- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT BACKGROUND: Some studies have provided the possibility that adipose tissue may mediate air pollution-induced lung dysfunction. Studies using quantified fat mass data are needed to
understand the biological mechanisms between adipocyte and air pollution in lung function. We aimed to investigate whether abdominal adiposity measured by computed tomography (CT) modifies
the effects of air pollution on lung function in Korean men. METHODS: A total of 1876 men who visited one of two health checkup centers were recruited for this study. Adiposity traits such
as visceral adipose tissue (VAT), subcutaneous adipose tissue (SAT) and total adipose tissue (TAT) areas were measured by CT. We used the annual mean concentrations of ambient air pollutants
including nitrogen dioxide (NO2) and particulate matter with an aerodynamic diameter ⩽10 μm (PM10). RESULTS: Interquartile range (IQR) increase in annual mean concentration of NO2 was
significantly associated with a 2.5% lower forced expiratory volume in 1 s (FEV1) and 2.9% lower forced vital capacity (FVC) (both _P_<0.05). The decrease in lung function was more
strongly associated with adiposity traits than with body mass index. In a stratified analysis of adiposity, compared with subjects with low-VAT area (VAT⩽200 cm2), those with high-VAT area
(VAT>200 cm2) showed a rapid decrease in FEV1 with each IQR increase in PM10 (_β_=–0.0812; 95% confidence interval (CI) =–0.1590, –0.0035) and NO2 (_β_=–0.0979; 95% CI=–0.1611, –0.0346).
In the high-VAT group, each IQR increase in NO2 content was significantly associated with a 10.6% decrease (_β_=–0.1056; 95% CI=–0.1770, –0.0343) in FVC. SAT and TAT areas showed similar
patterns. CONCLUSIONS: We report the first finding that abdominal adiposity intensifies the inverse relationship between air pollution and lung function. You have full access to this article
via your institution. Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS ASSOCIATION BETWEEN LONG-TERM AIR POLLUTION EXPOSURE AND INSULIN RESISTANCE INDEPENDENT OF ABDOMINAL ADIPOSITY IN
KOREAN ADULTS Article Open access 09 November 2022 INTERACTION BETWEEN VISCERAL ADIPOSITY AND AMBIENT AIR POLLUTION ON LDL CHOLESTEROL LEVEL IN KOREAN ADULTS Article 17 November 2020
RELATIONSHIP BETWEEN OBESITY, BODY COMPOSITION, AND PULMONARY FUNCTION AMONG KOREAN ADULTS AGED 40 YEARS AND OLDER Article Open access 27 August 2024 INTRODUCTION Ambient air pollution is
one of the most important global health issues because it increases the risk of and aggravates many diseases such as asthma, lung disease, stroke and certain cancers.1, 2, 3, 4, 5 Air
pollution has been shown to have negative effects on respiratory health, and acute or repeated exposure to air pollution is associated with a reduced lung function.6, 7, 8, 9 A recent
genome-wide interaction study based on the SAPALDIA (Swiss Cohort Study on Air Pollution and Lung Disease in Adults) cohort reported that particulate matter with an aerodynamic diameter ⩽10
μm (PM10) was significantly associated with lung function decline by interacting with certain variants of _CDH13._10 Our previous study also replicated this _CDH13_ gene-by-PM10 interaction
effect on lung function in Korean men.11 _CDH13_ (also known as T-cadherin) is closely related to adiponectin, which is secreted exclusively from fat tissue.10 These findings indicate that
there might be a potential connection between air pollution, fat tissue and lung function. In fact, several plausible hypotheses have been proposed to explain this connection, including the
roles of oxidative stress and inflammation because of their shared mechanisms; that is, both obesity-induced inflammation and oxidative stress are related to excess adipose tissue.12
Increased adipose tissue produces predominantly proinflammatory cytokines including leptin, visfatin, resistin, tumor necrosis factor-α and interleukin-6. Activated reactive oxygen species
produced by accumulated adipose tissue increases systemic oxidative stress. Although previous reports have shown significant synergistic effects of obesity and exposure to ambient air
pollutants such as nitrogen dioxide (NO2) and PM10 content on lung function using an indirect measurement of obesity including body mass index (BMI),6, 13, 14 accurate quantitative
measurement of adipose tissue mass by computed tomography (CT) is needed to understand the plausible mechanisms between adipose tissue and air pollution in lung function. However, to our
knowledge, no studies have investigated whether there is an additive effect of fat accumulation in adipose tissue on the relationship between ambient air pollution and lung function. In
addition, most epidemiological studies regarding negative impacts of air pollution on lung function have focused mainly on children or specific populations such as Europeans, and there are
few studies of these associations in Asian adults. This study was to investigate the chronic effects of ambient air pollutants such as PM10 and NO2 on lung function in Korean men and to
identify whether these effects are mediated by abdominal adiposity in particular visceral adipose tissue (VAT), subcutaneous adipose tissue (SAT) and total adipose tissue (TAT) areas
measured by CT. We provide the first evidence that adiposity may mediate the effects of air pollution on lung function in Asian adults. SUBJECTS AND METHODS SUBJECTS The participants in this
study were recruited at the two health-care centers at Seoul National University Hospital from 2009 to 2014.11 They visited the center to have periodic comprehensive screening health
checkups. During this period, we enrolled a total of 2761 subjects, 885 of whom were excluded because they met the following exclusion criteria: (1) age ⩽40 years; (2) lacking the necessary
phenotypic information such as adiposity-related traits, lung function and smoking status; (3) lacking zip code information for estimating exposure to air pollution; or (4) missing air
pollution values. Therefore, a total of 1876 subjects were included in the final analysis. This study was approved by the institutional review board of the Seoul National University Hospital
Biomedical Research Institute (approval number, H-0911–010–299; C-1511–114–723). ASSESSMENT OF LUNG FUNCTION Pulmonary function was assessed in each subject using a 1022 digital spirometer
(SensorMedics, Anaheim, CA, USA).15 After each measurement, each flow–volume curve was examined to ensure that it satisfied the acceptability and reproducibility criteria, and the same
measurement process was repeated at least three times for forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC) values. The highest absolute values for FVC and FEV1 were
chosen as the outcome variables in this study. ADIPOSITY-RELATED TRAITS ASSESSMENT The details of the methods to measure abdominal adiposity have been described in a previous study.16
Briefly, abdominal adiposity, including VAT, SAT and TAT, was measured using CT scanner (Somatom Sensation 16 CT scanner, Siemens AG, Erlangen, Germany), and the areas of the fat
compartments were estimated with Rapidia 2.8 CT software (Infinitt, Seoul, Korea). To define the visceral obesity group, an optimal cut-off criterion in Korean men (VAT⩾136 cm2) was first
considered. However, we could not observe the significant effect of visceral obesity group. Therefore, we classified into three groups according to VAT level: subjects with low-VAT level
(VAT⩽100 cm2), subjects with moderate VAT level (100 cm2⩽200 cm2) and subjects with high-VAT level (VAT>200 cm2). Similar to VAT, the subjects were categorized into three subgroups
according SAT and TAT level, because of the absence of optimal cut-off criterion in Korean men for SAT or TAT. LIFESTYLE AND ANTHROPOMETRIC VARIABLES To examine the associations between
adiposity, exposure to ambient air pollution and lung function, we collected data about lifestyle factors and anthropometric markers. Health-related behaviors such as smoking status and
physical activity were assessed using a structured questionnaire and classified as categorical variables as follows: cigarette smoking status (current, former or never smoker) and moderate
activity (yes or no). Anthropometric data including height and weight were also measured. ASSESSMENT OF AIR POLLUTION EXPOSURE To assess exposure to ambient air pollution, we obtained the
monitoring data (2009–2014) for 24-h concentrations of ambient PM10 and NO2 from the Ministry of the Environment of Korea (https://www.airkorea.or.kr). These concentrations were measured at
about 300 nationwide monitoring sites in Korea. The annual average concentrations of air pollutants at each monitoring site were calculated to identify the effects of air pollutants on lung
function. Residential zip codes were used to link each subject to the annual average concentrations from the nearest monitoring site. STATISTICAL ANALYSIS Correlation coefficients between
air pollutants and adiposity measures were estimated using Pearson’s correlational analysis. Multiple linear regression analysis was performed to evaluate the associations between ambient
air pollution, adiposity traits and lung function. To identify the effects of adiposity traits on the relationship between air pollution and lung function, we performed a stratified analysis
using the cut-off for the definition of high-adiposity group for each adiposity trait. The results are presented as beta coefficients and 95% confidence intervals (CIs) for lung function
after adjustment for covariates such as the site of recruitment, age,2 height, BMI, smoking status (never, past or current), pack years and moderate activity (yes or no). These estimates
were converted by scale to the interquartile range (IQR) for each pollutant (9.2 μg m−3 for PM10 and 13.9 ppb for NO2). All analyses were implemented in SAS 9.3 (SAS Institute, Cary, NC,
USA). RESULTS The detailed characteristics of the study subjects are shown in Table 1. A total of 1876 subjects (recruitment site A, _n_=1405; recruitment site B, _n_=471) were included in
the final association analyses. All subjects were men, and most were aged 50–60 years. The mean SAT area (139.8±53.1 cm2) was slightly higher than the VAT area (131.4±53.6 cm2). All
adiposity-related traits were significantly intercorrelated (_P_<0.001), and the correlation between VAT and TAT areas was the strongest of these correlations (_r_=0.880) (Supplementary
Material; Supplementary Table S1). The percentages of former and current smokers were 42.4% (_n_=796) and 32.3% (_n_=605), respectively. The mean FEV1 and FVC were 3.3±0.5 l and 4.1±0.6 l.
The median PM10 and NO2 concentrations were 49.0 μg m−3 and 31.5 ppb, respectively, and their IQRs were 9.2 μg m−3 and 13.9 ppb, respectively. There was a significant positive correlation
between PM10 and NO2 values (_r_=0.430, _P_<0.001) (Supplementary Material; Supplementary Table S1). The concentrations of PM10 and NO2 in each subgroup of VAT, SAT and TAT were also
demonstrated in Supplementary Table S2. There was no significant difference in air pollutant concentrations among the subgroups (all _P_>0.05) (Supplementary Material; Supplementary Table
S2). In addition, we have investigated the associations of moderate activity and smoking status with lung function. As a result, smoking status and pack years were associated with decreased
FEV1, although no significant association between smoking status and FVC was observed. However, moderate activity was not significantly associated with FEV1 and FVC (data not shown). Table
2 shows the results of the analysis of the associations between air pollution or adiposity-related traits and lung function including FEV1 and FVC. NO2 concentration was significantly
associated with FEV1 (_P_=0.0131); there was a 2.5% decrease in FEV1 (95% CI=–4.6, –0.5%) with IQR (13.9 ppb) increase in NO2 concentration. Similarly, FVC was significantly associated with
NO2 concentration (_P_=0.0102); there was a 2.9% decrease in FVC (95% CI=–5.1, –0.7%) for IQR (13.9 ppb) increase in NO2 concentration. However, PM10 was not significantly associated with a
reduction in FEV1 or FVC (both _P_>0.05). Analysis of the associations between adiposity-related traits and lung function showed that BMI was not significantly associated with FEV1 or FVC
(both _P_>0.05). However, overall obesity, defined as a BMI⩾25 kg m−2, was significantly associated with FVC (_P_=0.0230). All abdominal adiposity traits such as VAT, SAT and TAT were
significantly associated with both FEV1 and FVC (all _P_<0.0001). Compared with BMI, the adiposity variables quantified using CT, including VAT area, were more strongly related to FEV1
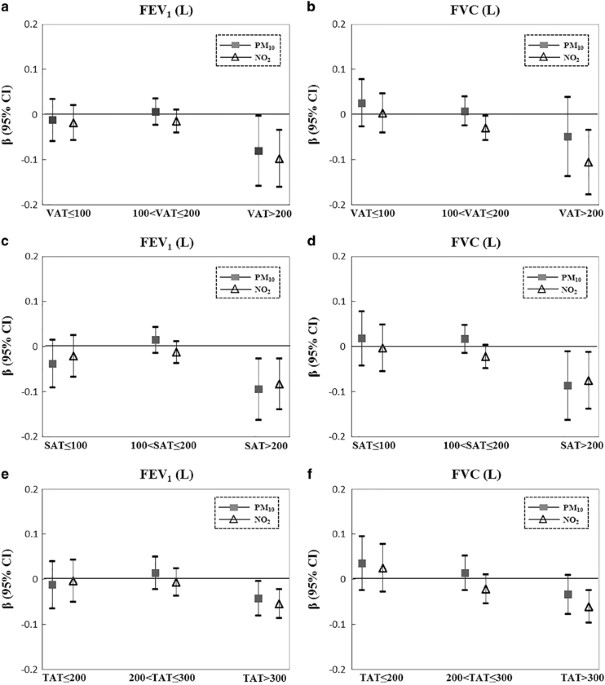
and FVC. To examine the effects of air pollution on lung function according to the degree of adiposity, we performed subgroup analysis by classifying the adiposity traits VAT, SAT and TAT
into three levels (Figure 1). The effects of air pollutants on FEV1 and FVC were much greater in the high-fat group with a VAT>200 cm2. Similar to VAT, the negative association between
air pollution and lung function was stronger in the high-fat group with an SAT area >200 cm2 than in the group with an SAT area⩽200 cm2. For TAT area, the negative associations between
air pollution, and FEV1 and FVC were strongest in the high-fat group with a TAT area >300 cm2. The negative association between TAT and FEV1 was smaller in the moderate fat group than in
the low- and high-fat groups, whereas the relationship between TAT and FVC was smaller in the low-fat group than in the other two groups. Table 3 shows the results of the regression analysis
in the low- and high-adiposity groups with cut-off points of 200, 200 and 300 cm2 for VAT, SAT and TAT areas, respectively. Similar to the results for obesity classified by BMI
(Supplementary Material; Supplementary Table S3), the effects of air pollution on lung function were much stronger in the high- than in the low-adiposity group. In the low-adiposity group,
none of the air pollutants showed significant effects on FEV1, whereas in the high-adiposity group, PM10 and NO2 concentrations were significantly associated with decreased FEV1 (both
_P_<0.05). In the high-VAT group (VAT area >200 cm2), FEV1 decreased 8.1% (_β_=–0.0812; 95% CI=–0.1590, –0.0035) and 9.8% (_β_=–0.0979; 95% CI=–0.1611, –0.0346) for each IQR increase
in PM10 and NO2, respectively. The high-SAT group (SAT area >200 cm2) showed a pattern similar to the high-VAT group. In the high-TAT group (TAT area >300 cm2), FEV1 decreased 4.3%
(_β_=–0.0426; 95% CI=–0.0810, –0.0042) and 5.5% (_β_=–0.0545; 95% CI=–0.0864, –0.0226) for each IQR increase in PM10 and NO2 concentration, respectively. In the high-adiposity group, air
pollution was also associated with decreased FVC. In the high-VAT group, FVC decreased 10.6% (_β_=–0.1056; 95% CI=–0.1770, –0.0343) for each IQR increase in NO2 concentration. PM10
(_P_=0.0262) and NO2 (_P_=0.0198) concentrations were also significantly associated with a decrease in FVC in the high-SAT group; FVC decreased 8.7 (_β_=–0.0868; 95% CI= –0.1629, –0.0108)
and 7.5% (_β_=–0.0752; 95% CI=–0.1379, –0.0125) for each IQR increase in PM10 and NO2 concentration. Overall, the effects of NO2 were greater than those of PM10 when analyzed according to
VAT area, whereas the effects of PM10 were greater than those of NO2 when analyzed according to SAT area. In the high-TAT group (TAT area >300 cm2), FVC decreased 6.1% (_β_=–0.0607; 95%
CI=–0.0967, –0.0248) for IQR increase in NO2 concentration. DISCUSSION This study investigated the associations between exposure to ambient air pollution, as shown by the PM10 and NO2
levels, and lung function in Korean men, and whether these associations are modified by adiposity level. We observed a significant negative relationship between annual average concentration
of NO2 and lung function (_P_<0.05), showing 2.5% (_β_=–0.0254; 95% CI=–0.0455, –0.0053) FEV1 and 2.9% (_β_=–0.0292; 95% CI=–0.0514, –0.0070) FVC decrease per IQR (13.9 ppb) increase in
the NO2 concentration. Interestingly, in the subgroup analyses, the associations of PM10 and NO2 concentrations were much stronger in the high- than in the low-adiposity group. In the
high-VAT group, each IQR increase in PM10 and NO2 concentration was associated with a decrease in FEV1 (_β_ (95% CI) for PM10=–0.0812 (–0.1590, –0.0035) and _β_ (95% CI) for NO2=–0.0979
(–0.1611, –0.0346)), compared with the low-VAT group. In the high-VAT group, FVC was also negatively associated with NO2 concentration; there was a 10.6% (_β_=–0.1056; 95% CI=–0.1770,
–0.0343) decrease in FVC for increase in IQR. This pattern was similar in the subgroups classified according to subcutaneous and total abdominal fat. Considering the negative impacts of air
pollution on health, the increase in air pollution in South Korea has become an inevitable social issue. A recent report documented that Korea is expected to experience the greatest increase
in premature deaths and economic damage caused by air pollution among the Organization for Economic Cooperation and Development (OECD) countries, if Korea's air pollution continues its
current trend by 2060.17 The median values of PM10 (μg m−3) and NO2 (ppb) concentrations estimated in our study were 49 and 31.5, respectively. In particular, the level of PM10
concentration is considerably higher compared to other European studies.6, 18 This was even higher than the measured PM10 concentration near the busy road in Germany.19 However, when
compared to the average concentrations of 31 major provincial cities in China (average concentration for PM10 in 2014 =109.8 μg m−3), the level of PM10 concentration in our study was much
lower.20 Epidemiological studies have reported significant associations between exposure to air pollutants and a decreased lung function in adults.18, 19, 21 In 1997, significant
relationships between the annual mean levels of air pollutants such as PM10, NO2 and SO2, and lung function were observed in adults aged 18–60 years residing in Switzerland.21 In 2005,
Schikowski _et al._19 found that chronic exposure to PM10 and NO2 was related with increased risk of chronic obstructive pulmonary disease in 55-year-old women in Germany. Forbes _et al._18
reported a significant association between chronic exposure to air pollution and FEV1 in a large English population, and reported a 3% decline in FEV1 per 10 μg m−3 increase in PM10
concentration. However, these effects of air pollution on lung function in adults were found in specific European populations. More recent evidence has suggested an additive effect of air
pollution and obesity on lung function decline.6, 13, 14 In 2013, Schikowski _et al._14 investigated whether the effect of improved air quality on lung function is modified by obesity
status. They reported significant interactions between a change in PM10 concentration and BMI; after a decrease in PM10 concentration, the annual rates of decline in lung function were
smaller in the groups with low or normal BMI compared with those defined as obese according to BMI. Dong _et al._13 found that the risks for asthma and respiratory symptoms including cough
were greater in obese children than in normal weight children. In particular, the interaction effects with obesity on cough and phlegm were significant for NO2 and PM10 concentrations. One
European adult study based on the multicenter cohorts in the European Study of Cohorts for Air Pollution Effects (ESCAPE) identified a larger effect of exposure to air pollution including
PM10 and NO2 on lung function in the obese group.6 To date, the mechanisms underlying the synergistic effects of obesity on the link between ambient air pollution and lung function remain
unclear, but several possible physiological mechanisms linked to adipocyte have been suggested. One plausible mechanism is the inflammatory pathway. Exposure to ambient air pollution
promotes airway inflammation, which can lead to a decline in lung function and/or lung injury.22 Similarly, a significant correlation between obesity and systemic inflammation has been
reported.23 Adipokines such as leptin and adiponectin, which mediate the inflammatory response, are produced mainly in adipose tissue. Inflammatory cytokines including tumor necrosis
factor-α and interleukin-6 are also released by adipocytes. These molecules are directly linked to the inflammatory process. In addition, macrophage migration inhibitory factor, a
proinflammatory protein, is known to be a crucial factor in inflammation of chronic adipose tissue.24 Immune cells including macrophages can also infiltrate adipose tissue. The macrophages
within adipose tissue not only contribute to the production of inflammatory cytokines, but also lead to increased local inflammation.25 Both air pollution and high adiposity are closely
related to increased inflammation, and the synergistic effect of air pollution and adiposity in the high-fat group may be explained by the combined effects of adipose tissue and ambient air
pollution on airway and/or systemic inflammation. Another possible explanation is that air pollution and high adiposity can both increase oxidative stress.12, 26, 27 Many components of
ambient air pollutants cause lung damage through oxidative stress, either by acting directly on reactive oxygen species production or by the indirect induction of local inflammation.28
Accumulated adipose tissue also promotes the production of proinflammatory adipokines, which trigger the production of reactive oxygen species.26 Oxidative stress is significantly associated
with the decline in lung function.29, 30, 31 These plausible hypotheses are supported by present findings in adipose tissue as well as the _CDH13_ gene-by-PM10 interaction effect identified
previously.10, 11 Most studies have primarily focused on short-term or acute effects in a restricted region or a specific population, particularly children. The present study showed
significant associations between abdominal adipose tissue, as well as the negative effects of air pollution on FEV1 and FVC using nationwide data in Korean adults. To our knowledge, we have
shown for the first time that high adiposity strengthens an inverse relationship between air pollution and lung function in Asian men. However, our study does have some limitations. First,
the study design was cross sectional, which means that no causal inferences can be made about the observed effects of adiposity on the relationship between air pollution and lung function.
Second, we did not measure the exposure time to ambient air pollutants in individuals. CONCLUSION Our study identified a synergistic effect of adiposity on the relationship between prolonged
exposure to air pollution and FEV1, and FVC decreases in Asian men. Our findings provide the first evidence that accumulated abdominal fat intensifies the adverse effects of air pollutants
on lung function. REFERENCES * Boffetta P, Nyberg F . Contribution of environmental factors to cancer risk. _Brit Med Bull_ 2003; 68: 71–94. Article CAS Google Scholar * Guarnieri M,
Balmes JR . Outdoor air pollution and asthma. _Lancet_ 2014; 383: 1581–1592. Article CAS Google Scholar * Hong YC, Lee JT, Kim H, Kwon HJ . Air pollution - a new risk factor in ischemic
stroke mortality. _Stroke_ 2002; 33: 2165–2169. Article CAS Google Scholar * Ko FWS, Hui DSC . Outdoor air pollution: impact on chronic obstructive pulmonary disease patients. _Curr Opin
Pulm Med_ 2009; 15: 150–157. Article CAS Google Scholar * Leikauf GD . Hazardous air pollutants and asthma. _Environ Health Perspect_ 2002; 110 (Suppl 4): 505–526. Article CAS Google
Scholar * Adam M, Schikowski T, Carsin AE, Cai YT, Jacquemin B, Sanchez M _et al_. Adult lung function and long-term air pollution exposure. ESCAPE: a multicentre cohort study and
meta-analysis. _Eur Respir J_ 2015; 45: 38–50. Article CAS Google Scholar * Gehring U, Gruzieva O, Agius RM, Beelen R, Custovic A, Cyrys J _et al_. Air pollution exposure and lung
function in children: the ESCAPE Project. _Environ Health Perspect_ 2013; 121: 1357–1364. Article Google Scholar * Min JY, Min KB, Cho S, Paek D . Lag effect of particulate air pollution
on lung function in children. _Pediatr Pulmonol_ 2008; 43: 476–480. Article Google Scholar * Sunyer J . Lung function effects of chronic exposure to air pollution. _Thorax_ 2009; 64:
645–646. Article Google Scholar * Imboden M, Kumar A, Curjuric I, Adam M, Thun GA, Haun M _et al_. Modification of the association between PM10 and lung function decline by cadherin 13
polymorphisms in the SAPALDIA Cohort: a genome-wide interaction analysis. _Environ Health Perspect_ 2015; 123: 72–79. Article CAS Google Scholar * Kim HJ, Min JY, Min KB, Seo YS, Sung J,
Yun JM _et al_. _CDH1_3 gene-by-PM10 interaction effect on lung function decline in Korean men. _Chemosphere_ 2016; 168: 583–589. Article Google Scholar * Fernandez-Sanchez A,
Madrigal-Santillan E, Bautista M, Esquivel-Soto J, Morales-Gonzalez A, Esquivel-Chirino C _et al_. Inflammation, oxidative stress, and obesity. _Int J Mol Sci_ 2011; 12: 3117–3132. Article
CAS Google Scholar * Dong GH, Qian Z, Liu MM, Wang D, Ren WH, Fu Q _et al_. Obesity enhanced respiratory health effects of ambient air pollution in Chinese children: the seven northeastern
cities study. _Int J Obes_ 2013; 37: 94–100. Article CAS Google Scholar * Schikowski T, Schaffner E, Meier F, Phuleria HC, Vierkotter A, Schindler C _et al_. Improved air quality and
attenuated lung function decline: modification by obesity in the SAPALDIA cohort. _Environ Health Perspect_ 2013; 121: 1034–1039. Article Google Scholar * American Thoracic Society .
Standardization of Spirometry, 1994 Update. American Thoracic Society. _Am J Respir Crit Care Med_ 1995; 152: 1107–1136. Article Google Scholar * Kim HJ, Park JH, Lee S, Son HY, Hwang J,
Chae J _et al_. A common variant of NGEF is associated with abdominal visceral fat in Korean men. _PLoS One_ 2015; 10: e0137564. Article Google Scholar * OECD. The Economic Consequences of
Outdoor Air Pollution. Published 9 June 2016. Available at:
https://www.oecd.org/environment/indicators-modelling-outlooks/Policy-Highlights-Economic-consequences-of-outdoor-air-pollution-web.pdf. * Forbes LJ, Kapetanakis V, Rudnicka AR, Cook DG,
Bush T, Stedman JR _et al_. Chronic exposure to outdoor air pollution and lung function in adults. _Thorax_ 2009; 64: 657–663. Article CAS Google Scholar * Schikowski T, Sugiri D, Ranft
U, Gehring U, Heinrich J, Wichmann HE _et al_. Long-term air pollution exposure and living close to busy roads are associated with COPD in women. _Respir Res_ 2005; 6: 152. Article Google
Scholar * He J, Gong S, Yu Y, Yu L, Wu L, Mao H _et al_. Air pollution characteristics and their relation to meteorological conditions during 2014-2015 in major Chinese cities. _Environ
Pollut_ 2017; 223: 484–496. Article CAS Google Scholar * Ackermann-Liebrich U, Leuenberger P, Schwartz J, Schindler C, Monn C, Bolognini G _et al_. Lung function and long term exposure to
air pollutants in Switzerland. Study on Air Pollution and Lung Diseases in Adults (SAPALDIA) Team. _Am J Respir Crit Care Med_ 1997; 155: 122–129. Article CAS Google Scholar * Esposito
S, Tenconi R, Lelii M, Preti V, Nazzari E, Consolo S _et al_. Possible molecular mechanisms linking air pollution and asthma in children. _BMC Pulm Med_ 2014; 14: 31. Article Google Scholar
* Mancuso P . Obesity and lung inflammation. _J Appl Physiol (1985)_ 2010; 108: 722–728. Article Google Scholar * Kim BS, Rongisch R, Hager S, Grieb G, Nourbakhsh M, Rennekampff HO _et
al_. Macrophage migration inhibitory factor in acute adipose tissue inflammation. _PLoS One_ 2015; 10: e0137366. Article Google Scholar * Surmi BK, Hasty AH . Macrophage infiltration into
adipose tissue: initiation, propagation and remodeling. _Future Lipidol_ 2008; 3: 545–556. Article CAS Google Scholar * Marseglia L, Manti S, D'Angelo G, Nicotera A, Parisi E, Di
Rosa G _et al_. Oxidative stress in obesity: a critical component in human diseases. _Int J Mol Sci_ 2015; 16: 378–400. Article Google Scholar * Yang W, Omaye ST . Air pollutants,
oxidative stress and human health. _Mutat Res_ 2009; 674: 45–54. Article CAS Google Scholar * Ghio AJ, Carraway MS, Madden MC . Composition of air pollution particles and oxidative stress
in cells, tissues, and living systems. _J Toxicol Environ Health B Crit Rev_ 2012; 15: 1–21. Article CAS Google Scholar * Ben Moussa S, Sfaxi I, Tabka Z, Ben Saad H, Rouatbi S .
Oxidative stress and lung function profiles of male smokers free from COPD compared to those with COPD: a case-control study. _Libyan J Med_ 2014; 9: 23873. Article Google Scholar *
Ochs-Balcom HM, Grant BJ, Muti P, Sempos CT, Freudenheim JL, Browne RW _et al_. Oxidative stress and pulmonary function in the general population. _Am J Epidemiol_ 2005; 162: 1137–1145.
Article Google Scholar * Waseem SMA, Hussain M, Islam N . Oxidative stress in mild and moderate COPD: assessment of oxidant anti-oxidant imbalance. _Biomed Res_ 2014; 25: 115–119. CAS
Google Scholar Download references ACKNOWLEDGEMENTS This research was supported by the Basic Science Research Program through the National Research Foundation of Korea funded by the
Ministry of Education, Science and Technology (grant number 2015R1D1A1A01057619, 2015R1A1A3A04000923 and 2015R1D1A1A01059048). This work was supported by the National Research Foundation of
Korea (NRF) grant funded by the Korea government (MSIP) (No. 2012R1A5A2A44671346). AUTHOR INFORMATION Author notes * H-J Kim and J-H Park: These two authors contributed equally to this work.
* J-I Kim and B Cho: These two authors contributed equally to this work. AUTHORS AND AFFILIATIONS * Institute of Health and Environment, Seoul National University, Seoul, Korea H-J Kim, J-Y
Min & Y-S Seo * Department of Family Medicine, Seoul National University Hospital, Seoul, Korea J-H Park, J M Yun, H Kwon & B Cho * Department of Family Medicine, Seoul National
University College of Medicine, Seoul, Korea J-H Park & B Cho * Department of Preventive Medicine, Seoul National University College of Medicine, Seoul, Korea K-B Min * Department of
Biochemistry and Molecular Biology, Seoul National University College of Medicine, Seoul, Korea J-I Kim * Department of Biomedical Sciences, Seoul National University Graduate School, Seoul,
Korea J-I Kim Authors * H-J Kim View author publications You can also search for this author inPubMed Google Scholar * J-H Park View author publications You can also search for this author
inPubMed Google Scholar * J-Y Min View author publications You can also search for this author inPubMed Google Scholar * K-B Min View author publications You can also search for this author
inPubMed Google Scholar * Y-S Seo View author publications You can also search for this author inPubMed Google Scholar * J M Yun View author publications You can also search for this author
inPubMed Google Scholar * H Kwon View author publications You can also search for this author inPubMed Google Scholar * J-I Kim View author publications You can also search for this author
inPubMed Google Scholar * B Cho View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHORS Correspondence to J-I Kim or B Cho. ETHICS
DECLARATIONS COMPETING INTERESTS The authors declare no conflict of interest. ADDITIONAL INFORMATION Supplementary Information accompanies this paper on International Journal of Obesity
website SUPPLEMENTARY INFORMATION SUPPLEMENTARY MATERIAL (DOCX 26 KB) RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Kim, HJ., Park, JH., Min, JY. _et
al._ Abdominal adiposity intensifies the negative effects of ambient air pollution on lung function in Korean men. _Int J Obes_ 41, 1218–1223 (2017). https://doi.org/10.1038/ijo.2017.97
Download citation * Received: 12 December 2016 * Revised: 24 February 2017 * Accepted: 14 March 2017 * Published: 25 April 2017 * Issue Date: August 2017 * DOI:
https://doi.org/10.1038/ijo.2017.97 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently
available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative