- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
Sir, Chronic granulomatous disease (CGD) is a rare inherited disorder in which phagocytes lack a functional NADPH oxidase and so cannot generate superoxide anions. This impaired function
leads to the failure to kill catalase positive microbes such as _Staphylococcus aureus_.1 The most common form is X-linked caused by mutations in CYBB encoding gp91phox, the heavy chain of
flavocytochrome b(558).2 Systemically, patients are characterised by hypergammaglobulinemia, hepatosplenomegaly, and lymphadenopathy. Typical ocular lesions associated with this condition
are chorioretinal scars. We present a case of a young male who developed spontaneous macula oedema associated with this condition, which has not previously been described as an ocular
complication. CASE REPORT A 10-year-old male with a genetically proven diagnosis of CGD had been referred to the Southampton Eye Unit because of a vitreous haemorrhage in his left eye. He
had been under follow-up at Great Ormond Street and Yeovil Hospitals. Previously, he had had a bone marrow transplant in July 2002 and consequently developed graft versus host disease
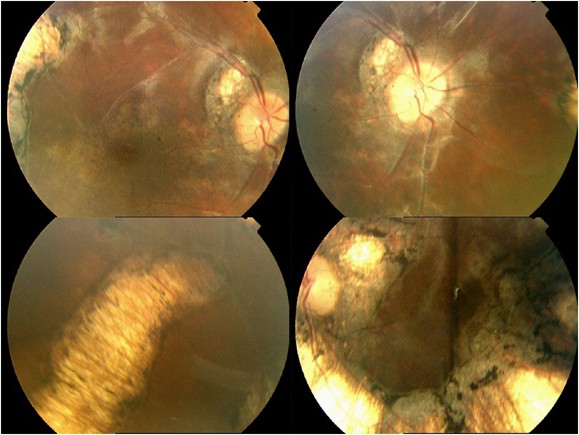
following this, which responded to steroids. He had also been noted to have chorioretinal scars bilaterally (Figure 1) that had no effect clinically on his vision and appeared to be stable.
He initially presented as an emergency to Yeovil Hospital with sudden loss of vision in his left eye (VA=HM) on 21 July 2003 due to a vitreous haemorrhage. A B-scan showed flat retina and
the haemorrhage gradually resolved with no evidence of neovascularisation seen. A referral to Southampton for a vitreoretinal opinion confirmed that the vitreous haemorrhage had resolved
although the vision had only improved to 6/18 due to cystoid macula oedema (CMO) which had not been noted previously. A 4-month follow-up showed no symptomatic change in vision at 6/18 in
the left eye. An OCT was performed (Figure 2) and management was to observe. At 8 months, there was a worsening of the CMO. A subtenons injection of 30 mg of triamcinolone was performed in
September 2004, which resulted in resolution of the CMO and an increase in vision to 6/6 in the left eye. Further 3-month follow-up revealed recurrence of the oedema with decrease in vision
to 6/12 demonstrating only a transient effect of the triamcinolone for CMO. Clinically, the patient was happy with his vision and at this stage further observation only is required. COMMENT
Chronic granulomatous disease is a rare inherited disorder (X-linked or autosomal recessive) in which phagocytes lack the ability to undergo the respiratory burst necessary to kill certain
types of bacteria and fungi leading to recurrent life-threatening infections. The exact incidence is unknown although estimated to be between 1 : 220 000–500 000.3 Initially described in the
1950s the patient invariably died in the first decade of life although significant advances have taken place since improving survival to a median of 25 years.3 Clinically, patients present
with catalase positive infections in which granuloma formation and inflammatory processes predominate. The ‘typical’ retinal abnormality consists of ‘punched out’ chorioretinal lesions
associated with pigment clumping lying along major retinal vessels.4 Other documented ophthalmic complications in CGD include blepharoconjunctivitis and marginal keratitis.5 Spontaneous
cystoid macula oedema has never been reported in association with this disease to our knowledge. The pathogenesis of this is unclear. It may be that the chronic CMO is a long-term
complication of the bone marrow transplant (BMT) or graft versus host disease. BMT has been associated with a microvascular maculopathy consisting of cotton wool spots, exudates,
haemorrhages, and CMO although there are no previous reports of isolated CMO as a late complication following these events. In this case, the oedema initially underwent complete resolution
following a subtenons injection of triamcinolone. The pathophysiology of this ocular manifestation in this condition is unknown. REFERENCES * Behrman RE, Kliegman RM, Jenson HB . _Nelson
Textbook of Paediatrics_, 17th edn. Saunders: London, 2004. Google Scholar * Stasia MJ, Bordigioni P, Floret D, Brion JP, Bost-Bru C, Michel G _et al_. Characterization of six novel
mutations in the CYBB gene leading to different sub-types of X-linked chronic granulomatous disease. _Hum Genet_ 2004 [Epub ahead of print]. * Kamani NR . Chronic granulomatous disease.
Website:www.emedicine.com. * Goldblatt D, Butcher J, Thrasher AJ, Russell-Eggitt I . Chorioretinal lesions in patients and carriers of chronic granulomatous disease. _J Pediatr_ 1999; 134
(6): 780–783. Article CAS Google Scholar * Barequet IS, Wygnanski-Jaffe T, Spierer A, Moisseiev J . Ophthalmic diagnosis of chronic granulomatous disease. _J Pediatr Ophthalmol
Strabismus_ 2002; 39 (1): 44–45. Article Google Scholar Download references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Southampton Eye Unit, Southampton General Hospital, Southampton,
Hampshire, UK L Clifford & R S B Newsom Authors * L Clifford View author publications You can also search for this author inPubMed Google Scholar * R S B Newsom View author publications
You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to L Clifford. ADDITIONAL INFORMATION There are no competing interests. RIGHTS AND PERMISSIONS
Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Clifford, L., Newsom, R. Spontaneous cystoid macula oedema in chronic granulomatous disease: a new posterior segment sign.
_Eye_ 20, 1111–1113 (2006). https://doi.org/10.1038/sj.eye.6702147 Download citation * Received: 17 May 2005 * Accepted: 08 September 2005 * Published: 25 November 2005 * Issue Date: 01
September 2006 * DOI: https://doi.org/10.1038/sj.eye.6702147 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative





