- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT _AIM_ The aim of this study is to evaluate long-term efficacy of intravitreal injections of aflibercept as primary treatment for subfoveal/juxtafoveal myopic choroidal
neovascularisation (CNV). _METHODS_ Thirty-eight treatment-naive eyes of thirty-eight patients with subfoveal/juxtafoveal myopic CNV received initial intravitreal aflibercept injections and
were followed for at least 18 months. Aflibercept was applied again for persistent or recurrent CNV, as required. Statistical analysis was carried out using SPSS. _RESULTS_ Mean patient age
was 45.8 years, and mean eye refractive error was −7.79 D. For the total patient group (_n_=38 eyes), mean logMAR best-corrected visual acuity (BCVA) significantly improved from 0.69 at
baseline to 0.15 at 18 months (_P_<0.01). Over half of the treated eyes obtained resolution with one aflibercept injection. Patients were also grouped according to age, as <50 years
(_n_=20 eyes) and ≥50 years (_n_=18 eyes). Mean BCVA improvement was significantly greater in eyes of the younger myopic CNV group, compared with those of ≥50 years (0.21 _vs_ 0.35;
_P_<0.05). The mean number of aflibercept injections was 1.8 for the <50 years myopic CNV group, and 3.6 for the ≥50 years myopic CNV group (_P_<0.001). Correlation between
spherical equivalent refraction and final visual acuity reached statistical significance only for the <50 years myopic CNV group (_P_<0.001; Levene’s correlation). _CONCLUSIONS_
Intravitreal aflibercept provides long-term visual acuity improvement in myopic CNV. The <50 years old myopic CNV group had significantly fewer injections, with greater visual acuity
improvement. Intravitreal aflibercept in myopic CNV does not require the three-injection loading phase used for aflibercept treatment of neovascular age-related macular degeneration. SIMILAR
CONTENT BEING VIEWED BY OTHERS CHOROIDAL REMODELING FOLLOWING DIFFERENT ANTI-VEGF THERAPIES IN NEOVASCULAR AMD Article Open access 22 January 2024 LONG-TERM OUTCOMES OF RANIBIZUMAB VS.
AFLIBERCEPT FOR NEOVASCULAR AGE-RELATED MACULAR DEGENERATION AND POLYPOIDAL CHOROIDAL VASCULOPATHY Article Open access 16 July 2021 RETINAL AND CHOROIDAL EFFICACY OF SWITCHING TREATMENT TO
FARICIMAB IN RECALCITRANT NEOVASCULAR AGE RELATED MACULAR DEGENERATION Article Open access 26 April 2024 INTRODUCTION Pathological myopia is one of the leading causes of visual impairment
worldwide, and choroidal neovascularisation (CNV) is one of the most sight-threatening complications in patients affected with pathological myopia.1 The estimated risk for development of CNV
from pathological myopia has been estimated as 4–10%, and the natural course of subfoveal CNV is generally poor.2 Indeed, a large proportion of patients with myopia will have progression of
myopic maculopathy, and a consequent visual loss. Photodynamic therapy (PDT) has been one of the treatments of choice for myopic CNV over the past decade, and several studies have
demonstrated that compared with placebo, PDT can reduce the risk of visual loss.3, 4 However, patients treated with PDT do not gain better mean visual acuity, and PDT does not prevent visual
loss for longer than 2 years.5 In recent years, the short-term efficacy of intravitreal anti-vascular endothelial growth factor (VEGF) agents has been shown for the arrest of myopic CNV,
which have included bevacizumab6 and ranibizumab.7 The majority of the studies with these agents have reported significant mean visual acuity improvements at 12 months. Other more recent
