- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
MAIN Sir, Congenital arteriovenous communications or malformations are rare retinal vascular anomalies. We report an unusual juxtapapillary arteriovenous communication of the retina
presenting as an incidental finding in an otherwise healthy individual. CASE REPORT A 41-year-old Caucasian male was referred with a retinal vascular lesion in one eye following a routine
visit to his optometrist. He was asymptomatic with no past ocular history or family history of glaucoma. Five years back a benign lump had been removed from his tongue. His medical history
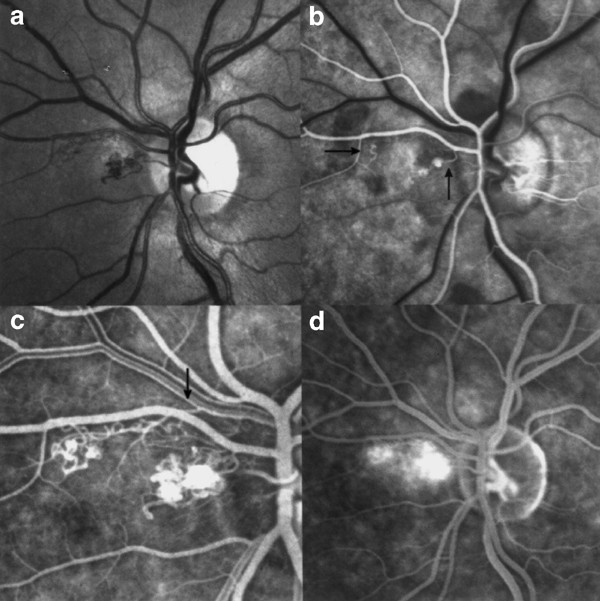
was otherwise unremarkable. Ocular examination revealed a best-corrected visual acuity of 6/5 in both eyes. The anterior segments and intraocular pressures were normal. Fundus biomicroscopy
revealed an unusual juxtapapillary vascular lesion in the left eye (Figure 1a). The right fundus was normal. A fundus fluorescein angiogram demonstrated anomalous vessels of arteriovenous
nature. They were nasal to the optic disc and leaked as the angiogram progressed. No other abnormalities were detected (Figure 1b–d). No vascular malformations were detected in the
conjunctiva, mouth, or tongue. The histology of the lesion that had been removed from the patient's tongue was reviewed. This confirmed the diagnosis of a granular cell myoblastoma,
ruling out the possibility of a second arteriovenous malformation. Full blood count, ESR, blood glucose, and serum lipids were normal. Computerised tomography of the brain and orbits showed
no abnormality. Mitochondrial DNA analysis for Leber's hereditary optic neuropathy (LHON 11 778, 3460, and 14 484) and sequence analysis of exons 1–3 of the Von Hippel–Lindau gene were
negative. The patient has been symptomatically and clinically stable for 1 year and remains under long-term review. COMMENT The patient presents with an unusual unilateral retinal vascular
anomaly as an incidental clinical finding. The presentation, clinical and angiographic appearance is consistent with the diagnosis of a congenital arteriovenous communication group 1.
Congenital arteriovenous malformations or communications were classified into three groups on the basis of severity.1,2 Group 1 consists of an anastamosis between a small arteriole and a
small venule with the interposition of an abnormal capillary or arteriolar plexus. Group 2 demonstrates direct arteriovenous communications between a branch retinal artery and vein. Group 3
consists of diffuse marked dilatation of the vascular tree with many large calibre anastamosing channels. Congenital arteriovenous malformations usually present on routine examination, with
unilateral involvement in single or multiple sites of the same fundus.1,2 They have a predilection for the papillomacular bundle and the superotemporal quadrant. They have rarely been
reported nasal to the optic disc.1,2 Capillary bed leakage within the area of arteriovenous malformation is uncommon but has been described.1 The arteriovenous malformation in this case was
located nasal to the disc and demonstrated leakage on angiography. Ocular complications of arteriovenous malformations include intraretinal haemorrhage, and exudation, aneurysm formation,
vascular occlusion, neovascular glaucoma and vitreous haemorrhage.3 The association of retinal arteriovenous malformations with systemic arteriovenous malformations is well documented.1
Sites of involvement include the central nervous system, orbit, eyelid, oro-naso-pharyngeal area, skin, lung, and spine.1 Group 1 arteriovenous malformations are usually isolated findings
detected on routine examination, non progressive, and associated with good visual acuity.1 Photocoagulation treatment may be indicated if exudative maculopathy develops.3 The differential
diagnosis of congenital arteriovenous malformations includes peripapillary telangiectasia, capillary and cavernous haemangiomas, and retinovascular disease.1 Peripapillary telangiectatic
microangiopathy is well described in LHON.4 The microangiopathy precedes the optic neuropathy, and the telangiectatic vessels do not demonstrate leakage on angiography.5 In nearly all
families, LHON is associated with one of three mitochondrial DNA (mtDNA) mutations, at base pairs 11 778, 3460, or 14 484.6 Mitochondrial DNA analysis in this patient was negative. Retinal
capillary haemangiomas may be sporadic or occur as a part of Von Hippel–Lindau's disease.7 Clinically, these often present with exudative features and show arteriovenous shunting.8
These features were absent in this patient and genetic testing was negative. Cavernous haemangioma is a rare unilateral congenital anomaly located between two retinal veins and presenting
with the typical appearance of a cluster of grapes.9 Arteriovenous malformations should also be distinguished from acquired optic disc venous collaterals secondary to retinal venous
occlusion or optic disc meningioma.3 The clinical and fluorescein angiogram findings, normal CT scan of the brain and orbits, and negative genetic screening all point in favour of a
congenital arteriovenous malformation. The atypical features in this case are the location of the arteriovenous malformation, which was nasal to the disc, and the leakage of dye on
angiography. REFERENCES * Mansour AM, Walsh JB, Henkind P . Arteriovenous anastamoses of the retina. _Ophthalmology_ 1987; 94: 35–40. Article CAS Google Scholar * Archer DB, Deutman A,
Ernest JT, Krill AE . Arteriovenous communications of the retina. _Am J Ophthalmol_ 1973; 75: 224–241. Article CAS Google Scholar * Gass JDM . _Stereoscopic Atlas of Macular Disease
Diagnosis and Treatment_, VOL. 1. Mosby: St Louis, 1997; pp 440–442. Google Scholar * Nikoskelainen E, Hoyt WF, Nummelin K, Schatz H . Fundus findings in Leber's hereditary optic
neuroretinopathy III. Fluorescein angiographic studies. _Arch Ophthalmol_ 1984; 102(7): 981–989. Article Google Scholar * Nikoskelainen E, Hoyt WF, Nummelin K . Ophthalmoscopic findings in
Leber's hereditary optic neuropathy. II. The fundus findings in the affected family members. _Arch Ophthalmol_ 1983; 101(7): 1059–1068. Article Google Scholar * Chalmers RM, Schapira
AH . Clinical, biochemical and molecular genetic features of Leber's hereditary optic neuropathy. _Biochem Biophys Acta_ 1999; 1410(2): 147–158. Google Scholar * Webster AR, Maher ER,
Bird AC, Gregor ZJ, Moore AT . A clinical and molecular genetic analysis of solitary ocular angioma. _Ophthalmology_ 1999; 106(3): 623–629. Article Google Scholar * Gass JDM .
_Stereoscopic Atlas of Macular Disease Diagnosis and Treatment_, VOL. 2. Mosby: St Louis, 1997, pp 850–857. Google Scholar * Kushner MS, Jampol LM, Haller JA . Cavernous hemangioma of the
optic nerve. _Retina_ 1994; 14: 359–361. Article CAS Google Scholar Download references ACKNOWLEDGEMENTS We acknowledge Dr PJS Dunn of the Department of Histopathology, Worcester Royal
Infirmary; Dr John Harry of the Birmingham and Midland Eye Centre and the Medical Illustration Department of City Hospital; and Birmingham Midland Eye Centre, City Hospital for medical
illustration. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Birmingham Midland Eye Centre, City Hospital, Dudley Rd, Birmingham, B18 7QH, UK S Chatterjee, M Hope-Ross & IH Clark *
Worcestershire Royal Hospital, Charles Hastings Way, Worcester, WR1 3AS, UK PB Chell Authors * S Chatterjee View author publications You can also search for this author inPubMed Google
Scholar * M Hope-Ross View author publications You can also search for this author inPubMed Google Scholar * IH Clark View author publications You can also search for this author inPubMed
Google Scholar * PB Chell View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to M Hope-Ross. RIGHTS AND PERMISSIONS
Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Chatterjee, S., Hope-Ross, M., Clark, I. _et al._ A rare and unusual congenital arteriovenous communication of the retina. _Eye_
18, 74–75 (2004). https://doi.org/10.1038/sj.eye.6700375 Download citation * Published: 06 January 2004 * Issue Date: 01 January 2004 * DOI: https://doi.org/10.1038/sj.eye.6700375 SHARE
THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to
clipboard Provided by the Springer Nature SharedIt content-sharing initiative