- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
Dieter Egli was just about to start graduate school in 1998 when researchers first worked out how to derive human embryonic stem cells. In the two decades since, the prolific cells have been
a fixture of his career. The biologist, now at Columbia University in New York City, has used them to explore how DNA from adult cells can be reprogrammed to an embryonic state, and to
tackle questions about the development and treatment of diabetes. He has even helped to develop an entirely new form of human embryonic stem cell that could simplify studies on what
different human genes do1. His wide-ranging research established him as a leader in embryonic stem-cell biology, a field challenged by restricted funding and an enthusiasm for competing
technologies that don’t carry the same ethical baggage. Still, many say that human embryonic stem cells are now more relevant than ever. “I am very excited about embryonic stem cells,” says
Egli. “They will lead to unprecedented discoveries that will transform life. I have no doubt about it.” Embryonic stem (ES) cells provide unparallelled information on early development. Like
astronomers looking back to the Big Bang for fundamental insight about the Universe, biologists rake over the molecules inside these remarkable entities for clues as to how a single
original cell turns into trillions, with a dizzying array of forms and functions. Scientists have learnt how to turn the cells into dozens of mature cell types representing various tissues
and organs in the body. These are used to test drugs, to model disease and, increasingly, as therapies injected into the body. Starting with an attempt to repair spinal-cord injuries in
2010, there have been more than a dozen clinical trials of cells created from ES cells — to treat Parkinson’s disease and diabetes, among other conditions. Early results suggest that some
approaches are working: a long-awaited report this week shows improved vision in two people with age-related macular degeneration, a disease that destroys the sharpness of vision2. “In some
ways, it’s not a surprise, because 20 years ago we expected it,” says Egli, “but I’m still surprised that this promise is becoming a reality.” TENTATIVE BEGINNINGS In 1981, researchers
managed to culture stem cells from mouse embryos. They soon recognized the research potential of these intriguing entities, which can both replicate themselves and be nudged into becoming
any of the body’s 200-plus cell types3,4. But that trick was not easy to accomplish in primates. It took biologist James Thomson, at the University of Wisconsin–Madison 14 years to achieve
it in monkeys5. Three years later, using donated embryos that had gone unused in fertility treatments, Thomson struck again, creating the world’s first human ES-cell line6. The discovery
sparked an ethical firestorm. Critics, mostly from religious circles, argued that embryos constitute human beings, and wanted to prevent any research that involved destroying them. In 2001,
US President George W. Bush restricted government funding to research on just a few existing ES-cell lines. The decision effectively forced those intent on carrying out the research in the
United States to seek private or state funding, and often to create duplicate laboratories — one for ES-cell research and another for work funded by the US federal government. In other
countries, including Germany and Italy, the creation of the cells was banned altogether. Nonetheless, the research went forward where it could. Investigators in Australia, Singapore, Israel,
Canada and the United States, among others, soon reported that they had converted embryonic stem cells into neurons, immune cells and beating heart cells7. Researchers also discussed plans
to derive stem cells from embryos made by a process called somatic-cell nuclear transfer — the same method used to create cloned animals such as Dolly the sheep — in which the nucleus from
an adult donor cell is transferred into a human egg that has had its nucleus removed. The rationale for this ‘therapeutic cloning’ was to provide a limitless source of dynamic cells with the
same DNA as the cell donor. They started talking about studying complex genetic diseases ‘in a dish’ and replacing failing organs and tissues in the same the way that mechanics replace car
parts. There were several false starts, notably in 2005, when investigators found that South Korean scientist Woo Suk Hwang had fraudulently claimed to have isolated stem cells in this way.
But by 2013, a team led by Shoukhrat Mitalipov, a stem-cell researcher at the Oregon Health and Science University in Portland, finally succeeded8. Throughout the first 15 years, however,
much ES-cell research focused on using the cells to understand pluripotency — the amazing ability to become any type of cell. Bit by bit, scientists have been piecing together the molecular
pathways that make it possible. “We learned pluripotency from ES cells,” says Mitalipov. Such research contributed to arguably the biggest innovation in regenerative medicine and biological
research in the 2000s: the discovery of induced pluripotent stem (iPS) cells. In 2006, stem-cell biologist Shinya Yamanaka at Japan’s Kyoto University worked out how to return adult mouse
cells to an embryonic-like state using just four genetic factors9. The following year, he and Thomson achieved the same feat in human cells10,11. The process offered, in theory, the same
potential pay-off as therapeutic cloning — a limitless supply of pluripotent cells that are genetically matched to a patient — but without the ethical quandaries. Many predicted that iPS
cells would soon displace embryonic stem cells in the research space, but it didn’t happen. The number of ES-cell publications grew rapidly after 2006 and has held pace, at about 2,000 per
year since 2012. Part of the reason was that ES cells were the gold standard against which researchers could compare iPS cells. And even today, there are some who doubt the safety of using
iPS cells. Zhou Qi, a stem-cell biologist at the Chinese Academy of Sciences Institute of Zoology in Beijing, says that concerns that iPS cells would cause tumours inspired him to use ES
cells for more than a dozen clinical trials he is orchestrating. Much of the research on ES cells has been in making them easier to work with. Deriving them was initially a finicky process:
plucking one from a culture and growing it into a new population worked less than 1% of the time. A handful of advances has changed that. In 2007, for example, Yoshiki Sasai at the RIKEN
Centre for Developmental Biology in Kobe, Japan, discovered a molecule, called a ROCK inhibitor12, that could keep ES cells from dying when they were removed from the colonies in which they
thrived. The success rate for creating new colonies shot to 27%. “It fundamentally changed what you could do,” says cell biologist Malin Parmar at Lund University in Sweden. Parmar, who is
using ES cells to derive neurons for a Parkinson’s disease clinical trial, says that such technical advances ushered in “a new golden age” for ES-cell research. The cells can now be produced
quickly, reliably and indefinitely. And yet they somehow avoid turning into cancer, as some feared they would. “We still do not know why or how” they maintain this equilibrium, says
Hiromitsu Nakauchi, a stem-cell biologist at the University of Tokyo, who has been trying to make unlimited supplies of blood platelets from ES and iPS cells. TIME TO DIVERSIFY Researchers
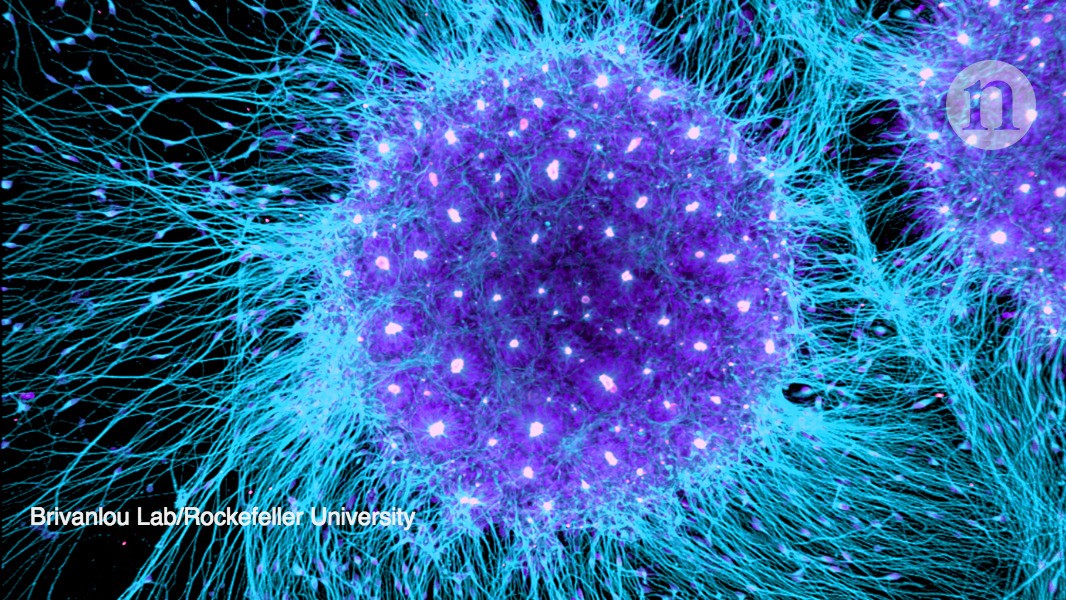
are also trying to grow organs. Given the right signalling molecules and 3D environment, ES cells organize into complex tissues known as organoids, even in a dish. This capacity is important
for researchers such as James Wells at Cincinnati Children’s Hospital in Ohio, who is developing intestinal organoids for testing drugs, and perhaps one day for transplant. And new sources
of ES cells have presented other research tools for genetic disease. In 2004, for example, fertility doctors in Chicago started making ES-cell lines from embryos created through _in vitro_
fertilization that had been found to have a genetic defect, and thus were rejected for fertility treatments. This allowed the team to create cellular models of thalassaemia, Huntington’s
disease, Marfan’s syndrome, muscular dystrophy and other genetic conditions13. In 2007, researchers used ES cells to pin down the molecular changes that lead to cognitive impairments seen in
a heritable condition known as Fragile X syndrome14. Researchers say that iPS cells promise even more for disease-in-a-dish studies — namely the ability to grow stem cells from any living
person with a suspected genetic condition. But many investigators still see strong potential for ES cells in this area. Some conditions cause damage to adult cells that would make any iPS
cells derived from them uninformative. And ES cells still have a supporting role. In 2008, for example, Kevin Eggan at Harvard University in Cambridge, Massachusetts, produced iPS cell lines
from people with the neurodegenerative disease amyotrophic lateral sclerosis (ALS). From previous work with ES cells, Eggan knew how to coax pluripotent cells into becoming motor neurons,
the brain cells affected by the disease. When he did the same with patient-derived iPS cells, he was able to quickly compare the two types of cell. Cells from patients fired much more than
their counterparts from people without the disease15. “We took advantage of all the work we had done with ES cells to understand motor neurons,” says Eggan. Now, an anti-seizure medicine
that quieted iPS cells made from patients is being tested in humans. Results are expected in the next two months. Egli and Nissim Benvenisty at the Hebrew University of Jerusalem overturned
long-held concepts of human biology when they derived ES-cell lines with just half the normal number of chromosomes1. Researchers are now starting to use gene-editing tools on these
‘haploid’ ES cells to understand how genes function in development. Because they have only one set of genes to worry about, the cells could deliver much more straightforward results, Egli
says. The advances in disease research with ES cells have not all come smoothly. It took Douglas Melton at the Harvard Stem Cell Institute in Cambridge 15 years to turn ES cells into
functional β-cells — the pancreatic cells that can sense glucose and produce insulin. Then he couldn’t find any difference between pancreatic cells produced from normal ES cells and iPS
cells from people with type 1 or 2 diabetes. “We know there is a genetic susceptibility, but that doesn’t mean you can see it _in vitro_,” he says. CELL REVIVAL Melton still has plans for
the β-cells he’s made from ES cells. He hopes to transplant them into people with type 1 diabetes to end, or at least reduce, their reliance on insulin injections. The last hurdle in the
work is introducing the cells so that they are not destroyed by the immune system. Semma Therapeutics, a company that Melton founded in Cambridge, aims to do this by ensconcing the cells in
a pouch that would allow nutrients in and insulin out, but would block access to immune cells. He expects to start clinical trials within three years. ViaCyte in San Diego, California,
paused enrolment for a clinical trial it launched in 2014 to redesign its encapsulation technology. Last year, it started a separate clinical trial using a modified delivery mechanism. And
other companies, such as Novo Nordisk in Denmark are starting up programmes for diabetes using cells derived from ES cells. In the clinical realm, many have assumed that iPS cells would
eventually win out over ES cells. One potential advantage is that they can produce cells and tissues with the same DNA as the patient and thus not cause an immune reaction when transplanted.
But for most genetic diseases, including type 1 diabetes, iPS cells created from a patient would contain the mutation that causes the problem, and the cells would have to be modified to
confer any therapeutic benefit. Then there’s the matter of cost. Preparing a single iPS-cell line for clinical use would cost roughly US$1 million, says Jeanne Loring, a stem-cell biologist
at the Scripps Research Institute in La Jolla, California. That’s currently prohibitive if the goal is to use a patient’s own cells, but Loring expects that the price will come down and is
working on developing iPS cells as a treatment for Parkinson’s disease. So far, researchers have initiated just one human trial using cells derived from iPS cells. Led by ophthalmologist
Masayo Takahashi at the RIKEN Center for Developmental Biology, it aims to treat macular degeneration, but was halted in 2014 when investigators decided to simplify the procedure and use
donor-derived, rather than patient-derived, stem cells. It restarted in 2017, but hit another roadblock in January, when a membrane developed in the eye of a participant and had to be
surgically removed. ENJOYING OUR LATEST CONTENT? LOGIN OR CREATE AN ACCOUNT TO CONTINUE * Access the most recent journalism from Nature's award-winning team * Explore the latest
features & opinion covering groundbreaking research Access through your institution or Sign in or create an account Continue with Google Continue with ORCiD