studies have shown longer-term visual results for treatment of myopic CNV for up to 2 years after intravitreal injections of bevacizumab.8, 9 However, some discrepancies have been detected
for such longer-term visual outcomes; indeed, it has been demonstrated that the initial visual gain with bevacizumab is not significantly maintained at 2 years.9, 10 This appears to be
because patients with myopic CNV who were treated with this anti-VEGF agent had undergone prior treatments, with some of these treatments being for non-subfoveal CNV. The use of aflibercept
(Eylea; Regeneron, Tarrytown, NY, USA; Bayer, Basel, Switzerland) has been introduced more recently, which is a recombinant fusion protein that binds all isoforms of VEGF, and also placental
growth factor.11 Aflibercept recently obtained US Food and Drug Administration approval for the treatment of neovascular age-related macular degeneration (AMD).12 With treatment of
aflibercept every 2 months following 3-monthly loading doses, it was shown to be non-inferior to monthly injections of ranibizumab, in terms of patients who maintained or improved their
vision at 12 months. These aflibercept benefits were also maintained to 2 years.12 However, there remain discrepancies in the literature about the efficacy of ranibizumab and bevacizumab for
maintenance of good visual acuity over 2 years of treatment of patients with myopic CNV. Thus, considering also the relative lack of data for aflibercept treatment for these patients, we
investigated the long-term visual outcome of patients with myopic CNV treated with aflibercept. MATERIALS AND METHODS This was a retrospective study of consecutive patients with
subfoveal/juxtafoveal CNV secondary to pathological myopia who received intravitreal aflibercept injections. The treatments were carried out in the Department of Ophthalmology, Polytechnic
University of Marche, Ancona (Italy), and informed consent was obtained from all of the patients before treatment. The inclusion criteria included: treatment-naive patients with follow-up of
≥18 months; myopia with a spherical equivalent refractive error of ≥–5 D; active CNV, as documented by fluorescein angiography and SD-OCT (spectral-domain optical coherence tomography);
subfoveal–juxtafoveal CNV; and best-corrected visual acuity (BCVA) 20/800 or better. The exclusion criteria included: prior treatments for CNV, including PDT and thermal laser
photocoagulation; history of intraocular surgery; extrafoveal CNV; CNV from ocular pathology other than pathological myopia, such as AMD, choroiditis, angioid streaks, and trauma; and
hereditary disease in the studied and fellow eye. At baseline and at all subsequent visits, complete ophthalmic examinations were carried out, which included Snellen BCVA (converted to the
logarithm of the minimum angle of resolution; logMAR), slit-lamp biomicroscopy, tonometry, fundus examination, and fluorescein angiography. Fundus photography and SD-OCT (Topcon America,
Paramus, NJ, USA; Heidelberg Engineering Inc., Dossenheim, Germany) were performed at baseline, and at 1 week and 1, 2, 3, 6, 12, and 18 months after aflibercept injection. Intravitreal
injections of aflibercept 2 mg were carried out using a 30-gauge needle, at 4 mm from the limbus and under aseptic conditions. Retreatment with aflibercept was performed based on the
presence of active leakage on fluorescein angiography, persistent subretinal fluid on SD-OCT, or new haemorrhage, with minimum 3-monthly retreatments maintained. Statistical analysis was
carried out using SPSS (Version 17.0; SPSS Inc., Chicago, IL, USA). The patients were analysed according to both the total patient group and the age groups of <50 years _vs_ ≥50 years.
