- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
MAIN Sir, Acute retinal necrosis (ARN) is a distinct ocular inflammatory syndrome whose prominent features include severe occlusive vasculitis, diffuse necrotizing retinitis, and
moderate-to-severe vitreous cellular reaction.1 It preferentially affects the peripheral retina, and involvement of the posterior pole is uncommon.1 We describe a case of an atypical macular
lesion as a late complication of ARN, which responded favourably despite delayed treatment. CASE REPORT A 68-year-old immunocompetent woman presented complaining of reduction of vision in
the left eye over the prior 3 weeks. On examination, her corrected visual acuity in the affected eye was 6/24 and there was evidence of left minimal anterior uveitis and moderate vitritis.
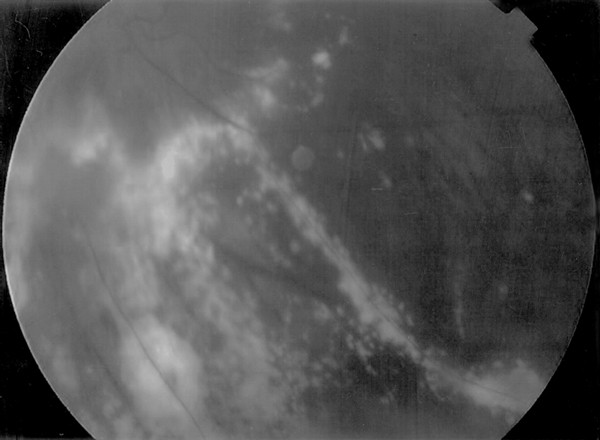
Intraocular pressures were normal, and bilateral moderate cataracts were noted. Fundoscopy in the left eye revealed peripheral confluent geographic areas of retinal necrosis and extensive
vasculitis involving predominantly the retinal arteries (Figure 1). Vitreous and retina in the fellow eye were unremarkable. Unilateral ARN was diagnosed on her clinical features, but the
patient declined treatment and further follow-up. After 8 months, she attended the eye clinic reporting further decrease of her vision in the affected eye. Her visual acuity in the left eye
had decreased to perception of light, and on retinal examination along with peripheral necrotic areas, a nodular lesion with ill-defined borders associated with retinal haemorrhage,
exudation, and swelling at the macula was noted (Figures 2 and 3). The patient was commenced on oral acyclovir 800 mg five times per day, and 3 days later methylprednisolone 16 mg t.d.s. was
introduced. After 1 week, best-corrected visual acuity had improved to 6/60 and the nodular lesion at the posterior pole had significantly reduced in size (Figure 4). Treatment was tapered
and retinitis remained quiescent over 6 months follow-up. COMMENT ARN is a necrotizing vaso-occlusive retinitis caused mainly by varicela zoster or herpes simplex virus (types 1and 2) and
rarely by cytomegalovirus.1 Standard diagnostic criteria include chorioretinal vasculitis, retinal necrosis, anterior uveitis, and vitritis.2 Lesions characteristically develop in the
midperipheral retina, and in the absence of treatment retinitis progresses circumferentially with subsequent disappearance of the intraocular inflammation usually between 6 and 12 weeks
following the onset of symptoms.2,3 Since ARN typically affects healthy patients, the stimulated inflammatory response is usually contained in the peripheral retina because of intact,
effective immune resistance to the virus.4 Posterior pole involvement is very rare and typically occurs late in the disease course.1,4 This may manifest as advancement of the leading edge of
the retinal whitening towards the macula, formation of macular holes, or development of macular edema.1,3 Treatment of ARN includes administration of systemic acyclovir, antithrombotic
agents, high dose of systemic corticosteroids, and prophylactic application of laser photocoagulation posterior to the area of retinitis.1 The above case shows that intraocular inflammation
can be present many months after diagnosis, resulting in unusual manifestations at the posterior pole and consequent devastating reduction of central vision. Although prompt treatment is
mandatory for the resolution of retinal lesions, we clearly demonstrated that even late administration of antiviral and anti-inflammatory agents may lead to significant improvement in visual
acuity. REFERENCES * Duker JS, Blumenkranz MS . Diagnosis and management of the acute retinal necrosis (ARN) syndrome. _Surv Ophthalmol_ 1991; 35(5): 327–343. Article CAS Google Scholar
* Holland GN . Standard diagnostic criteria for the acute retinal necrosis syndrome. Executive Committee of the American Uveitis Society. _Am J Ophthalmol_ 1994; 117(5): 663–667. Article
CAS Google Scholar * Fisher JP, Lewis ML, Blumenkranz M, Culbertson WW, Flynn Jr HW, Clarkson JG _et al_. The acute retinal necrosis syndrome. Part 1: clinical manifestations.
_Ophthalmology_ 1982; 89(12): 1309–1316. Article CAS Google Scholar * Culbertson WW, Atherton SS . Acute retinal necrosis and similar retinitis syndromes. _Int Ophthalmol Clin_ 1993;
33(1): 129–143. Article CAS Google Scholar Download references ACKNOWLEDGEMENTS There was no financial support or proprietary interest in this work. AUTHOR INFORMATION AUTHORS AND
AFFILIATIONS * AHEPA General Hospital, Thessaloniki, Greece I Tsinopoulos, F Topouzis & P Brazitikos * Department of Ophthalmology, Royal Free Hospital Medical School, Pond Street,
London, NW32QG, UK P Tranos * Radcliffe Infirmary, Oxford, UK K Hundal Authors * I Tsinopoulos View author publications You can also search for this author inPubMed Google Scholar * P Tranos
View author publications You can also search for this author inPubMed Google Scholar * F Topouzis View author publications You can also search for this author inPubMed Google Scholar * K
Hundal View author publications You can also search for this author inPubMed Google Scholar * P Brazitikos View author publications You can also search for this author inPubMed Google
Scholar CORRESPONDING AUTHOR Correspondence to P Tranos. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Tsinopoulos, I., Tranos, P., Topouzis, F. _et
al._ Atypical acute retinal necrosis (ARN) responding to late treatment. _Eye_ 18, 203–204 (2004). https://doi.org/10.1038/sj.eye.6700579 Download citation * Published: 05 February 2004 *
Issue Date: 01 February 2004 * DOI: https://doi.org/10.1038/sj.eye.6700579 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link
Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative