- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
This special supplement is an updated compilation of the selected chapters of the State of India’s Newborns Report 2014 (SOIN 2014) released in September 2014.1 The supplement captures the
story of India’s neonatal health initiatives in recent years and sets sights on averting all preventable neonatal deaths. It is an honest effort to share India’s experience in improving
neonatal health with a wide spectrum of national and global stakeholders. These papers highlight the success, and also provide insight to address the gaps as we move forward. The last decade
has been a defining phase in neonatal health and survival in India. Since the launch of the National Rural Health Mission (NRHM) in 2005, newborn healthcare has received unprecedented
attention and resources.2 The country launched several new initiatives to boost maternal–neonatal care under NRHM.2 The Janani Suraksha Yojana (JSY) provides for cash incentive for
childbirth in facilities. The Facility Based Newborn Care (FBNC) aims to build a three-tier system of neonatal care encompassing the primary health centers (PHCs), the community health
centers (CHCs) and the District Hospitals. The Home-based Newborn Care (HBNC) program envisages home visiting by the Accredited Social Health Activists (ASHAs) for neonatal examination,
sickness detection and family counseling. The Navjat Shishu Suraksha Karyakram (NSSK) aims at provision of essential newborn care including resuscitation in facilities at all delivery
points. The Janani Shishu Suraksha Karyakram (JSSK) goes a step further and entitles mothers and infants to free transportation, care, medicines and diagnostics in all public facilities. As
a part of the recently instituted Rashtriya Bal Suraksha Karyakram (RBSK), the focus has been placed on screening infants for selected birth defects and developmental delays. The health
system development has seen a transformational change in these years in increasing access of health services to the poor.3, 4 More than 900 000 village level ASHA workers, 33 000 nurses, 14
000 paramedics, 8000 doctors and 3000 specialists have been inducted. More than 38 300 facilities have been constructed; and over 20 000 ambulances deployed.3 Medical graduate seats have
increased by 55 per cent and postgraduate seats by 75%. More than 500 000 village health and sanitation committees have been formed to catalyze community participation. In a five year span
(2007–2012), over 11 billion USD were spent on NRHM, the core focus of which is reproductive, maternal, neonatal, child and adolescent health.4 Actual public spending together on health
sector as a whole by the federal and state government more than doubled between the X Plan (2002–2007) and XI Plan (2007–2012) periods.4 WHAT DIFFERENCE DID THIS MAKE TO MATERNAL, NEONATAL
AND CHILD HEALTH? Maternal mortality ratio (MMR per 100 000 live births) declined from 254 (2004–2006) to 178 (2010–2012). 5 Under-five mortality rate (U5MR) dropped by 30% from 74 per 1000
live births (2005–2006) to 49 (2013). Infant mortality rate has declined from 58 per 1000 live births in 2005 to 40 in 2013. In the same period neonatal mortality rate (NMR) decreased by
22%, from 37 per 1000 live births to 28, in 2013.1, 6 These are not small achievements. Although we continue to have 0.8 million neonatal deaths each year, the country saved an additional
360 000 neonatal lives in 2012 compared with the year 2000.3 The JSY has ensured that an additional 11 million women are now delivering in government facilities each year with institutional
delivery rate reaching 80%. A nationwide network of FBNC has been established at various levels: 14 163 newborn care corners at the point of child births; 1904 newborn stabilization units
(at sub-district hospitals); 565 special newborn care units for sick and small newborns at district hospitals. More than 0.6 million newborn babies, mostly from poor families, are receiving
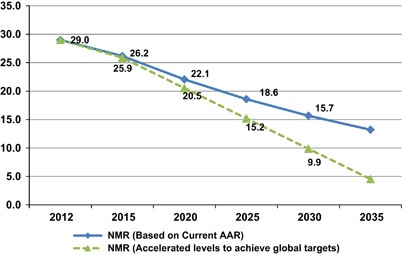
care in these SNCUs in the district hospitals across the nation each year.3 In September 2014, India launched the India Newborn Action Plan (INAP). INAP envisages attainments of single-digit
NMR and still birth rate (SBR) in India by the year 2030 (see Figure 1).3 INAP has been developed in response to the global Every Newborn Action Plan (ENAP) approved by the World Health
Assembly in June 2014.7 ENAP aims to achieve, by 2035, a target of 10 or less newborn deaths (per 1000 live births) and 10 or less stillbirths (per 1000 total births) in all countries. India
aims to achieve these targets by 2030, 5 years in advance of the global timeline.3 The INAP will be implemented within the existing RMNCH+A (Reproductive, Maternal, Newborn and Child
Health+Adolescent) framework, and guided by the principles of integration, equity, gender, quality of care, convergence, accountability and partnerships. INAP envisages six pillars of
intervention packages, impacting stillbirths and newborn health. These include: pre-conception and antenatal care; care during labor and childbirth; immediate newborn care; care of healthy
newborn; care of small and sick newborn; and care beyond newborn survival. Newborns should not only survive, but also thrive and attain the highest developmental potential. This mandates
that beyond survival we track and take care of every child to ensure growth, appropriate nutrition, health and development. Accordingly, the sixth pillar of INAP is ‘Care beyond newborn
survival’. India’s academia and industry need to develop affordable products and solutions for maternal, newborn and child care that are applicable worldwide. Indian researchers need to
explore the poorly understood science of prematurity, fetal growth restriction and brain development. For stillbirths, we need to establish reliable system to measure and classify fetal
deaths in the community and healthcare facilities. Above all, there is a need to undertake major initiatives to accelerate implementation of interventions in an accelerated fashion
(detection and care of sick neonates, scale up of Kangaroo Mother Care) using the best principles of implementation science. INAP commits to strengthen the health system to address critical
gaps in infrastructure; streamline procurement and supply chain mechanisms (to ensure essential commodity security); and supplement availability of skilled human resource (especially in
hard-to-reach areas and for underserved populations). To improve quality of services in public health facilities, the state and district program management capacity shall be enhanced to
deliver evidence-based interventions in an integrated manner across the continuum of care and quality assurance mechanisms. In addition, steps towards good governance—responsiveness,
transparency and accountability of the health system—shall be invigorated. Concerted efforts shall be made at national and state levels to ensure intradepartmental and interdepartmental
convergence and multi-stakeholder partnerships. This would be vital for addressing critical social determinants of maternal and newborn health, such as child marriage, gender inequity,
early/adolescent pregnancy, and frequent and multiple pregnancies. INAP emphasizes the need to address gender discrimination (for example, female feticide) that affects care-seeking for
female infants, children and women. INAP also calls for increased focus on maternal and newborn health for the urban poor, especially by harnessing the potential of the private sector. At
the cusp of the post-MDGs era, 2015 is an exciting year in India’s history—a time for hope and determination for attaining the best possible maternal, neonatal and child health in the
country in near future. REFERENCES * Zodpey S, Paul VK, _State of India’s Newborns 2014_. Public Health Foundation of India, All India Institute of Medical Sciences and Save the Children:
New Delhi, India, 2014. Google Scholar * Ministry of Health and Family Welfare, Government of India _5 Years of Unprecedented Progress Under National Rural Health Mission_. Times of India:
New Delhi, 2014. * Ministry of Health and Family Welfare, Government of India. India Newborn Action Plan. 2014 Available at: http://nrhm.gov.in/india-newborn-action-plan.html. Accessed 18
August 2016. * Planning Commission, Government of India. Twelfth Five Year Plan (2012-2017), volume III: social sectors. 2012.
http://planningcommission.nic.in/plans/planrel/fiveyr/12th/pdf/12fyp_vol3.pdf. Accessed 17 August 2016. * Registrar General of India. Special bulletin on maternal mortality in India
2010-2012. 2013. http://www.censusindia.gov.in/vital_statistics/SRS_Bulletins/MMR_Bulletin-2010-12.pdf. Accessed 17 August 2016. * Registrar General of India. Sample Registration System
Bulletin. 2014. http://www.censusindia.gov.in/vital_statistics/SRS_Bulletin_2014.pdf. Accessed 19 August 2016. * WHO, UNICEF. Every Newborn: An Action Plan To End Preventable Deaths. 2014
https://www.everynewborn.org/Documents/Full-action-plan-EN.pdf. Accessed 18 August 2016. Download references ACKNOWLEDGEMENTS Support for this publication was provided by Save the Children’s
Saving Newborn Lives program. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India V K Paul * Ministry of Health
and Family Welfare, Government of India, New Delhi, India R Kumar * Indian Institute of Public Health Delhi, Public Health Foundation of India, Delhi, India S Zodpey Authors * V K Paul View
author publications You can also search for this author inPubMed Google Scholar * R Kumar View author publications You can also search for this author inPubMed Google Scholar * S Zodpey
View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to S Zodpey. ETHICS DECLARATIONS COMPETING INTERESTS The authors
declare no conflict of interest. RIGHTS AND PERMISSIONS This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third
party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative
Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit
http://creativecommons.org/licenses/by-nc-nd/4.0/ Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Paul, V., Kumar, R. & Zodpey, S. Toward single digit neonatal mortality
rate in India. _J Perinatol_ 36 (Suppl 3), S1–S2 (2016). https://doi.org/10.1038/jp.2016.182 Download citation * Published: 07 December 2016 * Issue Date: December 2016 * DOI:
https://doi.org/10.1038/jp.2016.182 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently
available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative







:max_bytes(150000):strip_icc():focal(119x0:121x2)/tori-spelling-240-13-da9d4c7732454004aed71e77a291f0a8.jpg)