Paired _t_-tests were performed to evaluate the effects of the post-treatment visual outcome _vs_ baseline (pre-treatment). The differences in the visual outcomes between the two age groups
were compared using two-sample _t_-tests. Linear regression was performed to determine the effects on visual outcome of baseline BCVA, age, spherical equivalent, and number of injections. A
P-value of <0.05 was considered as statistically significant. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were
followed during this study. RESULTS In all, 38 eyes from 38 patients (24 women and 14 men) were included in the study, and the baseline and clinical characteristics of these patients are
given in Table 1. For the total patient group, the baseline mean age (±standard deviation [SD]) was 45.8 years (±20.5 years; range, 22–79 years). The CNV was seen for 30 right eyes (79%) and
8 left eyes (21%). The baseline mean spherical equivalent refractive index was −7.79 D (±3.75 SD; range, −5.00 to −12.50). The mean follow-up time was 21±1.9 months. For the total patient
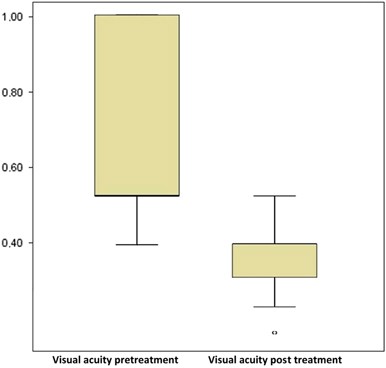
group, the mean BCVA (±SD) improved significantly, from 0.69±0.30 logMAR at baseline to 0.15±0.09 logMAR at 18 months (_P_<0.001) (Figure 1). The mean central foveal thickness decreased
significantly from 276 _μ_m at baseline to 215 _μ_m at 18 months (_P_<0.001) (Table 2). Paired _t_-tests also demonstrated significant improvement in BCVA compared with baseline at 1, 3,
6, 12, and 18 months (_P_<0.001). The greatest improvements were seen within the first 3 months of the initial aflibercept injection, and the BCVA remained stable thereafter. Overall, 55%
(21/38) of the patients achieved resolution of their myopic CNV with a single aflibercept injection. Thus, 19 of the 38 patients (50%) received >1 aflibercept injection, with a total of
79 aflibercept injections given to the 18 months of follow-up (ie, mean, 2.1 aflibercept injections/patient). In detail, over the 18 months of follow-up, 50% of patients received one
injection, 18.4% received two injections, 10.5% received three injections, 15.8% received four injections, and 5.3% received five injections. The further analysis provided 20 eyes for
patients aged <50 years, and 18 eyes for those aged ≥50 years. The mean number of aflibercept injections was 1.5 for the <50 years myopic CNV group, and 2.7 for the ≥50 years myopic
CNV group (_P_ <0.001). Indeed, 60% (12/20) of the treated eyes of the patients <50 years old obtained resolution with just one injection, which was significantly greater than that
seen for the treated eyes of the patients ≥50 years old (60 _vs_ 49%, respectively; _P_<0.05). The mean BCVA improvement was greater in the younger group (<50 years) compared with the
≥50 years (0.64 _vs_ 0.38, respectively; _P_<0.05) (Figure 2). In the 18 months of follow-up, the <50 year patients showed significantly better BCVA improvement than those of ≥50 years
(0.21±0.12 _vs_ 0.35±0.12, respectively; _P_<0.05). In the comparison of spherical equivalent refraction between the patients of <50 _vs_ ≥50 years, at baseline the young patients
were more myopic than the old patients (−9.9 _vs_ −5.5), although this difference did not reach statistical significance. With stratification by age, the correlation between the spherical
equivalent refraction and the final visual acuity showed significance only for the patients of <50 years (_P_<0.001; Levene’s correlation) (Figure 3), as the correlation lost
significance for the patients of ≥50 years. This suggests that spherical equivalent refraction is also predictive of the final visual acuity, and that higher myopia relates to worse visual
acuity in young patients. In the linear regression analysis of the total patient group, after adjusting for age, spherical equivalent refraction, and number of injections, baseline BCVA was
the most predictive factor for the visual outcome (_P_<0.001). Baseline spherical equivalent refraction did not correlate with initial and final BCVA (_P_>0.05; Levene’s correlation).
No relevant ocular or systemic complications were detected. DISCUSSION Several treatments have been proposed for myopic CNV, such as laser photocoagulation, surgical removal of CNV, macular
translocation, and PDT without and with intravitreal triamcinolone acetonide. However, the most appropriate treatment remains to be established. Laser photocoagulation should not be
considered in juxtafoveal cases, as the long-term expansion of the laser scar can cause decreased visual acuity; this is however not a concern for extrafoveal cases.13 PDT with
benzoporphyrin, a derivative verteporfin, is a treatment option for subfoveal CNV in pathological myopia. Treatment with PDT has been described to provide more stable visual acuity compared
with placebo.4 However, more recently, intravitreal injections of anti-VEGF agents have been proposed as the main therapy for the treatment of myopic CNV.14, 15 Indeed, previous reports have
shown that these agents can provide good outcomes in the treatment of myopic CNV. However, most of these studies included patients who had been previously treated with PDT, and also
included older subjects.16, 17, 18 Previous studies by Gharbiya _et al_8 and Nakanishi _et al_16 showed that patients with myopic CNV can gain significant visual improvement to 2 years
following monthly intravitreal injections of bevacizumab. However, Ruiz-Moreno _et al_9 and Ikuno _et al_10 demonstrated that the initial visual improvements in these patients were no longer
significant after 2 years of monthly intravitreal bevacizumab therapy. This lack of significant visual improvement in these two latter studies might be explained by the relatively small
sample sizes for the patients studied by Ruiz-Moreno _et al_9 and the inclusion of only patients >50 years old by Ikuno _et al._10 In the present study, we detected better visual acuity
in patients aged <50 years in the first 18 months of follow-up, which is in agreement with the clinical findings of Yoshida _et al_,19 who also showed similar clinical progress based on
the patient's age. This can be explained by several factors, such as decreased integrity and function of the myopic retinal pigment epithelium in older patients, which might reduce the
inhibition of angiogenesis, with the consequent larger and more active CNV, as well as a delay in the regression of CNV in these older patients.20 Indeed, myopic CNV in older patients can
present clinical and pathophysiological features of both AMD and high myopia, with poor natural outcome. Older patients tend to develop chorioretinal atrophy degeneration, which is a
condition that negatively influences the final visual acuity in these patients. In the present study, the patients were balanced for age and sex, and these factors did not influence the
significantly better final visual acuity at 18 months, compared with baseline. Our findings show that the patients with myopic subfoveal–juxtafoveal CNV had a mean improvement of five lines
at 18 months from baseline, following the intravitreal aflibercept injections. Of note, the treatment of subfoveal myopic CNV with PDT has also been reported to show no significant
improvements at 2 years,5 with several studies demonstrating such inferior visual outcomes correlated to PDT.21, 22 An explanation here might relate to the enlargement of chorioretinal
atrophy around the CNV following PDT, as eyes affected by pathological myopia do not show any increased scarring after treatment: the reduced number of injections might explain the absence
of chorioretinal atrophy associated with CNV. On the basis of a prospective randomised clinical trial, the RADIANCE study, that demonstrated a superiority of intravitreal ranibizumab over
PDT, ranibizumab has recently received approval in the European Union as the first effective anti-VEGF treatment for myopic CNV. The study proved that 40% of patients treated with
ranibizumab, as opposed to 15% of PDT, gained 15 or more letters of visual acuity at 3 months.23 The mean visual acuity gain was ~14 Early Treatment Diabetic Retinopathy Study letters at 1
year at a mean of 3.5 ranibizumab injections. In detail, 50% of the patients required 1–2 injections, 36% required 3–5 injections, and 14% required 6–12 injections over the 12-month study.
In our series of patients, 68.4% of them received 1–2 injections of aflibercept, 31.6% required 3–5 injections, and 0% required 6–12 injections over the 18-month follow-up. Indeed, CNV
myopic eyes treated with aflibercept required a significant lower number of injections considering the longer follow-up of 18 months. A potential risk associated with the treatment of myopic
CNV with anti-VEGFs is the formation of marginal crack lines after treatment-related contraction of the myopic CNV, which is considered as early damage of the retinal pigment epithelium
that might lead to expanding macular chorioretinal atrophy. This factor, in conjunction with treatment-related cumulative damage to the photoreceptors and the underlying retinal pigment
epithelium, might compromise the long-term results, as underlined by the relatively few aflibercept injections needed in the present study. Several studies24, 25, 26, 27 and an open-label,
non-comparative phase II trial known as REPAIR (Ranibizumab for the trEatmentof CNV secondary to pathological myopia; an Individualised Regimen)28, 29 have shown beneficial results of
intravitreal ranibizumab for myopic CNV. Twelve-month data from the phase II study indicated that ranibizumab was associated with significant improvements of BCVA score and central macular
thickness. Furthermore, fewer eyes had subretinal fluid, intraretinal cysts, or oedema at 12 months than at baseline (7.7 _vs_ 67.7%, 13.8 _vs_ 52.3%, 7.7 _vs_ 87.7%, respectively).
Nevertheless, further long-term data for ranibizumab are missing, including data relating to any potential for geographic atrophy, the risk of which was increased with ranibizumab in a
recent AMD study.30 To date, there are no data about the long-term effect of ranibizumab on myopic CNV. A prospective, observational study (LUMINOUS) is ongoing for the evaluation of
long-term safety and efficacy of ranibizumab in routine clinical practice.31 For the reduced number of aflibercept injections that were required, this can be explained by the decreased
aggressiveness of myopic CNV compared with AMD and by the characteristics of aflibercept compared with the other anti-VEGF agents. Indeed, aflibercept binds placental growth factor in
addition to both the VEGF-A and VEGF-B isoforms. Placental growth factor is present in human CNV, and animal studies have demonstrated that it can promote the development of experimental
CNV. Furthermore, aflibercept has a high affinity for VEGF (Kd, 0.5 pM), which is considerably greater than that of ranibizumab and bevacizumab for VEGF, and also of VEGF for its
receptors.23 This provides effective blocking of VEGF with longer duration of action, which thus also promotes extended dosing intervals. Indeed, the 1-year results from the VIEW 1 and VIEW
2 studies showed that in the treatment of CNV due to AMD, aflibercept was non-inferior under similar dosing regimens to ranibizumab.24, 25, 26, 27, 28 Here, aflibercept maintained the visual
gains obtained in the first year of the study with significantly fewer injections compared with ranibizumab. The 1-year data from the CLEAR-IT 2 study also demonstrated good visual and
anatomical outcome with aflibercept. After one injection per month for 3 months, only one or two more injections were needed per eye (with the treatment on an as-required basis, as in the
present study), with a mean time for reinjection of 129 days (ie, every ~4.5 months).32 These outcomes were similar to the ANCHOR,33 MARINA,34 and PRONTO35 ranibizumab trials for the initial
monthly regime of three injections, and in particular, these all indicated the need for less frequent dosing of aflibercept. This has been confirmed also in the present study for the
treatment of myopic CNV. In particular, we have shown the need for significantly fewer aflibercept injections for the <50 years myopic CNV group compared with the ≥50 years myopic CNV,
and over half of the total treated eyes obtained resolution with just one aflibercept injection. This suggests that a three-injection loading phase is not necessary for young patients
affected by myopic CNV who are treated with aflibercept. The good function of retinal pigment epithelium cells in young patients will also allow greater inhibition of CNV growth compared
with the older subjects. Aflibercept is a promising option for patients with naive myopic CNV due to its high binding affinity and extended duration of action. This latter quality is
particularly relevant, because pathological myopia is a chronic disease and it mainly affects patients of working age. Thus for these patients, aflibercept can be considered as a valid
alternative to other anti-VEGF agents, also with apparently fewer injections needed for the treatment. Indeed, as in previous trials in patients with AMD,36, 37 and although not examined
directly here for these patients with naive myopic CNV, the collected data indicate similar visual acuity obtained for aflibercept when compared with ranibizumab and bevacizumab, but with a
longer duration of action for aflibercept, and thus fewer injections needed. Furthermore, considering the reduced number of aflibercept injections on a _pro re nata_ basis observed in our
study, this will also reduce the burden on the health services and reduce the discomfort for the patient. Therefore, this combination of the efficacy, duration of action, economics, patient
benefit, and safety profiles of intravitreal aflibercept now indicate the need for a shift in the treatment choice for patients with naive myopic CNV. REFERENCES * Wong TY, Foster PJ, Hee J,
Ng TP, Tielsch JM, Chew SJ _et al_. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. _Invest Ophthalmol Vis Sci_ 2000; 41: 2486–2494. CAS PubMed Google
Scholar * Yoshida T, Kyoko Ohno-Matsui K, Ohtake Y, Takashima T, Futagami S, Baba T _et al_. Long-term visual prognosis of choroidal neovascularization in high myopia. A comparison between
age groups. _Ophthalmology_ 2002; 109: 712–719. Article PubMed Google Scholar * Lam DSC, Chan W-M, Liu DTL, Fan DSP, Lai WW, Chong KKL . Photodynamic therapy with verteporfin for
subfoveal choroidal neovascularization of pathological myopia in Chinese eyes: a prospective series of 1 and 2 year follow up. _Br J Ophthalmol_ 2004; 88: 1315–1319. Article CAS PubMed
PubMed Central Google Scholar * Blinder KJ, Blumenkranz MS, Bressler NM, Bressler SB, Donato G, Lewis H _et al_. Verteporfin therapy of subfoveal choroidal neovascularization in pathologic
myopia: 2 year results of a randomized clinical trial - VIP report no 3. _Ophthalmology_ 2003; 110: 667–673. Article PubMed Google Scholar * Chan WM, Ohji M, Lai TY, Liu DT, Tano Y, Lam
DS . Choroidal neovascularization in pathological myopia: an update in management. _Br J Ophthalmol_ 2005; 89: 1522–1528. Article PubMed PubMed Central Google Scholar * Yamamoto I,
Rogers AH, Reichel E, Yates PA, Duker JS . Intravitreal bevacizumab (Avastin) as treatment for subfoveal choroidal neovascularization secondary to pathologic myopia. _Br J Ophthalmol_ 2007;
91: 157–160. Article PubMed Google Scholar * Gharbiya M, Giustolisi R, Allievi F, Fantozzi N, Mazzeo L, Scavella V _et al_. Choroidal neovascularization in pathologic myopia: intravitreal
ranibizumab _versus_ bevacizumab: a randomized controlled trial. _Am J Ophthalmol_ 2010; 149: 458–464. Article CAS PubMed Google Scholar * Gharbiya M, Allievi F, Conflitti S, Esposito
M, Scavella V, Moramarco _et al_. Intravitreal bevacizumab for treatment of myopic choroidal neovascularization: the second year of prospective study. _Clin Ter_ 2010; 161: e87–e93. CAS
PubMed Google Scholar * Ruiz-Moreno JM, Montero JA . Intravitreal bevacizumab to treat myopic choroidal neovascularization: 2-year outcome. _Graefes Arch Clin Exp Ophthalmol_ 2010; 248:
937–941. Article CAS PubMed Google Scholar * Ikuno Y, Nagai Y, Matsuda S, Arisawa A, Sho K, Oshita T _et al_. Two years visual results for older Asian women treated with photodynamic
therapy or bevacizumab for myopic choroidal neovascularization. _Am J Ophthalmol_ 2010; 149: 140–146. Article PubMed Google Scholar * Sophie R, Akhar A, Sepah YJ, Ibrahim M, Bittencourt
M, Do DV _et al_. Aflibercept: a potent vascular endothelial growth factor antagonist for neovascular age-related macular degeneration and other retinal vascular diseases. _Biol Ther_ 2012;
2: 1–22. Article Google Scholar * Elshout M, van der Reis MI, Webers CA, Schouten JS . The cost-utility of aflibercept for the treatment of age-related macular degeneration compared to
bevacizumab and ranibizumab and the influence of model parameters. _Graefes Arch Clin Exp Ophthalmol_ 2014; 252: 1911–1920. Article CAS PubMed Google Scholar * Jalkh AE, Weiter JJ,
Trempe CL, Pruett RC, Schepens CL . Choroidal neovascularization in degenerative myopia: role of laser photocoagulation. _Ophthalmic Surg_ 1987; 18: 721–725. CAS PubMed Google Scholar *
Lai TY, Chan WM, Liu DT, Lam DS . Intravitreal ranibizumab for the primary treatment of choroidal neovascularization secondary to pathologic myopia: 12-month results. _Eye_ 2009; 23:
1275–1280. Article Google Scholar * Lai TY, Luk FO, Lee GK, Lam DS . Long-term outcome of intravitreal anti-vascular endothelial growth factor therapy with bevacizumab or ranibizumab as
primary treatment for subfoveal myopic choroidal neovascularization. _Eye_ 2012; 26: 1004–1011. Article CAS PubMed PubMed Central Google Scholar * Nakanishi H, Tsujikawa A, Yodoi Y,
Ojima Y, Otani A, Tamura H _et al_. Prognostic factors for visual outcomes 2 years after intravitreal bevacizumab for myopic choroidal neovascularization. _Eye_ 2011; 25: 375–381. Article
CAS PubMed PubMed Central Google Scholar * Hayashi K, Shimada N, Moriyama M, Hayashi W, Tokoro T, Ohno-Matsui K . Two-year outcomes of intravitreal bevacizumab for choroidal
neovascularization in Japanese patients with pathologic myopia. _Retina_ 2012; 32: 687–695. Article CAS PubMed Google Scholar * Yoon JU, Kim YM, Lee SJ, Byun YJ, Koh HJ . Prognostic
factors for visual outcome after intravitreal anti-VEGF injection for naïve myopic choroidal neovascularization. _Retina_ 2012; 32: 949–955. Article PubMed Google Scholar * Yoshida T,
Ohno-Matsui K, Ohtake Y, Takashima T, Futagami S, Baba T _et al_. Long-term visual prognosis of choroidal neovascularization in high myopia: a comparison between age groups. _Ophthalmology_
2002; 109: 712–719. Article PubMed Google Scholar * Baba T, Kubota-Taniai M, Kitahashi M, Okada K, Mitamura Y, Yamamoto S . Two-year comparison of photodynamic therapy and intravitreal
bevacizumab for treatment of myopic choroidal neovascularization. _Br J Ophthalmol_ 2010; 94: 864–870. Article PubMed Google Scholar * Yoon JU, Byun YJ, Koh HJ . Intravitreal anti-VEGF
_versus_ photodynamic therapy with verteporfin for treatment of myopic choroidal neovascularization. _Retina_ 2010; 30: 418–424. Article PubMed Google Scholar * Ohr M, Kaiser PK .
Aflibercept in wet age-related macular degeneration: a perspective review. _Ther Adv Chronic Dis_ 2012; 3: 153–161. Article CAS PubMed PubMed Central Google Scholar * Wolf S,
Balciuniene VI, Laganovska G, Menchini U, Ohno-Matsui K, Sharma T _et al_. RADIANCE: a randomized controlled study of a ranibizumab in patients with choroidal neovascularization secondary to
pathologic myopia. _Ophthalmology_ 2014; 121: 682–692. Article PubMed Google Scholar * Ladaique M, Dirani A, Ambresin A . Long-term follow-up of choroidal neovascularization in
pathological myopia treated with intravitreal ranibizumab. _Klin Monbl Augenheilkd_ 2015; 232: 542–547. Article CAS PubMed Google Scholar * Pasyechnikova NV, Naumenko VO, Korol AR,
Zadorozhnyy OS, Kustryn TB, Henrich PB . Intravitreal ranibizumab for the treatment of choroidal neovascularizations associated with pathologic myopia: a prospective study. _Ophthalmologica_
2015; 233: 2–7. Article CAS PubMed Google Scholar * Claxton L, Malcolm B, Taylor M, Haig J, Leteneux C . Ranibizumab, verteporfin photodynamic therapy or observation for the treatment
of myopic choroidal neovascularization: cost effectiveness in the UK. _Drugs Aging_ 2014; 31: 837–848. Article CAS PubMed PubMed Central Google Scholar * Deeks ED . Ranibizumab: a
review of its use in myopic choroidal neovascularization. _BioDrugs_ 2014; 28: 403–410. Article CAS PubMed Google Scholar * Tufail A, Narendran N, Patel PJ, Sivaprasad S, Amoaku W,
Browning AC _et al_. Ranibizumab in myopic choroidal neovascularization: the 12-month results from the REPAIR study. _Ophthalmology_ 2013; 120: 1944–1945. Article PubMed Google Scholar *
Tufail A, Patel PJ, Sivaprasad S, Amoaku W, Browning AC, Cole M _et al_. Ranibizumab for the treatment of choroidal neovascularisation secondary to pathological myopia: interim analysis of
the REPAIR study. _Eye_ 2013; 27: 709–715. Article CAS PubMed PubMed Central Google Scholar * Grunwald JE, Daniel E, Huang J, Ying GS, Maguire MG, Toth CA _et al_. Risk of geographic
atrophy in the comparison of age-related macular degeneration treatments trials. _Ophthalmology_ 2014; 121: 150–161. Article PubMed Google Scholar * Novartis Pharmaceuticals. Observe the
effectiveness and safety of ranibizumab in reallife setting (LUMINOUS) [ClinicalTrials.gov identifier NCT01318941]. US National Institutes of Health, http:www.clinicaltrials.gov. 2013. *
Yuzawa M, Fujita K, Wittrup-Jensen KU, Norenberg C, Zeitz O, Adachi K _et al_. Improvement in vision-related function with intravitreal aflibercept: data from phase 3 studies in wet
age-related macular degeneration. _Ophthalmology_ 2015; 122: 571–578. Article PubMed Google Scholar * Heier JS, Boyer D, Nguyen QD, Marcus D, Roth DB, Yancopoulos G _et al_. The 1-year
results of CLEAR-IT 2, a phase 2 study of vascular endothelial growth trap-eye dosed as-needed after 12-week fixed dosing. _Ophthalmology_ 2011; 118: 1098–1106. Article PubMed Google
Scholar * Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY _et al_. Ranibizumab _versus_ verteporfin for neovascular age-related macular degeneration. _N Engl J Med_ 2006; 355:
1432–1444. Article CAS PubMed Google Scholar * Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY _et al_. Ranibizumab for neovascular age-related macular degeneration. _N
Engl J Med_ 2006; 355: 1419–1431. Article CAS PubMed Google Scholar * Wolf A, Reznicek L, Muhr J, Ulbig M, Kampik A, Haritoglou C . [Treatment of recurrent neovascular age-related
macular degeneration with ranibizumab according to the PrONTO scheme]. _Ophthalmologe_ 2013; 110: 740–745 [German]. Article CAS PubMed Google Scholar * Do DV, Schmidt-Erfurth U, Gonzalez
VH, Gordon CM, Tolentino M, Berliner AJ _et al_. The DA VINCI study: phase 2 primary results of VEGF Trap-Eye in patients with diabetic macular edema. _Ophthalmology_ 2011; 118: 1819–1826.
Article PubMed Google Scholar Download references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Neuroscience, Ophthalmology, Polytechnic University of Marche, Ancona, Italy
C Bruè, C Mariotti & A Giovannini * Ophthalmology, Macerata Hospital, Macerata, Italy C Bruè * Ophthalmology, Sant’Orsola Hospital, Malpighi, Italy A Pazzaglia * Ophthalmology, G.
Rodolico Vittorio Emanuele Hospital, Catania, Italy M Reibaldi Authors * C Bruè View author publications You can also search for this author inPubMed Google Scholar * A Pazzaglia View author
publications You can also search for this author inPubMed Google Scholar * C Mariotti View author publications You can also search for this author inPubMed Google Scholar * M Reibaldi View
author publications You can also search for this author inPubMed Google Scholar * A Giovannini View author publications You can also search for this author inPubMed Google Scholar
CORRESPONDING AUTHOR Correspondence to C Bruè. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no conflict of interest. RIGHTS AND PERMISSIONS This work is licensed under a
Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons
license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to
reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Bruè, C.,
Pazzaglia, A., Mariotti, C. _et al._ Aflibercept as primary treatment for myopic choroidal neovascularisation: a retrospective study. _Eye_ 30, 139–145 (2016).
https://doi.org/10.1038/eye.2015.199 Download citation * Received: 27 February 2015 * Accepted: 31 July 2015 * Published: 30 October 2015 * Issue Date: January 2016 * DOI:
https://doi.org/10.1038/eye.2015.199 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative