reported to be causative of human mitochondrial diseases [2] for which all inheritance patterns (mitochondrial, X-linked, autosomal dominant, and recessive) have been identified. [3]. Misato
1, mitochondrial distribution and morphology regulator, a human ortholog of misato in _Drosophila melanogaster_, is encoded by _MSTO1_ at 1q22. _MSTO1_ knockdown with siRNA caused
mitochondrial fragmentation in human HeLa cells and overexpression of recombinant _MSTO1_ induced the aggregation of mitochondria at the perinuclear region in COS-7 cells, indicating that
_MSTO1_ is critical for mitochondrial distribution [4]. Despite its significance for the integrity of mitochondrial functions, until recently, diseases involving _MSTO1_ mutation were
unknown in humans. However, two groups recently and independently reported that _MSTO1_ mutations caused clinical features reflective of mitochondrial dysfunction [5, 6]. Their inheritance
could be either autosomal dominant or recessive [5, 6]. Specifically, Gal et al. reported a heterozygous missense mutation in _MSTO1_, which caused muscle weakness, short stature, motor
developmental delay, and cerebellar atrophy. Functional analysis of the patients’ fibroblasts revealed that _MSTO1_ was involved in mitochondrial morphogenesis and maintenance by supporting
mitochondrial fusion [5]. Meanwhile, Nasca et al. reported biallelic mutations in _MSTO1_, which caused myopathy, optic atrophy, ataxia, serum creatinine kinase (CK) elevation, and severe
cerebellar hypoplasia [6]. Here, we present novel biallelic mutations in _MSTO1_, which cause global developmental delay, cerebellar hypoplasia, and retinitis pigmentosa. The detailed
clinical features are described and genotype–phenotype correlations are discussed. MATERIALS AND METHODS PATIENTS A series of patients with cerebellar atrophy were collected. Detailed
clinical information was obtained by the clinicians examining the patients. The Institutional Review Board of Yokohama City University of Medicine approved the experimental protocols.
Informed consent was obtained from the patients’ guardians, in accordance with Japanese regulatory requirements. SAMPLE PREPARATION AND WHOLE-EXOME SEQUENCING Genomic DNA was isolated from
peripheral blood leukocytes using QuickGene 610 L (Wako, Osaka, Japan). It was then captured using the SureSelect Human All Exon v5 (50 Mb) or v6 (60 Mb) Kit (Agilent Technologies, Santa
Clara, CA, USA), and sequenced on an Illumina HiSeq2500 (Illumina, San Diego, CA, USA) with 101-bp paired-end reads. Exome data processing, variant calling, and variant annotation were
performed as previously described [7]. The average read depth of protein-coding regions ranged from 79.6× to 101.7×, and at least from 96.2 to 97.5% of target bases were sequenced by 10 or
more reads. Common single-nucleotide polymorphisms (SNPs) with minor allele frequencies ≥1% in dbSNP 137 and variants observed in more than 5 of our 575 in-house ethnically matched control
exomes were filtered out. Among the remaining rare variants, we focused on amino acid-altering or splicing-affecting variants. Particular attention was paid to mutations in known causative
genes associated with ataxia, cerebellar atrophy, and other neurodegenerative diseases. _MSTO1_ variants were confirmed by Sanger sequencing with an ABI PRISM 3500xl autosequencer (Life
Technologies, Carlsbad, CA, USA) of PCR products using genomic DNA from patients and their parents as a template. CELL CULTURE, RT-PCR, AND TA CLONING Lymphoblastoid cells derived from
patient 1 harboring c.1099 G>A were grown in Roswell Park Memorial Institute 1640 medium supplemented with 10% fetal bovine serum, tylosin, and antibiotic–antimycotic solution in a 5% CO2
incubator. After incubation with dimethyl sulfoxide (as vehicle control) with/without 30 µM cycloheximide (Sigma) to prevent nonsense-mediated mRNA decay (NMD) for 4 h, total RNA was
extracted using RNeasy Plus Mini kit (Qiagen). Four milligrams of total RNA was subjected to reverse transcription using PrimeScript 1st strand synthesis kit with random hexamers (Takara).
cDNA was isolated from lymphoblastoid cells from a patient with a different disease (static encephalopathy of childhood with neurodegeneration in adulthood with _WDR45_ mutation) and the
current patient and PCR-amplified with specific primers (available on request). cDNA was cloned using TA-cloning kit (Takara). The statistical test was calculated by SPSS Statistics version
22.0 (IBM). RESULTS CLINICAL FEATURES Clinical features of the two patients are summarized together with previously described patients in Table 1. Patients 1 and 2 showed similar clinical
features. Both patients were born by cesarean section due to a transient non-reassuring fetal status by fetal heart beat monitoring, and showed small head circumference (31.5 cm (−1.4 S.D.)
in patient 1 and 30.5 cm (−2.7 S.D.) in patient 2) at birth. No perinatal episodes were recognized which could affect their development, but they showed severe growth impairment, hypotonia,
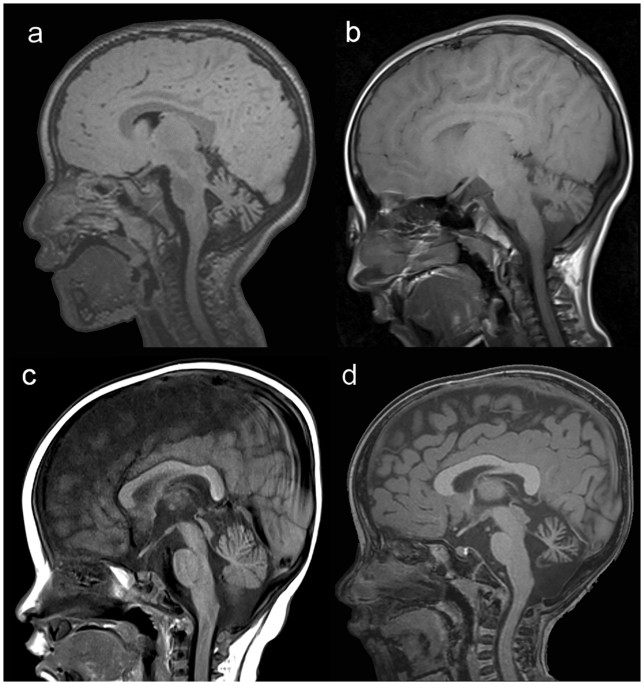
global (especially motor) developmental delay, and pigmentary retinopathy. Both patients showed triangular face and sunken eyes. Brain magnetic resonance imaging (MRI) of patients 1 and 2
showed cerebellar atrophy at 1 year and at 7 months of age, respectively. Patient 1 is a 13-year-old girl who initially showed motor delay at 5 months of age, although she controlled her
head at 3 months. Her hair was thick. She was able to sit and crawl at 1 year and 6 months and 2 years, respectively. She walked with an assisting instrument at 4 years. Her intellectual
development was mild (as she could talk), but her motor skills deteriorated (with loss of the ability to walk at 13 years). She suffered recurrent vomiting and diarrhea since infancy. Brain
MRI studies indicated cerebellar vermis and hemispheres atrophy at 1 year (data not shown, Fig. 1a, b, taken at the age of 3 years and 8 years), but no cerebral atrophy to date. Serum CK was
mildly elevated (430 IU/L) at 9 years of age. Ophthalmologic assessment including funduscopy revealed bilateral retinal pigmentary denaturation, severe hypermetropia, and esotropia. Patient
2 is a 3-year-old girl who showed hypotonia, multiple arthrogryposis, and difficulty taking nutrition orally at birth. Serum CK was 916 IU/L at 7 days of age. Transient arthrogryposis and
CK elevation were exhibited, but gradually improved until complete recovery at 2 years. She showed global developmental delay: head control at 11 months, sitting at 1 year and 8 months, and
pulling herself up and speaking meaningful words at 2 years. She could speak a few words but could not walk at the age of 3 years. Brain MRI showed atrophy of cerebellar vermis and
hemispheres at 7 months (Fig. 1c), and this atrophy had slightly progressed at 2 years of age (Fig. 1d). The ophthalmologic evaluation led to the possible diagnosis of pigmentary retinal
denaturation. GENETIC ANALYSIS Whole-exome sequencing in the patients revealed biallelic _MSTO1_ mutations. Although the probability of being loss-of-function (LoF) intolerant score of
_MSTO1_ is low (0.0418 based on the Exome Aggregation Consortium (ExAC, http://exac.broadinstitute.org/) database), the probability of being LoF intolerant for recessive models score is more
than 0.95 (0.952 based on the ExAC). Segregation of mutations was confirmed by Sanger sequencing of the DNA of the patients and their parents (Fig. 2a; Supplemental Fig. 1). The same
variant (c.836 G > A; p.Arg279His) was found in both families. The results of computational prediction tools for evaluating the c.836 G > A were inconsistent (Supplemental Table 1):
Polyphen-2 (http://genetics.bwh.harvard.edu/pph2/) and MutationTaster (http://www.mutationtaster.org/) indicated that this variant was “possibly damaging” or “pathogenic,” respectively,
