- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT _PURPOSE_ To describe the presentation of cytomegalovirus retinitis (CMVR) in a series of infants. _METHODS_ Immunocompromised infants with either HIV or systemic cytomegalovirus
(CMV) were examined for CMVR. Ocular involvement was recorded and monitored by digital imaging. _RESULTS_ Five infants were detected to have CMVR. All the infants demonstrated changes within
the macula. One infant progressed from a fine granular pattern to fulminant CMVR. _CONCLUSION_ Infants under a year with CMVR have a predilection for the disease to present at the macula,
in contrast to the presentation in adults, which tends to involve more peripheral parts of the retina. SIMILAR CONTENT BEING VIEWED BY OTHERS CYTOMEGALOVIRUS RETINITIS AFTER ALLOGENEIC
HEMATOPOIETIC STEM CELL TRANSPLANTATION UNDER CYTOMEGALOVIRUS ANTIGENEMIA-GUIDED ACTIVE SCREENING Article 12 December 2020 A CROSS-SECTIONAL STUDY OF FUNDUS LESION CHARACTERISTICS IN
PATIENTS WITH ACUTE VISUAL IMPAIRMENT CAUSED BY COVID-19 INFECTION Article Open access 15 November 2024 EXTRALESIONAL MICROVASCULAR AND STRUCTURAL MACULAR ABNORMALITIES IN CYTOMEGALOVIRUS
RETINITIS Article Open access 08 December 2020 INTRODUCTION Cytomegalovirus (CMV) is the most frequent intrauterine viral infection affecting between 0.5% and 2.0% of all live births,1 and
evidence of ocular involvement is present in 5–30%2 of infants exhibiting general symptoms and signs of the infection. CMV retinitis (CMVR) is the most common opportunistic infection
affecting the eyes in adults with HIV and before combination therapy, studies showed that between 20 and 40%2,3 were affected. In contrast, CMVR has been reported in only 5% of children with
acquired immunodeficiency syndrome (AIDS).2,4 In adults, CMVR presents in the peripheral retina in 85% of instances.2 It may affect one or both eyes and is frequently multifocal. It is
typically recognised by a ‘fulminant’ picture of retinal vasculitis and vascular sheathing with areas of yellow-white, full-thickness, retinal necrosis producing retinal oedema associated
with haemorrhage and hard exudates. The ‘indolent or granular’ variant describes a pattern in which there is less oedema and no haemorrhage or vascular sheathing, and this variant is seen
more often in the periphery of the retina. These fulminant and indolent forms represent two ends of the clinical spectrum, and an individual may exhibit elements of both. Isolated macular
involvement occurs in less than 5% of eyes in adults.3 On the clinical suspicion that CMVR might present differently in infants and adults, we analysed the ocular findings of a series of
immunocompromised infants. METHODS Immunocompromised infants presenting to St Mary's Hospital Paediatric Infectious Diseases Unit, London, between September 1999 and October 2001, with
either HIV or under investigation for systemic CMV disease, were screened for CMVR by retinal examination. Contact digital photography was performed in infants with retinal changes using the
RetCam 120 wide-field digital fundus camera (Massie Labs, Dublin, CA, USA). CMV infection was confirmed through virus shedding in the urine and the presence of CMV viraemia. CMV viral load
was measured using assays on either whole blood or plasma and were fully quantitative looking at nested polymerase chain reaction (PCR), second round on the light cycler real time detection
using syber green dye (Micropathology Ltd, Coventry, UK). Where intravitreal ganciclovir was administered, a vitreous biopsy was taken and qualitative PCR-based assays confirmed the presence
of CMV DNA. In the HIV-affected infants, the viral load was measured using the Chiron bDNA assay. RESULTS Retinal abnormalities were detected in five infants screened (age 0–10 months),
four had the HIV infection and one had congenital CMV infection (Table 1). There were two male and three female infants. All of them had bilateral disease. The clinical presentation varied
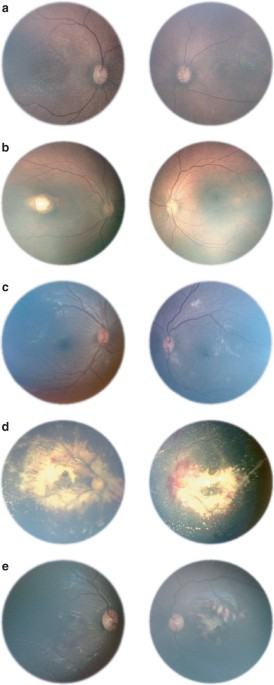
from subtle white flecks at the macula, giving a granular appearance with central pigment epithelial disturbance (Figures 1a and b). The clinical findings did not progress over 3 months in
these two infants. One infant displayed a similar subtle granular appearance at presentation, but this progressed to florid CMVR over 10 days (Figure 1c). The remaining two infants
demonstrated more florid disease at presentation, more characteristic of typical CMVR (Figures 1d and e). The presentation was located at the macula in all the infants in at least one eye.
Three infants with active retinitis had vitreous samples taken, which confirmed the presence of CMV DNA. They were treated with intravenous ganciclovir with or without foscarnet and
subsequently with serial intraocular injections of ganciclovir. DISCUSSION CMVR is a significant cause of ocular morbidity in immunocompromised patients and here we show that the pattern of
presentation, both with respect to its location within the retina and its progression, may be different in infants compared to adults. Several reasons for differences in the presentation of
CMVR have been postulated. For example, reactivation of latent infections is less likely to be present in children, which makes the infection more likely to be a primary infection.2 The
immaturity of the immune system in infants is likely to make the response to infection more severe.5 Finally, different exposure to the virus through breast milk in the perinatal period as
opposed to sexual or percutaneous transmission may affect the presentation.6 The HIV-infected infants in our series were all immunosuppressed and were in their primary HIV viraemic phase, in
contrast to adults with CMVR, who present later in the course of their illness (when the HIV disease progresses to severe immunosuppression). Moreover, as CMV and HIV infections occur
during an important immunological developmental period, there may be interactions between the infections.7 The above factors may contribute to the differences in disease expression, for
example, in a series of infants described by Baumal _et al_4 89% of paediatric cases presented bilaterally (in contrast to approximately 33% of adults) and the retinitis was noted to have a
predisposition for posterior pole of the eyes in infants as compared to adults.4 Similar features of CMVR having a predisposition for the posterior pole and presenting bilaterally have been
recorded in other series of infants with HIV or with congenital CMV. The distribution of active retinitis in infants in other series is shown in Table 2. Congenital CMV infections do not
present in the typical haemorrhagic manner, as seen in immunocompromised children,1 which we noted in the infant with congenitally acquired CMV. No identifiable factors were associated with
the lack of progression in the infants with stable retinitis over the study period. Our findings are interesting, but have limitations. Although the number of infants in this series is
small, they were systematically examined. It was not a prospective study, rather the response to a clinical suspicion, and represents in effect a pilot study that may stimulate further
investigation. REFERENCES * Coats DK, Demmler GJ, Paysee EA, Du LT, Libby C . Ophthalmologic findings in children with congenital cytomegalovirus infection. _J AAPOS_ 2000; 4(2): 110–116.
Article CAS Google Scholar * Cunningham ET, Pepose JS, Holland GN . Cytomegalovirus infections of the retina. In: Ryan SJ (ed). _Retina_, 3rd ed. Mosby: London, 2001, pp 1558–1575. Google
Scholar * Studies of Ocular Complications of AIDS (SOCA) Research Group in Collaboration with the AIDS Clinical Trials Group (ACTG). Foscarnet–ganciclovir cytomegalovirus trial. 5.
Clinical features of cytomegalovirus retinitis at diagnosis. _Am J Ophthalmol_ 1997; 124: 141–157. * Baumal CR, Levin AV, Read SE . Cytomegalovirus Retinitis in Immunosuppressed children.
_Am J Ophthalmol_ 1999; 127(5): 550–558. Article CAS Google Scholar * Williams AJ, Duong T, McNally LM, Tookey PA, Masters J, Miller R _et al_. _Pneumocystis carinii_ pneumonia and
cytomegalovirus infection in children with vertically acquired HIV infection. _AIDS_ 2001; 15(3): 335–339. Article CAS Google Scholar * Du LT, Coats DK, Kline MW, Rosenblatt HM, Bohannon
B, Contant CF _et al_. Incidence of presumed cytomegalovirus retinitis in HIV-infected paediatric patients. _J AAPOS_ 1999; 3(4): 245–249. Article CAS Google Scholar * Levin AV, Zeichner
S, Duker JS, Starr SE, Augsburger JJ, Kronwith S . Cytomegalovirus retinitis in an infant with acquired immunodeficiency syndrome. _Pediatrics_ 1989; 84: 683–687. CAS PubMed Google Scholar
* Pass RF, Stagno S, Myers GJ, Alford CA . Outcome of symptomatic congenital cytomegalovirus infection: results of long-term longitudinal follow up. _Paediatrics_ 1980; 66: 758–762. CAS
Google Scholar * Yamanaka H, Yamanaka J, Okazaki KI, Miyazawa H, Kuratsuji T, Genka I _et al_. Cytomegalovirus Infection of Newborns Infected with HIV-1 from Mother: Case report. _Jpn J
Infect Dis_ 2000; 53: 215–216. CAS PubMed Google Scholar * Vadala P, Fortunato M, Capozzi P, Vadala F . Case report: CMV retinitis in two 10-month-old children with AIDS. _J Paediatr
Ophthalmol Strabismus_ 1998; 35: 334–335. CAS Google Scholar * Dennehy PJ, Warman R, Flynn JT, Scott GB, Mastrucci MT . Ocular manifestations in paediatric patients with acquired
immunodeficiency syndrome. _Arch Ophthalmol_ 1989; 107: 978–982. Article CAS Google Scholar * Salvador F, Blanco R, Colin A, Galan A, Gil-Gibernau JJ . Cytomegalovirus retinitis in
paediatric acquired immunodeficiency syndrome: report of two cases. _J Paediatr Ophthalmol Strabismus_ 1993; 30: 159–162. CAS Google Scholar * Hammond CJ, Evans JA, Shah SM, Acheson JF,
Walters MDS . The spectrum of eye diseases in children with AIDS due to vertically transmitted HIV disease: clinical findings, virology and recommendations for surveillance. _Graefe's
Arch Clin Exp Ophthalmol_ 1997; 235: 125–129. Article CAS Google Scholar Download references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * The Western Eye Hospital, London, UK S M E Wren
& S M Mitchell * Department of Ophthalmology, Imperial College, London, UK A R Fielder & K D Cocker * Department of Paediatrics, St Mary's Hospital, London, UK D Bethell, E G H
Lyall & G Tudor-Williams Authors * S M E Wren View author publications You can also search for this author inPubMed Google Scholar * A R Fielder View author publications You can also
search for this author inPubMed Google Scholar * D Bethell View author publications You can also search for this author inPubMed Google Scholar * E G H Lyall View author publications You can
also search for this author inPubMed Google Scholar * G Tudor-Williams View author publications You can also search for this author inPubMed Google Scholar * K D Cocker View author
publications You can also search for this author inPubMed Google Scholar * S M Mitchell View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING
AUTHOR Correspondence to A R Fielder. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Wren, S., Fielder, A., Bethell, D. _et al._ Cytomegalovirus
Retinitis in infancy. _Eye_ 18, 389–392 (2004). https://doi.org/10.1038/sj.eye.6700696 Download citation * Received: 06 March 2003 * Accepted: 25 July 2003 * Published: 07 April 2004 * Issue
Date: 01 April 2004 * DOI: https://doi.org/10.1038/sj.eye.6700696 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * cytomegalovirus * retinitis *
infants







