- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT _PURPOSE_ To investigate the psychosocial impact of amblyopia therapy on children and their carers. _METHOD_ The study was prospective and incorporated a repeated-measures design. A
total of 59 carers were classified into occluded (_N_=31) or nonoccluded group (_N_=28). A questionnaire consisting of the Perceived Stress Index (PSI) and the Perceived Psychosocial
Questionnaire (PPQ) was used to measure carer's perception of stress and psychosocial well-being of the child respectively prior to and following commencement of treatment. Parametric
and nonparametric tests were used to analyse the data. _RESULTS_ No significant difference in carer's stress (_P_>0.05) and child's psychosocial well-being (_P_>0.05) was
observed between occluded and nonoccluded groups. Within occluded group, carer's stress (_P_>0.05) and child's psychosocial well-being (_P_>0.05) did not differ significantly
before and following commencement of treatment. Within the occluded group, carers felt more negative towards their child following onset of glasses therapy (_P_<0.01) and became more
positive when occlusion was introduced in the subsequent follow-up (_P_<0.01). _CONCLUSIONS_ When compared to carers in the nonoccluded group, those with children undergoing occlusion
therapy did not experience significantly more stress or perceived their child as exhibiting less psychosocial well-being. Within the occluded group, carers’ stress level and child's
psychosocial well-being did not significantly change following onset of occlusion therapy. Carers felt temporarily more negative towards the child following onset of treatment with glasses.
In this study, there is no evidence to indicate that occlusion therapy has negative psychosocial impact on carers and children alike. SIMILAR CONTENT BEING VIEWED BY OTHERS THE IMPACT OF
CHILDHOOD GLAUCOMA ON PSYCHOSOCIAL FUNCTIONING AND QUALITY OF LIFE: A REVIEW OF THE LITERATURE Article Open access 22 March 2023 THE IMPACT OF THE INTEGRATED PEOPLE-CENTERED EYE CARE MODEL
ON MYOPIA CONTROL AMONG CHILDREN AND ADOLESCENTS IN CHINA Article Open access 14 April 2025 PATIENT PERSPECTIVES ON THEIR OUTCOMES FROM STRABISMUS SURGERY UNDERTAKEN FOR PSYCHOSOCIAL REASONS
Article Open access 21 June 2024 INTRODUCTION Amblyopia is an acquired defect in vision caused by abnormal visual experience early in life. On clinical testing, it is usually unilateral but
may be bilateral. Amblyopia itself produces no apparent change in the appearance of ocular structures. The visual system is sensitive to the effects of abnormal visual experience only
during a limited time in infancy and childhood when it is immature and plastic. This period extends from birth through the end of the first decade. Visual loss can be potentially reversed if
amblyopia is detected and treated within this period. It is the most prevalent visual disability in children. A recent review estimated the prevalence of amblyopia in the UK to be between
2.4 and 6.1% in children of 3–4 years old.1 Numerous studies have documented the association between amblyopia and a variety of functional difficulties such as poor reading performance,2,3
and reduced stereopsis and motor abilities involving eye–hand coordination.4 As such functions are important for a child's development,5,6 early detection and treatment of amblyopia is
arguably the logical step forward. The need to implement treatment is more pressing when Tommila and Tarkkanen,7 and more recently Rahi _et al_,8,9 reported that the incidence of loss of
vision in the healthy eye of individuals with amblyopia is higher compared to the normal population. Currently, various screening procedures are used to identify amblyopia in children
between the age of 3 and 4 years in the UK.10 Amblyopia is usually treated by correcting the refractive error with glasses and/or occlusion therapy involving patching of the nonamblyopic
eye. Occlusion therapy has been used for over 250 years11 and is aimed at encouraging the development of vision in the amblyopic eye. The efficacy of both the screening and treatment of
amblyopia has been questioned recently by a systematic review.1 The authors concluded that there is insufficient evidence to indicate that amblyopia represents a significant disability that
affects day-to-day functioning. They also highlighted a need for more investigations on the potential negative impact of treatment, particularly the psychosocial consequences of treatment on
the child and his/her family. The objective of the present study is to address the latter point. A few studies have begun to address the psychosocial impact of amblyopia and its treatment.
Packwood _et al_12 surveyed 25 adults with amblyopia and reported that this sample perceived a greater degree of somatisation, obsessive-compulsive behaviour, interpersonal sensitivity,
depression, and anxiety compared to those who has strabismus and those without amblyopia. In addition, a substantial number of those with amblyopia reported that amblyopia had interfered
with school, work, and lifestyle. A few issues are worth noting. First of all, the small sample size and the retrospective nature of the study rendered the interpretation of the data
difficult. It is unclear from the data if amblyopia _per se_ had a direct effect on school, work, and lifestyle of those who had this condition. More importantly, the study did not specify
in what ways amblyopia interfered with these factors and if the psychosocial impact of this condition was substantial enough to affect day-to-day functioning. Hence whether amblyopia can be
considered a significant disability remains unclear. In addition, the psychosocial impact of the amblyopia treatment itself was not explored. Recently, the Paediatric Eye Disease
Investigator Group conducted a randomised clinical trial comparing the efficacy of occlusion therapy and atropine penalisation in children with moderate amblyopia.13,14 Part of the study
aimed to evaluate the social stigma associated with the treatments. Approximately 5 weeks into treatment, parents of children with amblyopia given atropine treatment (_n_=181) or occlusion
therapy (_n_=192) completed the 18-item Amblyopia Treatment Index consisting of three subscales measuring adverse effects of treatment, difficulties with compliance, and social stigma of
treatment. The findings indicated that parents of children undergoing occlusion therapy perceived significantly more problems with the treatment compared to those who were given atropine.
However, both treatments were equally well tolerated. Although this study compared the adverse effects of two treatment modalities, it did not address the psychological impact of the
treatments on the child and parents compared to the pretreatment period. Such information is needed to assess the treatment impact and determine if treatment benefits outweigh potential
consequences. The present study addresses three issues. The carer's perception of their personal stress level, psychosocial impact of occlusion therapy on the child, and carer–child
relationship were evaluated prior to and following treatment. MATERIALS AND METHODS PARTICIPANTS All primary carers attending a clinic in a large district general hospital, with children who
were diagnosed with probable amblyopia or reduced vision, and about to undergo treatment (glasses and/or occlusion therapy) for the first time, were invited to participate in this research.
This is an ongoing study that commenced since October 2000. To date, a total of 93 participants have been recruited. However, only 65 of them have completed the study. The data of these
participants will be discussed in this paper. DEMOGRAPHICS OF CARERS Majority of the carers (_n_=52) were mothers of the child seen in the clinic. A total of 96.9% of the sample was
Caucasians. The mean age of carers was 32.4 (SD=6.3) years old. A total of 15.9% of the sample had tertiary education or higher; 38.1, 42.9, and 3.1% obtained college, secondary level, and
primary level, respectively. In all, 80% of the sample had more than one child other than the one who was seen at the clinic. Among the siblings, majority (80%) did not have amblyopia. The
carer's understanding of amblyopia was also surveyed. A substantial number of them (43.1%) admitted that they knew little or nothing about the condition. DEMOGRAPHICS OF AMBLYOPIC CHILD
There were 36 males and 29 females with a mean age of 57.1 (SD=20.9) months old (ie 4.8 years old). Of these children, 60% attended primary school; 21.5% were in nursery, 12.3% in play
groups, and 6.2% cared at home. A total of 26 (40.0%) were diagnosed anisometropic amblyopia, 24 (36.9%) strabismic amblyopia, 13 (20.0%) combined strabismic and anisometropic amblyopia, and
two (3.1%) refractive amblyopia. Mean visual acuity of the amblyopic eye at presentation was 0.32 (SD=0.54) using equivalent decimal Snellen notation. MATERIALS PERCEIVED PSYCHOSOCIAL
QUESTIONNAIRE Prior to the commencement of the study, a focus group was conducted to investigate the general issues related to amblyopia treatment, in particular occlusion therapy. The focus
group consisted of ophthalmologists, orthoptists, parents of children who have experienced occlusion therapy, and a psychologist. The issues raised included the child's ability to
concentrate, the degree of demands placed on the carer, the extent that the child cries more often, and play situations. These were incorporated into the development of the questionnaire
used in this study, particularly the Perceived Psychosocial Questionnaire (PPQ).15 PPQ is intended to measure the psychosocial well-being of the child. Higher overall PPQ score indicates
lower psychosocial well-being. PERCEIVED STRESS INDEX The stress level of carers was measured using the standardised global stress scale known as the Perceived Stress Index (PSI).16 This
10-item index measures the degree to which general situations are perceived as stressful. Higher overall score represents a higher perception of stress experienced. It was important to
measure general stress in this study as opposed to specific stress as a result of occlusion therapy. Occlusion therapy _per se_ may not exert a direct impact on the carer's life, but
may affect the predictability, controllability, and the degree of overload experienced by the carer in their daily lives. These three components have been repeatedly found to be important
factors associated with stress and are measured by PSI.17,18 CARER–CHILD RELATIONSHIP The carer–child relationship was depicted by how upset, irritated, patient, and attentive the carer felt
towards the child. A total score was obtained by the summation of carer's response in these areas. Higher score indicates better relationship. QUESTIONNAIRE COMPONENTS In summary, the
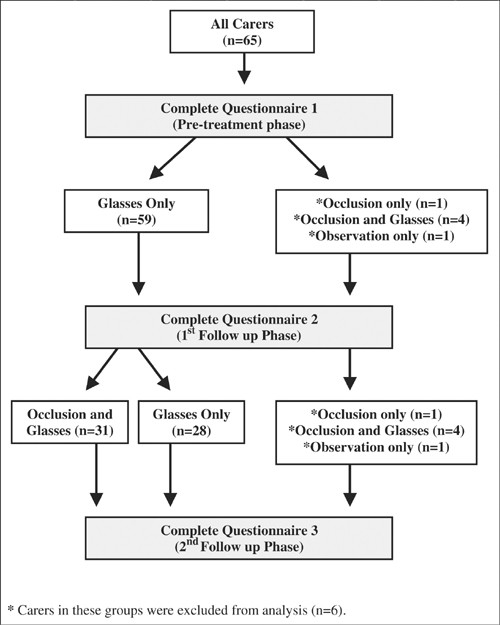
five subsections of the study questionnaire are listed in Table 1. STUDY DESIGN The study was prospective and incorporated a repeated-measures design. Carers were asked to complete the
previously discussed questionnaire at three different time points, that is, pretreatment phase, 1st follow-up phase, and 2nd follow-up phase (see Figure 1). The mean time interval between
the pretreatment phase and 1st follow-up phase, and 1st follow-up phase and 2nd follow-up phase were 6.9 (SD=2.4) weeks and 7.4 (SD=8.6) weeks, respectively. PRETREATMENT PHASE The diagnosis
of amblyopia was confirmed in this first visit to the outpatient clinic. All carers were asked to complete one questionnaire prior to the commencement of amblyopia treatment. Following the
consultation, carers were given instructions to proceed with the amblyopia treatment, that is, spectacle correction (glasses) and/or occlusion the next day. (Majority of patients with
amblyopia initially received glasses. In the follow-up clinic, these patients were assessed for visual improvement in the amblyopic eye. When no significant improvement was shown, occlusion
therapy was initiated. However, a small minority of patients commenced on occlusion therapy during the first (pretreatment) visit.) All except six children were prescribed glasses alone as
their initial treatment. One of the six children was instructed to commence with occlusion therapy and four were treated with both occlusion and glasses. One was under observation only. The
carers of these six children were excluded from the study to reduce bias. 1ST FOLLOW-UP PHASE All carers returned to the clinic for their child's routine follow-up, during which they
were asked to complete the second questionnaire. This was carried out prior to their consultation. In this visit, some of the children who were initially prescribed glasses were placed on
occlusion therapy (_n_=31) because of the lack of improvement in the visual acuity of the amblyopic eye. The carers of these children were classified into the occluded group. Those who were
not given occlusion therapy at this stage (_n_=28) were classified into the nonoccluded group. 2ND FOLLOW-UP PHASE During this visit, all participants completed the third questionnaire prior
to seeing the orthoptists and/or ophthalmologist for further follow-up. DATA ANALYSIS _t_-Tests were used to analyse the carer's perception of personal stress level, the child's
psychosocial well-being, and carer–child relationship prior to and following the onset of occlusion therapy. The response of carers with children undergoing occlusion was also compared to
those whose child was prescribed glasses only. Nonparametric tests were used to assess the separate components of the carer–child relationship. This was conducted for both between (using
Mann–Whitney U-test) and within (using Wilcoxon signed rank test) the two groups. The data were analysed using SPSS version 10 (SPSS Inc.) and Excel version 7 (Microsoft Corporation).
RESULTS CARER'S PERCEIVED STRESS There was no significant difference in PSI scores between occluded and nonoccluded groups (_p_>0.05) (Table 2). Within the occluded group,
carer's perception of stress did not differ significantly between the pretreatment, 1st follow-up, and the 2nd follow-up phases (_p_>0.05). The result was similar within the
nonoccluded group. CARER'S PERCEPTION OF CHILD'S PSYCHOSOCIAL WELL-BEING The PPQ scores between the occluded group and nonoccluded group did not differ significantly between the
three phases (_p_>0.05). However, the occluded group scored consistently higher in all three phases. No significant difference in PPQ scores was observed within occluded (_p_>0.05) and
nonoccluded groups (_p_>0.05) (Table 3). RELATIONSHIP BETWEEN CARER AND CHILD The carer–child relationship scores were similar between the occluded and nonoccluded groups (Table 4).
There were no significant between-group differences in how upset, irritated, patient, or attentive carers were towards the child across all three phases (_p_>0.05) (Table 4). It is
interesting to note that the carer–child relationship score was lower for both groups in 1st follow-up phase compared to the pretreatment phase (Tables 5 and 6). In particular, they were
more upset and irritated with the child during this phase. However, these negative feelings were reduced in the 2nd follow-up phase. These findings only reached statistical significance
within the occluded group (_p_<0.01). Carers in this group were significantly less upset and irritated during 2nd follow-up phase compared to the 1st follow-up phase (Table 5). A similar
pattern emerged within the nonoccluded group, but the difference was not substantial enough in most cases to produce statistical significance with the exception of carer's irritability
towards the child. Carers in the nonoccluded group experienced a significant reduction in their irritable feelings towards the child (_p_<0.05) in the 2nd follow-up phase compared to the
1st follow-up phase (Table 6). In both groups, carers were as patient and attentive to the child in all three phases. EFFECT OF GLASSES ON CHILDREN The finding that both groups experienced a
lower carer–child relationship score during the 1st follow-up phase indicated the possibility that glasses _per se_ may be the reason for this phenomenon. All patients in our sample were
prescribed glasses following their pretreatment phase to correct the refractive error. Hence glasses alone may influence the well-being of the carer and/or the child. An additional analysis
was conducted on carers who have children given glasses as their initial treatment during the 1st follow-up phase (_n_=59). Carer's perception of his/her stress level, child's
psychosocial well-being, and carer–child relationship between pretreatment and 1st follow-up phase were examined. Results indicated no difference in PSI (_p_>0.05) and PPQ (_p_>0.05)
scores between these phases. However, carer–child relationship score was significantly lower following the onset of glasses in the 1st follow-up phase (_p_<0.01) (Table 7). Particularly,
carers were significantly more upset (_p_<0.01) and irritated (_p_<0.01) with the child at this phase compared to the pretreatment phase. DISCUSSION The findings of this study have
highlighted three important points. Firstly, the study demonstrated that carers with children undergoing occlusion therapy and those prescribed glasses only did not differ significantly in
their experience of stress. The implication of this finding suggests that with regard to carers, occlusion therapy is not more stressful than glasses. One study reported that occlusion
therapy has more problems with adverse effects, compliance, and social stigma compared to atropine treatment.13 This suggests that occlusion therapy may be a more stressful treatment
compared to atropine. However, whether this was the case was not addressed in that study. Our study showed that when compared to glasses, occlusion therapy was not a more stressful treatment
for the carer. Additionally, carer's experience of general stress before and following commencement of treatment did not differ significantly. This implies that carer's state of
general stress was not influenced substantially by the treatment. This finding appears to contradict the conventional anecdotal evidence that suggests occlusion therapy to be a stressful
procedure for carers. There are a few plausible explanations for this discrepancy. Firstly, occlusion therapy itself may represent a stressful experience, but the degree of stress is not
substantial enough to exert a measurable impact. It is also possible that the stress experienced is transient. Amblyopia treatment may have specific difficulties in the initial stages of
treatment when acuity is at its worst, but subsequently becomes more acceptable as the visual acuity improves. Therefore, carers may experience significant stress at onset of treatment, but
their level of stress reduces at the time of measurement. Finally, there are few individuals who may be very susceptible to stress, and the clinicians’ experience with these individuals may
have biased their impression, whereas the majority of carers cope well. The second point concerns the psychosocial impact of occlusion treatment on the amblyopic child. A common complaint
from parents with children undergoing occlusion therapy is that the child becomes more distressed following the onset of treatment. The repeated application of a patch for occlusion therapy
may cause skin irritation or rarely an allergic reaction. The occlusion of the nonamblyopic eye understandably causes a degree of distress in a young child. Although occlusion therapy can be
distressing, our data did not indicate that children with occlusion were experiencing significantly more distress following the onset of treatment. In addition, carers in the occluded group
did not perceive their child to experience poorer psychosocial well-being as compared to those just given glasses. Our findings seem to suggest that occlusion therapy does not exert a
significant adverse psychosocial impact on children undergoing occlusion and that it is not more distressing than treatment with glasses. Thirdly, with regard to the carer–child
relationship, it is interesting to note that carers felt that they are more upset and irritated with the child following the onset of treatment with glasses. This experience was reversed and
carers felt less upset and irritated during the 2nd follow-up phase when treatment has progressed for a time. These findings were more marked among carers within the occluded group. The
onset of occlusion was not related with more negative experience but rather surprisingly, carers in the occluded group experienced significantly more positive feelings towards the child as
opposed to carers in the nonoccluded group. It appears that carers with children undergoing occlusion therapy were more understanding towards their child's treatment experience. Since
further analysis showed that glasses alone also have the same impact, it is plausible that prescribing glasses as treatment exerts a negative but transient influence on the carer–child
relationship. The addition of occlusion therapy to glasses did not contribute to a substantial worsening in the carer–child relationship. Hence, our data support the findings of the
Paediatric Eye Disease Investigator Group that occlusion therapy is generally well tolerated.13 There are a few limitations in this study that should be taken into consideration when
interpreting our findings. Firstly, the period between consultations or study phases differs between each participant. This could possibly influence the results. For example, carers who had
a longer period between the pretreatment phase and the 1st follow-up phase may have a different response compared to those who had a shorter period. This limitation should be noted, although
it is practically difficult to control the length of intervals between follow-up in clinical settings. Secondly, our study only measures the _perception_ rather than the objective measure
of carer's stress, child's psychosocial well-being, and carer–child relationship. Hence we can only comment on the _perceived_ experience of the carer rather than what is actually
experienced. It is important that future studies evaluate the objective experience of amblyopia treatment in patients and carers alike. Thirdly, there are various factors such as treatment
compliance, treatment acceptability, duration of occlusion, density of amblyopia, types of amblyopia, and others that may influence the success of amblyopia treatment.19,20,21,22,23,24 These
in turn may have a significant influence on the psychosocial impact of amblyopia treatment. Data are currently being collected for further analysis in this on going study that will address
some of these issues. In summary, our study has attempted to address the psychosocial impact of occlusion therapy on patient and carer. Following onset of occlusion therapy, carers did not
perceive their stress level to be higher or their child's psychosocial well-being to be poorer. However, carers were temporarily more upset and irritated with the child following onset
of amblyopia treatment with glasses. The transient nature of this experience is reassuring. In conclusion, there is at present no evidence from this study to suggest that occlusion therapy
exerts a significant adverse psychosocial impact on carers and patients alike. This information should be taken into account when discussing the advantages and disadvantages of amblyopia
treatment and in particular that of occlusion therapy. REFERENCES * Snowdon S, Stewart-Brown SL . _Pre-school Vision Screening: Results of a Systematic Review_. University of York: NHS
Centre for Reviews and Dissemination, 1997. Google Scholar * Grosvenor T . Are visual anomalies related to reading ability? _J Am Optom Assoc_ 1977; 48(4): 510–517. CAS PubMed Google
Scholar * Grisham JD, Simons HD . Refractive error and the reading process: a literature analysis. _J Am Optom Assoc_ 1986; 57(1): 44–55. CAS PubMed Google Scholar * McGee RWS, Simpson
A, Silva PA . Stereoscopic vision and motor ability in a large sample of seven-year-old children. _J Hum Movement Stud_ 1991; 13: 343–352. Google Scholar * Williams SM, Sanderson GF, Share
DL, Silva PA . Refractive error, IQ and reading ability: a longitudinal study from age seven to 11. _Dev Med Child Neurol_ 1988; 30(6): 735–742. Article CAS Google Scholar * Fielder AR,
Moseley MJ . Does stereopsis matter in humans? _Eye_ 1996; 10 (Part 2): 233–238. Article Google Scholar * Tommila V, Tarkkanen A . Incidence of loss of vision in the healthy eye in
amblyopia. _Br J Ophthalmol_ 1981; 65(8): 575–577. Article CAS Google Scholar * Rahi JS, Logan S, Borja MC, Timms C, Russell-Eggitt I, Taylor D . Prediction of improved vision in the
amblyopic eye after visual loss in the non-amblyopic eye. _Lancet_ 2002; 360(9333): 621–622. Article Google Scholar * Rahi J, Logan S, Timms C, Russell-Eggitt I, Taylor D . Risk, causes,
and outcomes of visual impairment after loss of vision in the non-amblyopic eye: a population-based study. _Lancet_ 2002; 360(9333): 597–602. Article Google Scholar * Stewart-Brown SL,
Haslum MN, Howlett B . Preschool vision screening: a service in need of rationalisation. _Arch Dis Child_ 1988; 63(4): 356–359. Article CAS Google Scholar * de Buffon M . Dissertation sur
la cause de strabisme ou de les yeux louches. _Bull Mem Acad Sci_ 1743; 3: 174. Google Scholar * Packwood EA, Cruz OA, Rychwalski PJ, Keech RV . The psychosocial effects of amblyopia
study. _J AAPOS_ 1999; 3(1): 15–17. Article CAS Google Scholar * The study was conducted by the Pediatric Eye Disease Investigation Group (PEDIG). A randomized trial of atropine _vs_
patching for treatment of moderate amblyopia in children. _Arch Ophthalmol_ 2002; 120(3): 268–278. * Group TPEDI. The clinical profile of moderate amblyopia in children younger than 7 years.
_Arch Ophthalmol_ 2002; 120(3): 281–287. * Lukman H, Choong YF, Martin S, Laws DE . Development of Perceived Psychosocial Questionnaire (PPQ), a psychosocial measure to study the effect of
amblyopia treatment. Paper presented at The Association of Research in Vision and Ophthalmology (ARVO), 2002, Florida, USA. * Cohen S, Kamarck T, Mermelstein R . A global measure of
perceived stress. _J Health Soc Behav_ 1983; 24(4): 385–396. Article CAS Google Scholar * Friend TH . Behavioral aspects of stress. _J Dairy Sci_ 1991; 74(1): 292–303. Article CAS
Google Scholar * Steptoe A . Invited review. The links between stress and illness. _J Psychosom Res_ 1991; 35(6): 633–644. Article CAS Google Scholar * Smith LK, Thompson JR, Woodruff G,
Hiscox F . Factors affecting treatment compliance in amblyopia. _J Pediatr Ophthalmol Strabismus_ 1995; 32(2): 98–101. CAS PubMed Google Scholar * Fielder AR, Irwin M, Auld R, Cocker KD,
Jones HS, Moseley MJ . Compliance in amblyopia therapy: objective monitoring of occlusion. _Br J Ophthalmol_ 1995; 79(6): 585–589. Article CAS Google Scholar * Woodruff G, Hiscox F,
Thompson JR, Smith LK . Factors affecting the outcome of children treated for amblyopia. _Eye_ 1994; 8 (Part 6): 627–631. Article Google Scholar * Fielder AR, Auld R, Irwin M, Cocker KD,
Jones HS, Moseley MJ . Compliance monitoring in amblyopia therapy. _Lancet_ 1994; 343(8896): 547. Article CAS Google Scholar * Newsham D . A randomised controlled trial of written
information: the effect on parental non-concordance with occlusion therapy. _Br J Ophthalmol_ 2002; 86(7): 787–791. Article CAS Google Scholar * Newsham D . Parental non-concordance with
occlusion therapy. _Br J Ophthalmol_ 2000; 84(9): 957–962. Article CAS Google Scholar Download references ACKNOWLEDGEMENTS This study is funded by a grant from the Welsh Office for
Research and Development (WORD) and was presented in part at the Annual Congress, The Royal College of Ophthalmologists, Manchester, May 2002 and the Association for Research in Vision and
Ophthalmology (ARVO), Fort Lauderdale, Florida, May 2002. AUTHOR INFORMATION Author notes * The authors have no proprietary or financial interest in any products mentioned in the paper
AUTHORS AND AFFILIATIONS * Department of Ophthalmology, Singleton Hospital, Swansea, UK Y F Choong & D E Laws * Centre for Psychology University of Wales Institute, Cardiff, UK H Lukman
* Department of Orthoptics, Singleton Hospital, Swansea, UK S Martin Authors * Y F Choong View author publications You can also search for this author inPubMed Google Scholar * H Lukman View
author publications You can also search for this author inPubMed Google Scholar * S Martin View author publications You can also search for this author inPubMed Google Scholar * D E Laws
View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to Y F Choong. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT
THIS ARTICLE CITE THIS ARTICLE Choong, Y., Lukman, H., Martin, S. _et al._ Childhood amblyopia treatment: psychosocial implications for patients and primary carers. _Eye_ 18, 369–375 (2004).
https://doi.org/10.1038/sj.eye.6700647 Download citation * Received: 17 December 2002 * Accepted: 06 May 2003 * Published: 07 April 2004 * Issue Date: 01 April 2004 * DOI:
https://doi.org/10.1038/sj.eye.6700647 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * amblyopia * psychosocial * occlusion * treatment *
stress