whereas SIFT (http://sift.jcvi.org/) indicated that it was “tolerated.” The other mutations were a canonical splice site substitution, c.1099-1 G > A, in patient 1 and a nonsense
mutation, c.79 C > T (p.Gln27*), in patient 2. In the ExAC records, c.836 G > A and c.1099-1 G > A are extremely rare and c.79 C > T is absent (Supplemental Table 1). c.1099-1 G
> A is located in the acceptor site of intron 10 (Fig. 3a). Reverse transcription polymerase chain reaction (RT-PCR) was performed to confirm aberrant splicing. c.1099-1 G > A resulted
in exon 11 being 1 bp shorter than that in wild-type cDNA (Fig. 3a), being predicted to cause early truncation of the protein (p.Val367Trpfs*2) (Fig. 3b). The intensity of signal peaks
after the splicing mutation increased in the presence of cycloheximide, suggesting that mutant mRNA had been subjected to NMD [8] (Supplemental Fig. 2). The pathogenicity classification of
mutations by American College of Medical Genetics and Genomics and the Association for Molecular Pathology (ACMG/AMP) guidelines indicated that c.836 G > A (p.Arg279His) is likely
pathogenic, and that c.79 C > T (p.Gln27*) and c.1099 G > A (p.Val367Trpfs*2) are pathogenic. Detailed ACMG/AMP criteria are described in Supplemental Table 2. DISCUSSION To date, a
total of eight _MSTO1_ mutations have been reported (including the current mutations) in five unrelated patients: five missense mutations (four recessive and one dominant inheritance), one
nonsense mutation (recessive), and two splice site mutations (recessive) [5, 6]. Although various missense variants throughout _MSTO1_ are registered in ExAC (Fig. 2b; Supplemental Table 3),
most recessive missense mutations are clustered within or just after the tubulin-like domain. p.Val8Met and p.Gln27* are located within the segment II tubulin-like domain [9]. Several
mutations in genes involved in mitochondrial fission (_MEN2_, _OPA1_, _DNM1L_, and _MFF_) cause human neurological diseases: Charcot–Marie–Tooth disease type 2 A, optic atrophy 1, infantile
encephalopathy, and Leigh-like encephalopathy, respectively [10,11,12,13]. A previous study indicated that MSTO1 regulated mitochondrial fission and fusion dynamics, and was involved in
mitochondrial morphogenesis and maintenance [6]. It was expected that the diseases described above were caused by the abnormality of mitochondrial fission regulation. In two previous
studies, clinical features associated with recessive mutations were more severe and had an earlier onset than those associated with a dominant mutation [5, 6] (Table 1). We described two
patients with early-onset global developmental delay, motor developmental delay, growth impairment, and cerebellar atrophy without seizures, who had recessive mutations. These clinical
features were also described previously in patients with recessive _MSTO1_ mutations. In addition, cognitive deficiency was only recognized in our patients. Previous studies and this report
indicated that the cerebellum and limb muscles showed more susceptibility to impaired mitochondrial fission rather than the cerebral cortex and cardiac muscle [5, 6]. Mutations of _DNM1L_
and _OPA1_, which are known to be associated with mitochondrial fission, cause different human diseases [11, 13]. Inhibition of _Drp1_ (a mouse ortholog of human _DNM1L_) by transfecting a
dominant negative mutant _Drp1_ disturbs dendritic development in cultured Purkinje cells [11], suggesting that several mitochondrial fission proteins play important roles in cerebellar
development. Haploinsufficiency of _OPA1_ is related to human optic atrophy and the expression of _OPA1_ is most abundant in the retinal ganglion cells [13], indicating that the tissue
susceptibility can be associated with the expression level of genes. _MSTO1_ is expressed widely in various tissues based on BioGPS (http://biogps.org/) and GeneCard (www.genecards.org).
Therefore, _MSTO1_ mutations may lead to not only the disorder of cerebellum and skeletal muscles, but also other organs. Our unrelated patients share a missense mutation (c.836 G > A,
p.Arg279His), together with a truncating mutation: c.79 C > T (p.Gln27*) in patient 1 and c.1099-1 G > A in patient 2. Notably, one individual with homozygous c.836 G > A
(p.Arg279His) is registered in ExAC. This might be suggestive of residual MSTO1 function that is somehow retained by the missense variant (Supplemental Figure 3) [14]. Therefore,
homozygosity for p.Arg279His may occur among the individuals classified as controls (removed patients with severe pediatric disease). p.Arg279His only combined with a protein-truncating
mutation can cause an affected status, which is supported by the lack of individuals with homozygous protein-truncating variants in ExAC. In conclusion, we have described two unrelated
patients with biallelic _MSTO1_ mutations. Our report provides valuable information on the consequences of _MSTO1_ mutations for human phenotypes. REFERENCES * Alston CL, Rocha MC, Lax NZ,
Turnbull DM, Taylor RW. The genetics and pathology of mitochondrial disease. J Pathol. 2017;241:236–50. Article CAS PubMed Google Scholar * Craven L, Alston CL, Taylor RW, Turnbull DM.
Recent advances in mitochondrial disease. Annu Rev Genom Hum Genet. 2017;18:257–75. Article CAS Google Scholar * Phadke R. Myopathology of adult and paediatric mitochondrial diseases. J
Clin Med. 2017;6:E64. * Kimura M, Okano Y. Human Misato regulates mitochondrial distribution and morphology. Exp Cell Res. 2007;313:1393–404. Article CAS PubMed Google Scholar * Gal A,
Balicza P, Weaver D, Naghdi S, Joseph SK, Varnai P, et al. MSTO1 is a cytoplasmic pro-mitochondrial fusion protein, whose mutation induces myopathy and ataxia in humans. EMBO Mol Med.
2017;9:967–84. Article CAS PubMed PubMed Central Google Scholar * Nasca A, Scotton C, Zaharieva I, Neri M, Selvatici R, Magnusson OT, et al. Recessive mutations in MSTO1 cause
mitochondrial dynamics impairment, leading to myopathy and ataxia. Hum Mutat. 2017;38:970–7. Article CAS PubMed PubMed Central Google Scholar * Iwama K, Sasaki M, Hirabayashi S, Ohba C,
Iwabuchi E, Miyatake S, et al. Milder progressive cerebellar atrophy caused by biallelic SEPSECS mutations. J Hum Genet. 2016;61:527–31. Article CAS PubMed Google Scholar * Hug N,
Longman D, Caceres JF. Mechanism and regulation of the nonsense-mediated decay pathway. Nucleic Acids Res. 2016;44:1483–95. Article PubMed PubMed Central Google Scholar * Miklos GL,
Yamamoto M, Burns RG, Maleszka R. An essential cell division gene of _Drosophila_, absent from Saccharomyces, encodes an unusual protein with tubulin-like and myosin-like peptide motifs.
Proc Natl Acad Sci USA. 1997;94:5189–94. Article CAS PubMed PubMed Central Google Scholar * Guillet V, Gueguen N, Cartoni R, Chevrollier A, Desquiret V, Angebault C, et al. Bioenergetic
defect associated with mKATP channel opening in a mouse model carrying a mitofusin 2 mutation. FASEB J. 2011;25:1618–27. Article CAS PubMed Google Scholar * Nasca A, Legati A, Baruffini
E, Nolli C, Moroni I, Ardissone A, et al. Biallelic mutations in DNM1L are associated with a slowly progressive infantile encephalopathy. Hum Mutat. 2016;37:898–903. Article CAS PubMed
PubMed Central Google Scholar * Koch J, Feichtinger RG, Freisinger P, Pies M, Schrodl F, Iuso A, et al. Disturbed mitochondrial and peroxisomal dynamics due to loss of MFF causes
Leigh-like encephalopathy, optic atrophy and peripheral neuropathy. J Med Genet. 2016;53:270–8. Article PubMed Google Scholar * Alexander C, Votruba M, Pesch UE, Thiselton DL, Mayer S,
Moore A, et al. OPA1, encoding a dynamin-related GTPase, is mutated in autosomal dominant optic atrophy linked to chromosome 3q28. Nat Genet. 2000;26:211–5. Article CAS PubMed Google
Scholar * Di Gioia SA, Connors S, Matsunami N, Cannavino J, Rose MF, Gilette NM, et al. A defect in myoblast fusion underlies Carey-Fineman-Ziter syndrome. Nat Commun. 2017;8:16077. Article
PubMed PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS We thank the individuals and their families for their participation in this study. We also thank Nobuko
Watanabe and Mai Sato for technical assistance. We are also thanks Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript. This work was supported by grants from
Research on Measures for Intractable Diseases, Comprehensive Research on Disability Health and Welfare, the Strategic Research Program for Brain Science (SRPBS), the Practical Research
Project for Rare/Intractable Diseases, the Initiative on Rare and Undiagnosed Diseases from the Japan Agency for Medical Research and Development, a Grant-in-Aid for Scientific Research on
Innovative Areas (Transcription Cycle) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan, Grants-in-Aid for Scientific Research (A and B), Grant-in-Aid for
Young Scientists (B), Challenging Exploratory Research from the Japan Society for the Promotion of Science, the fund for Creation of Innovation Centers for Advanced Interdisciplinary
Research Areas Program in the Project for Developing Innovation Systems from the Japan Science and Technology Agency, grants from the Ministry of Health, Labor and Welfare, and the Takeda
Science Foundation. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Human Genetics, Graduate School of Medicine, Yokohama City University, Yokohama, Japan Kazuhiro Iwama, Chihiro
Ohba, Satomi Mitsuhashi, Satoko Miyatake, Atsushi Takata, Noriko Miyake, Takeshi Mizuguchi & Naomichi Matsumoto * Department of Pediatrics, Graduate School of Medicine, Yokohama City
University, Yokohama, Japan Kazuhiro Iwama & Shuichi Ito * Department of Child Neurology, National Center Hospital, National Center of Neurology and Psychiatry, Tokyo, Japan Toru Takaori
& Akihiko Ishiyama * Niigata Prefecture Hamagumi Medical Rehabilitation Center for Disabled Children, Niigata, Japan Ai Fukushima * Department of Pediatrics, Epilepsy Center,
Nishi-Niigata Chuo National Hospital, Niigata, Japan Jun Tohyama * Clinical Genetics Department, Yokohama City University Hospital, Yokohama, Japan Satoko Miyatake & Shuichi Ito *
Department of Biochemistry, Hamamatsu University School of Medicine, Hamamatsu, Japan Hirotomo Saitsu Authors * Kazuhiro Iwama View author publications You can also search for this author
inPubMed Google Scholar * Toru Takaori View author publications You can also search for this author inPubMed Google Scholar * Ai Fukushima View author publications You can also search for
this author inPubMed Google Scholar * Jun Tohyama View author publications You can also search for this author inPubMed Google Scholar * Akihiko Ishiyama View author publications You can
also search for this author inPubMed Google Scholar * Chihiro Ohba View author publications You can also search for this author inPubMed Google Scholar * Satomi Mitsuhashi View author
publications You can also search for this author inPubMed Google Scholar * Satoko Miyatake View author publications You can also search for this author inPubMed Google Scholar * Atsushi
Takata View author publications You can also search for this author inPubMed Google Scholar * Noriko Miyake View author publications You can also search for this author inPubMed Google
Scholar * Shuichi Ito View author publications You can also search for this author inPubMed Google Scholar * Hirotomo Saitsu View author publications You can also search for this author
inPubMed Google Scholar * Takeshi Mizuguchi View author publications You can also search for this author inPubMed Google Scholar * Naomichi Matsumoto View author publications You can also
search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to Naomichi Matsumoto. ETHICS DECLARATIONS CONFLICT OF INTEREST The authors declare that they have no
conflict of interest. ELECTRONIC SUPPLEMENTARY MATERIAL SUPPLEMENTAL FIGURES SUPPLEMENTAL TABLES RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Iwama,
K., Takaori, T., Fukushima, A. _et al._ Novel recessive mutations in _MSTO1_ cause cerebellar atrophy with pigmentary retinopathy. _J Hum Genet_ 63, 263–270 (2018).
https://doi.org/10.1038/s10038-017-0405-8 Download citation * Received: 05 October 2017 * Revised: 04 December 2017 * Accepted: 10 December 2017 * Published: 16 January 2018 * Issue Date:
March 2018 * DOI: https://doi.org/10.1038/s10038-017-0405-8 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative







