- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT PURPOSE The purpose of this study was to investigate the outcomes of nasolacrimal duct intubation in the primary treatment of congenital nasolacrimal duct obstruction (CNLDO) in
children aged 7 years and older. METHODS Thirty children aged ≥7 years who underwent primary unilateral nasolacrimal duct intubation because of CNLDO were enrolled in this study. CNLDO
diagnosis was based on signs and symptoms including typical epiphora, increased tear meniscus, recurrent or persistent mucopurulent discharge, and an abnormal dye disappearance test (DDT).
Surgical success was defined as complete resolution of previous signs and symptoms and DDT grade 0–1. RESULTS The mean age was 10.7±2.5 years (ranging from 7 to 15 years). Of the 30
patients, 18 were male and 12 were female. The mean follow-up period was 8.8±3.4 months (ranging from 6 to 16 months). The mean silicone tube removal time was 4.6±1.1 months (ranging from 3
to 6 months). The complete resolution of signs and symptoms with DDT grade 0–1 was observed in 22 of 30 cases (73.3%) during the follow-up period. The mean age of the patients with
unsuccessful outcomes was 12.7±1.4 years, whereas that of the patients with successful outcomes was 10.0±2.4 years, and the difference was statistically significant (_P_=0.006). No serious
intra- and/or post-operative complication was observed. CONCLUSIONS The current study demonstrates that nasolacrimal duct silicone intubation with intranasal endoscopic visualization has
favorable outcomes as a primary treatment of persistent CNLDO in children aged 7 years and older. It can be used to reduce the need for dacryocystorhinostomy which is a more invasive
procedure. SIMILAR CONTENT BEING VIEWED BY OTHERS DCR FOR NASOLACRIMAL DUCT STENOSIS MAY BE LESS EFFECTIVE THAN FOR COMPLETE OBSTRUCTION Article Open access 09 April 2022 MANAGEMENT OF
CONGENITAL NASOLACRIMAL DUCT OBSTRUCTION IN DOWN SYNDROME Article 04 April 2022 CONGENITAL NASOLACRIMAL DUCT OBSTRUCTION UPDATE STUDY (CUP STUDY): PAPER I—ROLE AND OUTCOMES OF CRIGLER’S
LACRIMAL SAC COMPRESSION Article 10 August 2020 INTRODUCTION Congenital nasolacrimal duct obstruction (CNLDO), an extremely common cause of epiphora in the pediatric population, is caused by
a failure of nasolacrimal duct canalization.1 The obstruction is usually at the level of the Hasner valve, at the distal end of the duct.1 Fortunately, spontaneous resolution occurs in most
of the cases by the age of 1 year.2 Probing has been found to have high success rates in the treatment of cases whose obstruction does not resolve spontaneously.3, 4 However, it has been
shown that the success rate of probing diminishes with increasing age.5 Nasolacrimal duct silicone intubation is generally reserved for patients with persistent obstruction after failed
probing or as a primary method in older children.6 The procedure has been used to reduce the need for dacryocystorhinostomy (DCR). It has been displayed that nasolacrimal duct intubation is
a successful procedure in children aged up to 7 years.7, 8, 9, 10, 11 On the other hand, the studies including children older than 7 years are very rare, and those studies had study
population with wide age ranges also including younger children.12, 13 To the best of our knowledge, there is no study evaluating the success rates of nasolacrimal duct intubation for the
treatment of CNLDO in only children older than 7 years of age. Therefore, in the current study, we aimed to investigate the outcomes of primary nasolacrimal duct intubation in the treatment
of CNLDO in children older than 7 years. METHODS Children aged ≥7 years with previously untreated epiphora since birth who underwent primary nasolacrimal duct intubation for management of
CNLDO were enrolled in this prospective study. The diagnosis of CNLDO was based on signs and symptoms including typical epiphora, increased tear meniscus, recurrent or persistent
mucopurulent discharge, and an abnormal dye disappearance test.14 Of the 36 subjects, 3 with punctal occlusion and 3 with bicanalicular obstruction were excluded from the study. Patients
with Down syndrome, a history of previous probing or any other nasolacrimal duct surgery, and a midline facial anomaly were excluded from the study. Thirty patients met the inclusion
criteria. All subjects and parents were informed about the surgical procedure and the informed consents were obtained. The study was conducted in accordance with the Tenets of the
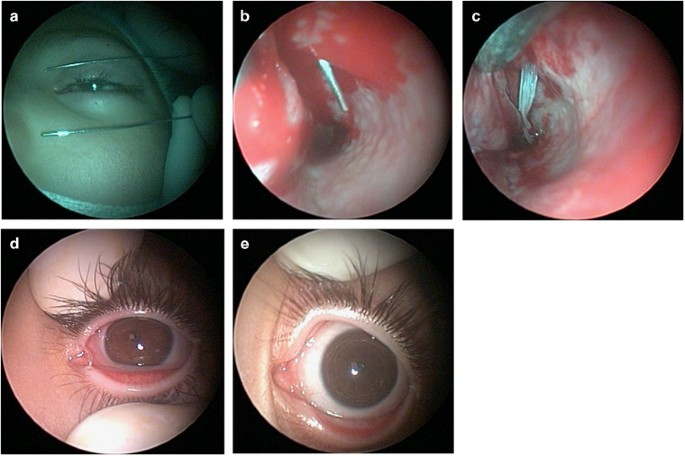
Declaration of Helsinki, and it was approved by the Local Ethics Committee. All nasolacrimal intubations were performed under general anaesthesia with direct intranasal endoscopic
visualization (using a 30°/2.7 mm nasal endoscope) by the same surgeon (SO). Before the intubation procedure, a cotton wool applicator soaked in 2% lidocaine with adrenaline 0.0125 mg/ml was
placed in the nasal cavity for 10 min. After dilating the upper and lower puncta and then probing with a Bowman probe, the metal probes which were fixed to the silicone tubing were passed
into the nasolacrimal duct and nasal cavity via the upper and lower canaliculus. The distal ends of the probes were caught by a small pediatric nasal forceps, and tied together (Figure 1).
Topical corticosteroids and antibiotics were given to the patients for 10 days, postoperatively. All tubes were removed under general anaesthesia. Intra- and/or post-operative complications
were recorded. After the first follow-up visit of week 1, patients were examined for signs and symptoms and dye disappearance test monthly. Surgical success was defined as complete
resolution of previous signs and symptoms and dye disappearance test grade 0–1. A failure of intubation procedure, absence of improvement, or the worsening of the signs and symptoms after a
successful intubation procedure was classified as surgical failure. Patients with unsuccessful outcomes were recommended to undergo DCR. STATISTICAL ANALYSIS SPSS version 16.0 was used for
statistical analysis. The distributions of variables were evaluated with Kolmogorov-Smirnov test. Student _t_-test and Chi-Square test were used to compare the continuous and categorical
variables of the patients with successful and unsuccessful results. A _P_-value of <0.05 was accepted as statistically significant. RESULTS The mean age was 10.7±2.5 years (ranging from 7
to 15 years). Of the 30 patients, 18 were male and 12 were female. All patients had initiation of symptoms of CNLDO within the first month after birth. A bicanalicular silicone tube was
successfully placed in all patients except for two cases for which probing could not be achieved. Inferior turbinate infracture was required in six (20%) of the cases. The mean follow-up
period was 8.8±3.4 months (ranging from 6 to 16 months). The mean silicone tube removal time was 4.6±1.1 months (ranging from 3 to 6 months). Three patients had symptomatic lacrimal fistula
located inferonasal to the medial canthus, preoperatively, which closed spontaneously after the intubation procedure. Although the silicone tubing was well-tolerated in the most of the
cases, three patients (10%) experienced epiphora and minimal mucopurulent secretion with the tubes in place which resolved after the removal of the tubes. The complete resolution of signs
and symptoms with dye disappearance test grade 0–1 was observed in 22 of 30 cases (73.3%) during the follow-up period. In six cases (20%), improvement of the signs and symptoms could not be
achieved after the procedure, and in two cases (6.7%), the intubation procedure could not be performed because of the severe obstruction in the nasolacrimal duct. The mean age of the
patients with unsuccessful outcomes was 12.7±1.4 years, whereas that of the patients with successful outcomes was 10.0±2.4 years and the difference was statistically significant (_P_=0.006).
Gender and time at mean silicone tube removal (both _P_>0.05) were not statistically different. No serious intra- and/or post-operative complications including excessive bleeding,
punctal damage, ‘cheese wiring’, dacryocystitis, or pyogenic granuloma formation were observed. DISCUSSION The present study showed that silicone intubation of nasolacrimal duct with nasal
endoscopic visualization had favorable results as a primary treatment of persistent CNLDO in children older than 7 years of age. CNLDO is a common lacrimal system disorder in children.
Conservative therapy has been found to be sufficient in most cases during the first 12 months, and probing has been proposed as the most effective procedure in cases aged between 12 and 18
months.4, 15 Although silicone intubation is generally used after failure of conservative therapy and probing, it has been suggested as the primary procedure in children older than 1.5–2
years, owing to the decreasing success of probing with age.16 Silicone tubing avoids annular obstruction and contraction inside the nasolacrimal canal during wound healing, by acting as a
temporary stent. Previous studies have shown high success rates of silicone intubation in the treatment of CNLDO in children aged up to 7 years.7, 8, 9, 10, 11 Orhan _et al_9 used silicone
intubation with the help of nasal endoscopic viewing in children with an age range of 18–48 months in the treatment of CNLDO. They found a 100% success rate for a follow-up period ranging
from 4 to 24 months. Repka _et al_8 reported a 90% success rate in children aged 6 to 45 months with no prior nasolacrimal surgical procedure. Andalib _et al_10 achieved an 86.2% success
rate for monocanalicular and an 89% success rate for bicanalicular silicone intubation in children younger than 7 years of age. In our study, the success rate was slightly lower (73.3%) than
in the previous studies, probably owing to the fact that success of nasolacrimal duct intubation reduces with increasing age.17, 18 In addition, in accordance with the previous studies,17,
18 we showed that the mean age of the patients with unsuccessful results was significantly higher than that of the patients with successful results. This may be caused by increased fibrosis
at the site of obstruction in older children. Few studies have investigated the results of nasolacrimal duct silicone intubation in children with wider age ranges.12, 13 Aggarwal _et al_12
achieved complete resolution of symptoms in 80% of patients, in a population including children with ages varied from 11 months to 9 years. They stated that this approach might avoid a DCR
in over 80% of children with epiphora. Kraft _et al_13 analyzed the outcomes of silicone intubations in children aged 6 months to 16 years and found an overall success rate of 80.3%.
However, in the aforementioned studies, no specific analysis for the patients older than 7 years were undertaken. To the best of our knowledge, we are the first in the literature to report
the results of silicone intubation in children aged 7 years or older. External and endonasal DCR have also been used in the treatment of the older children with persistent CNLDO.19, 20
However, silicone intubation is a less invasive procedure compared with external or endonasal DCR. According to our results, in older children with persistent CNLDO, silicone intubation
procedure may reduce the need for DCR, which has greater morbidity. We used direct intranasal endoscopic visualization intraoperatively for the retrieval of the silicone tubes. Retrieval of
metal probes through the inferior meatus can be difficult and complicated by the traumatic mucosal injuries around the inferior turbinate. Direct endoscopic viewing reduces the risk of nasal
mucosal trauma. In addition, it avoids the development of iatrogenic false passages and diminishes the requirement for inferior turbinate infracture. In our study, silicone intubation did
not require inferior turbinate infracture in most of the patients (80%) owing to intranasal endoscopic visualization. Limitations of the present study were the relative small sample size and
short follow-up period. Studies with larger sample sizes, longer follow-up periods and, in addition, a similar study with monocanalicular intubation (as this would avoid the use of a second
anaesthetic) would make useful contributions to the literature in the treatment of older children with persistent CNLDO. In conclusion, the current study demonstrates that nasolacrimal duct
silicone intubation with intranasal endoscopic visualization has favorable outcomes as a primary treatment of persistent CNLDO in children aged 7 years and older. It can be used to reduce
the need for DCR, which is a more invasive procedure. REFERENCES * Schnall BM . Pediatric nasolacrimal duct obstruction. _Curr Opin Ophthalmol_ 2013; 24: 421–424. Article Google Scholar *
Petersen RA, Robb RM . The natural course of congenital obstruction of the nasolacrimal duct. _J Pediatr Ophthalmol Strabismus_ 1978; 15: 246–250. CAS PubMed Google Scholar * Stager D,
Baker JD, Frey T, Weakley DR Jr, Birch EE . Office probing of congenital nasolacrimal duct obstruction. _Ophthalmic Surg_ 1992; 23: 482–484. CAS PubMed Google Scholar * Katowitz JA, Welsh
MG . Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction. _Ophthalmology_ 1987; 94: 698–705. Article CAS Google Scholar * Robb RM . Success rates of
nasolacrimal duct probing at time intervals after 1 year of age. _Ophthalmology_ 1998; 105: 1307–1309; discussion 1309–1310. Article CAS Google Scholar * Al-Faky YH, Al-Sobaie N, Mousa A,
Al-Odan H, Al-Huthail R, Osman E _et al_. Evaluation of treatment modalities and prognostic factors in children with congenital nasolacrimal duct obstruction. _J AAPOS_ 2012; 16: 53–57.
Article Google Scholar * Migliori ME, Putterman AM . Silicone intubation for the treatment of congenital lacrimal duct obstruction. _Ophthalmology_ 1988; 95: 792–795. Article CAS Google
Scholar * Pediatric Eye Disease Investigator Group, Repka MX, Melia BM, Beck RW, Atkinson CS, Chandler DL, Holmes JM _et al_. Primary treatment of nasolacrimal duct obstruction with
nasolacrimal duct intubation in children younger than 4 years of age. _J AAPOS_ 2008; 12: 445–450. Article Google Scholar * Orhan M, Onerci M . Intranasal endoscopic silicone intubation
for congenital obstruction of the nasolacrimal duct in children. _Int J Pediatr Otorhinolaryngol_ 1997; 41: 273–278. Article CAS Google Scholar * Andalib D, Gharabaghi D, Nabai R,
Abbaszadeh M . Monocanalicular versus bicanalicular silicone intubation for congenital nasolacrimal duct obstruction. _J AAPOS_ 2010; 14: 421–424. Article Google Scholar * Yazici B, Akarsu
C, Salkaya M . Silicone intubation with the Ritleng method in children with congenital nasolacrimal duct obstruction. _J AAPOS_ 2006; 10: 328–332. Article Google Scholar * Aggarwal RK,
Misson GP, Donaldson I, Willshaw HE . The role of nasolacrimal intubation in the management of childhood epiphora. _Eye (Lond)_ 1993; 7: 760–762. Article Google Scholar * Kraft SP,
Crawford JS . Silikon tube intubation in disorders of the lacrimal system in children. _Am J Ophthalmol_ 1982; 94: 290–299. Article CAS Google Scholar * MacEwen CJ, Young JD . The
fluorescein disappearance test (FDT): an evaluation of its use in infants. _J Pediatr Ophthalmol Strabismus_ 1991; 28: 302–305. CAS PubMed Google Scholar * Nelson LB, Calhoun JH, Menduke
H . Medical management of congenital nasolacrimal duct obstruction. _Pediatrics_ 1985; 76: 172–175. CAS PubMed Google Scholar * Paul TO, Shepherd R . Congenital nasolacrimal duct
obstruction: natural history and the timing of optimal intervention. _J Pediatr Ophthalmol Strabismus_ 1994; 31: 362–367. CAS PubMed Google Scholar * Lueder GT . Balloon catheter dilation
for treatment of persistent nasolacrimal duct obstruction. _Am J Ophthalmol_ 2002; 133: 337–340. Article Google Scholar * Welsh MG, Katowitz JA . Timing of silastic tubing removal after
intubation for congenital nasolacrimal duct obstruction. _Ophthal Plast Reconstr Surg_ 1989; 5: 43–47. Article CAS Google Scholar * de Souza CE, Nisar J, de Souza RA . Pediatric
endoscopic dacryocystorhinostomy. _Otolaryngol Head Neck Surg_ 2012; 147: 335–337. Article Google Scholar * Ali MJ, Gupta H, Naik MN, Honavar SG . Endoscopic guided single self-linking
silicone stent in pediatric external dacryocystorhinostomy. _Minim Invasive Ther Allied Technol_ 2013; 22: 266–270. Article Google Scholar Download references AUTHOR INFORMATION AUTHORS
AND AFFILIATIONS * Department of Ophthalmology, Gaziantep University Medical School, Gaziantep, Turkey S Okumuş, E Coşkun, Ü Aksoy & I Erbağcı * Department of Ophthalmology, Recep Tayyip
Erdoğan University Medical School, Rize, Turkey V Öner * Department of Otorhinolaryngology, Gaziantep University Medical School, Gaziantep, Turkey C Durucu * Department of Ophthalmology,
Gaziantep Ersin Aslan State Hospital, Gaziantep, Turkey E Durucu * Department of Anesthesiology, Gaziantep University Medical School, Gaziantep, Turkey L Şahin Authors * S Okumuş View author
publications You can also search for this author inPubMed Google Scholar * V Öner View author publications You can also search for this author inPubMed Google Scholar * C Durucu View author
publications You can also search for this author inPubMed Google Scholar * E Coşkun View author publications You can also search for this author inPubMed Google Scholar * Ü Aksoy View
author publications You can also search for this author inPubMed Google Scholar * E Durucu View author publications You can also search for this author inPubMed Google Scholar * L Şahin View
author publications You can also search for this author inPubMed Google Scholar * I Erbağcı View author publications You can also search for this author inPubMed Google Scholar
CORRESPONDING AUTHOR Correspondence to V Öner. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no conflict of interest. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS
ARTICLE CITE THIS ARTICLE Okumuş, S., Öner, V., Durucu, C. _et al._ Nasolacrimal duct intubation in the treatment of congenital nasolacrimal duct obstruction in older children. _Eye_ 30,
85–88 (2016). https://doi.org/10.1038/eye.2015.189 Download citation * Received: 10 May 2015 * Accepted: 08 August 2015 * Published: 09 October 2015 * Issue Date: January 2016 * DOI:
https://doi.org/10.1038/eye.2015.189 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative