- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
KEY POINTS * Discusses the causes of root resorption. * Summarises radiographic techniques commonly used in orthodontics with particular reference to root resorption. * Illustrates the
limitations of the three commonly used radiographic views: the upper standard occlusal, DPT and true cephalometric lateral skull radiograph when used for such purposes. * Suggests that the
paralleling techniques should be used when serial assessments of resorption are to be made over time. ABSTRACT The literature regarding external root resorption in relation to orthodontics
and its radiographic diagnosis is reviewed, including a summary of the more common radiographic techniques available. Sample cases are presented which demonstrate the need for good
radiographic technique and an awareness of the limitations of certain radiographs. A provisional diagnosis of external root resorption may need to be confirmed by further radiographic views
where appropriate. You have full access to this article via your institution. Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS EXTERNAL CERVICAL RESORPTION—A REVIEW OF PATHOGENESIS AND
POTENTIAL PREDISPOSING FACTORS Article Open access 10 June 2021 MANAGEMENT OF RARELY SEEN INTERNAL TUNNELLING ROOT RESORPTION ASSOCIATED WITH A MAXILLARY PERMANENT INCISOR Article Open
access 28 June 2024 THE ORTHODONTIC-ENDODONTIC INTERFACE: TRAUMA AND PULPAL CONSIDERATIONS Article Open access 13 September 2024 MAIN Resorption of the roots of the permanent teeth is a
pathological process originating either internally or externally. It develops when the natural protection of the predentine and odontoblasts in the root canal, or the precementum and
cementoblasts on the root surface are damaged or removed. Orthodontic forces are just one of several aetiological factors that have been implicated in external root resorption. Other
aetiological factors include reimplantation, trauma, pressure from adjacent unerupted teeth and related pathological conditions such as odontogenic and non-odontogenic tumours. Andreason1
has subclassified external root resorption into 3 subgroups: * Surface resorption * Inflammatory resorption * Replacement (ankylosis) resorption External resorption associated with
orthodontic forces is typically surface resorption and is most commonly found in the apical region of the roots causing them to become shorter. Repair with new cementum and periodontal
fibres, with recontouring of the root, usually occurs rapidly after the causative factors have been removed. External surface root resorption has long been recognised as an unwanted sequel
of orthodontic tooth movement,2 with some of this type of root resorption almost inevitably occurring during orthodontic treatment involving the use of fixed appliances.3,4 Such resorption
tends to follow the application of a force to a tooth, sufficient to cause hyalinisation, or aseptic necrosis, of its periodontal ligament.5,6 Whereas in some patients only small areas of
surface resorption occur, in others it can be much more extensive, with the amount lost being unpredictable and irreversible. Microscopic signs of external resorption are very common, even
in non-orthodontically treated teeth,7 but following orthodontic treatment, macroscopic evidence of resorption has been reported in up to 40% of adults and 16.5% of children.8 Schwartz9
reported that when the pressure decreases below the threshold for optimal tooth movement, external surface root resorption ceases. Other workers have also found such macroscopic resorption
stops on completion of orthodontic treatment.10,11 Factors suggestive of a tooth being more susceptible to external root resorption include short roots, roots which are abnormally shaped
(blunt or pipette-shaped) and roots already showing resorption.12,13 Traumatised teeth are only more prone to resorption if they show signs of pre-treatment resorption.14 Previously root
treated teeth on the other hand are thought to be less prone.8 Functionally root resorption is of importance, as recent work15 has suggested that roots less than 9 mm in length will lead to
increased tooth mobility, although the effects in the longer term are not known. Radiographs are required before the start of orthodontic treatment for the assessment of general dental
health, including root form and the presence or absence of any underlying disease, and to show the position and number of developing teeth.16 The dental panoramic tomograph (DPT) is widely
regarded as a valuable tool for these purposes, as it provides an overall view of the entire dentition and yet the patient is subjected to a lower radiation dose than from a full-mouth
series of intra-oral radiographs.17 The British Orthodontic Society _Radiography Guidelines_18 states that an upper standard occlusal radiograph may be necessary to supplement the panoramic
tomograph. This is because the focal trough of the tomograph is narrow in the incisor region, sometimes causing the apices and palatal structures to be out of focus or even invisible.
Periapical views or an upper standard occlusal are therefore recommended to be taken in addition to the dental panoramic tomograph when there is a clinical indication, such as suspected
underlying midline pathology or developmental anomaly.19 RADIOGRAPHIC TECHNIQUES INTRAORAL RADIOGRAPHS Intraoral radiographs of the teeth should be geometrically accurate. The idealised
positioning requirements are shown in Figure 1 and include: * The tooth/teeth under investigation and the film packet should be in contact or, if not feasible, as close together as possible
* The tooth/teeth and the film packet should be parallel to one another * The X-ray tubehead should be positioned so that the beam meets the tooth and the film at right angles in both the
vertical and horizontal planes * The positioning should be reproducible – particularly if the films are to be used for comparative purposes. For periapical radiography two techniques exist –
the paralleling technique and the bisected angle technique. As the name implies, with the paralleling technique the film packet is placed in a holder and positioned parallel to the
tooth/teeth under investigation. The X-ray tubehead is then aimed at right angles (vertically and horizontally) to both the teeth and film packet as shown in Figure 2. The resultant films
are geometrically accurate and are the views of choice for assessing external root resorption. By using a film holder, with fixed film packet and X-ray tubehead positions, the technique is
reproducible and thus sequential films can be used for comparative purposes to assess the progression of resorption. Two examples of films taken with the paralleling technique are shown in
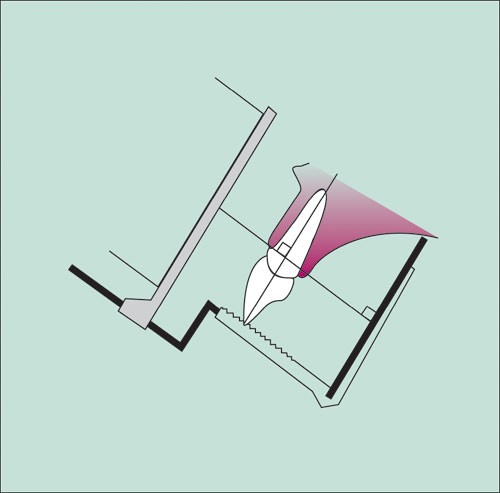
Figures 3a and 3b. In the bisected angle technique the film packet is placed as close as possible to the tooth/teeth under investigation without bending the film packet. The angle between
the long axes of the tooth and film is bisected and the X-ray beam is aimed at right angles to this line, through the apex of the tooth as shown in Figure 4. With this geometrical
arrangement the length of the tooth in the mouth is equal to the length of the tooth on the film, but incorrect vertical tubehead positioning can cause either foreshortening or elongation of
the image as shown in Figure 5. The many variables involved with this technique means that it is not usually possible to obtain reproducible views. Thus, bisected angle technique
periapicals are not ideal for the radiographic assessment of the amount of external root resorption, particularly over time. The upper standard occlusal radiograph shows the anterior part of
the maxilla and the upper anterior teeth on one film. It can therefore demonstrate on one film the presence or absence of supernumeraries, supplementals or odontomes, as well as allowing
examination of root form and any underlying disease such as external root resorption of the upper incisor teeth. However, the upper standard occlusal radiograph is in effect a large bisected
angle technique periapical as shown in Figure 6. It is therefore subject to the same disadvantages and distortion. As a result, considerable caution needs to be exercised if this view is
used to assess external root resorption. DIGITAL RADIOGRAPHY Digital radiography is a relatively recent development in dentistry enabling the film packet to be replaced with a digital image
receptor. Two types of receptors have been developed – CCD (charge coupled device) sensors and photo-stimulable phosphor imaging plates. Both systems have intraoral receptors suitable for
periapical radiography but only photo-stimulable phosphor plates have been produced for occlusal radiography. Digital radiography has been shown to demonstrate a similar degree of
sensitivity to film-based radiography in the detection of resorption, but with a lower radiation dose.20 However, the geometric relationship of the digital receptor, tooth and X-ray beam is
just as important as in conventional radiography if geometric distortion is to be avoided. Digital images have the additional advantages that they can be manipulated including enlargement,
contrast enhancement, inversion and pseudo-colouration which may prove to be an advantage when assessing external root resorption. DENTAL PANORAMIC TOMOGRAPH (DPT) The dental panoramic
tomograph is a sectional radiograph and only structures that are within the section will be evident and in focus on the film. This in focus section, or focal trough, is approximately the
same shape as the dental arch and resembles a three dimensional horse-shoe shape. During an exposure the X-ray tubehead orbits around the back of the patient's head while the film moves
past the face. A narrow slit X-ray beam is used which is aimed upwards at approximately 8° to the normal, as shown in Figure 7. The shape of the curved focal trough is pre-determined and
patients have to be positioned carefully within the machine to ensure that their teeth and the supporting structures appear in focus on the resultant film. Incorrect positioning results in a
distorted image with teeth appearing foreshortened, magnified and/or out of focus depending on the positioning error. In addition, normal anatomical structures can appear as radiolucent or
radiopaque shadows superimposed over the teeth as either real or actual shadows or as ghost or artefactual shadows all of which can degrade the quality of the final image.21 In orthodontic
patients, another common problem is one of skeletal base discrepancy. In markedly class II or class III cases, it may not be possible to position both the upper and lower labial segment
teeth within the focal trough of the machine simultaneously as shown in Figure 8. Roots that are outside the focal trough and are positioned lingually/palatally to it may appear magnified.
In addition to skeletal problems, teeth may be outside the focal trough if excessively proclined or retroclined. This can occur in either the upper or lower arches, or both as illustrated in
Figure 8b. In this case the main effect may be to foreshorten the final image. In such instances supplemental intraoral views are indicated to cover the region that is out of focus. In view
of the effect that incorrect patient positioning can have on the accuracy and definition of the final DPT image, considerable caution needs to be exercised when interpreting these films and
relying on them to assess external root resorption. TRUE CEPHALOMETRIC LATERAL SKULL The true cephalometric lateral skull radiograph provides an accurate and reproducible view of the length
of the upper incisors. However, this is likely to be subjected to a 5–12 % enlargement factor as a result of the radiographic set up, i.e. X-ray tubehead to patient and patient to film
distance as shown in Figure 9. In addition, superimposition of one side on the other may make the image unclear, particularly for the detailed assessment of external root resorption.
ILLUSTRATIVE CASES These cases are presented to illustrate the limitations of a single radiographic view when assessing external surface root resorption in relation to orthodontics CASE 1 At
first glance the DPT for this patient suggested that there may have been localised external root resorption present on the upper central incisor teeth (Fig. 10a), but this was contradicted
by the upper standard occlusal radiograph (Fig. 10b) where geometrical distortion has resulted in the teeth appearing elongated. The true cephalometric lateral skull (Fig. 10c) confirmed
that the roots of the upper central incisors were indeed short and this was considered to be the definitive view, as it is more reliable and not subject to the distortions inherent with the
other techniques. This proved to be an orthodontic diagnostic dilemma since the patient had severe upper arch crowding. As part of the extraction pattern the upper central incisors were
extracted, the upper laterals moved towards the midline and the upper canines aligned. Another problem of the DPT in this instance is the band of radiolucency over the apices of the upper
teeth due to the air between the tongue and the palate. Patients should ideally be asked to press their tongue against the palate during the taking of the DPT. CASE 2 The DPT for this
patient (Fig. 11a) again suggested apparent external root resorption. The upper standard occlusal radiograph (Fig. 11b) was not consistent with this finding. Upon closer examination, it can
be seen that the patient has been slightly incorrectly positioned in the machine during the taking of the DPT. The patient's chin has been raised too high as evidenced by the flatness
of the occlusal plane and of the mandible on the resulting film. This positioning error can lead to the apices of the maxillary anterior teeth being outside the focal trough, and the
angulation of the teeth to the X-ray beam leads to foreshortening of the image giving the appearance of short roots. However, although the true cephalometric lateral skull (Fig. 11c) did not
provide a good view of the apices of the upper incisors, it does illustrate the degree of proclination of the upper incisors. This would have been the main factor responsible for the
radiographic appearance of short roots. The upper standard occlusal view was felt to be the most informative in this case. CASE 3 This case was transferred from an orthodontist in Germany
and presented in mid-treatment. There was a lower fixed appliance present and the patient had intermittently worn an upper removable expansion appliance, but had ceased wearing this due to
discomfort and 'wobbly' teeth. The referring practitioner had supplied a pre-orthodontic DPT of reasonable quality (Fig. 12a), which showed no evidence of external root resorption.
A mid-treatment DPT was obtained prior to continuing treatment, in view of the complaint of "wobbly" teeth, which revealed, what initially appeared to be, severe external root
resorption of the upper central incisors (Fig. 12b). None of the other teeth showed signs of shortened roots on this second DPT. As in case 2, closer examination reveals the patient to have
been incorrectly positioned during the taking of the second radiograph. The chin has again been raised slightly too high, the patient is also positioned too far away from the film (as
evidenced by the mesio-distal magnification of the upper and lower incisor crowns). These positioning faults result in the apices being outside the focal trough and thus seemingly resorbed.
An upper standard occlusal radiograph taken at the same time showed the roots of the upper incisors to be unaffected (Fig. 12c) and it was felt the patient would be able to continue
treatment with an upper fixed appliance. This was confirmed on a later true cephalometric lateral skull (Fig. 12d), which also showed the incisor proclination that would contribute to the
upper incisors being outside the focal trough. The sample cases illustrate the ease with which it is possible to make an erroneous diagnosis of root resorption, its presence or absence,
based on radiographs which do not adequately demonstrate the area of interest. This can be either because of poor radiographic technique or because of the inherent limitations of the chosen
view(s). Knowledge of the techniques and their limitations is therefore essential when assessing external root resorption. In the cases described the limitations of the DPT were principally
caused by the proclination of the upper incisor teeth and the patients being incorrectly positioned within the machine. Malposition of the teeth may make it impossible to position the teeth
accurately within the narrow focal trough. Previous work looking at the role of the upper standard occlusal radiograph and DPT has shown the latter to be affected by the degree of both upper
and lower incisor proclination.22 Indeed, in the same work, of the 3 cases of root resorption seen in the 100 cases studied, the DPT had falsely indicated resorption in 2 of the cases,
which was not subsequently seen on the upper standard occlusal radiograph. The cases presented here clearly show the resultant image distortion and how diagnostic interpretation of external
root resorption was also compromised. The true cephalometric lateral skull radiograph is one of the most accurate ways of determining the root length of the upper incisors, but detailed
diagnosis of external root resorption is often not possible as a result of superimposition of adjacent tooth roots, in particular the maxillary lateral and canine teeth, as shown in case 2.
The upper standard occlusal is a good view for showing the anterior part of the maxilla but upper incisor root length will be greatly affected by the geometrical set-up when the film is
taken. Ideally, paralleling technique periapicals, as shown in Figures 3a and 3b, should be used to minimise the effects of geometrical distortion, which would otherwise lead to apparent
lengthening or shortening of the roots, particularly if resorption is to be monitored over time with repeat radiographs. CONCLUSIONS The cases presented highlight the potential problems and
limitations of using a dental panoramic tomograph for pre-orthodontic assessment and the need for vigilance in the correct patient positioning during radiographic exposure. The narrow focal
trough in the anterior portion of the maxilla presents a particular problem for many orthodontic patients with abnormally positioned or proclined incisors. The apices of the upper incisors
may not be shown and the appearance can mimic root resorption, while supernumerary and/or unerupted teeth may not be detected. Supplementary views may therefore be necessary whenever there
is any doubt that the dental panoramic tomograph demonstrates the necessary detail in this region. Paralleling technique periapicals are the intraoral views of choice but if unavailable an
upper standard occlusal can demonstrate the anterior maxilla but the image may be geometrically inaccurate. The true cephalometric lateral skull can be used to assess incisor root length,
but not for detailed diagnosis of external root resorption. In order to correctly assess the degree of external root resorption care should be taken to employ the radiographic technique(s)
that ensure geometrically accurate images. In some instances it may be necessary to take more than one radiograph. REFERENCES * Andreasen J O . External root resorption: its implications in
dental traumatology, paedodontics, periodontics, orthodontics and endodontics. _Int J Endodontics_ 1985; 18: 109–118. Article Google Scholar * Bates S . Absorption. _Br J Dent Science_
1856; 1: 256. Google Scholar * Brezniak N, Wasserstein A . Root resorption after orthodontic treatment: Part 1. Literature review. _Am J Orthod Dentofacial Orthop_ 1993; 103: 62–66. Article
Google Scholar * Brezniak N, Wasserstein A . Root resorption after orthodontic treatment: Part 2. Literature review. _Am J Orthod Dentofacial Orthop_ 1993; 103: 138–146. Article Google
Scholar * Rygh P . Orthodontic root resorption studied by electron microscopy. _Angle Orthod_ 1977; 47: 1–16. PubMed Google Scholar * Reitan K . Initial tissue behaviour during apical
root resorption. _Angle Orthod_ 1974; 44: 68–82. PubMed Google Scholar * Henry J L, Weinmann J P . The pattern of root resorption and repair of human cementum. _J Am Orthod Assoc_ 1951;
42: 270–290. Google Scholar * Mirabella A D, Årtun J . Prevalence and severity of apical root resorption of maxillary anterior teeth in adult orthodontic patients. _Eur J Orthod_ 1995; 17:
93–99. Article Google Scholar * Schwartz A M . Tissue changes incidental to tooth movement. _Int J Orthod_ 1980; 18: 331–352. Google Scholar * Copeland S, Green L J . Root resorption in
maxillary incisors following active orthodontic treatment. _Am J Orthod_ 1986; 89: 51–55. Article Google Scholar * Remington D, Joondeph D R, Årtun J, Riedel R A, Chapko M K . Long term
evaluation of root resorption occurring during orthodontic treatment. _Am J Orthod_ 1986; 96: 43–46. Article Google Scholar * Linge B O, Linge L . Evaluation of the risk of root resorption
during orthodontic treatment: a study of upper incisors. _Eur J Orthod_ 1983; 5: 173–183. Article Google Scholar * Levander E, Malmgren O . Apical root resorption in upper anterior teeth.
_Eur J Orthod_ 1988; 10: 30–38. Article Google Scholar * Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, Ludberg M . Root resorption after orthodontic treatment of traumatised teeth.
_Am J Orthod_ 1982; 82: 487–491. Article Google Scholar * Levander E, Malmgren O . Long-term follow-up of maxillary incisors with severe apical root resorption. _Eur J Orthod_ 2000; 22:
85–92. Article Google Scholar * Smith N J D . Orthodontic radiology: a review. _Int Dent J_ 1987; 37: 16–24. PubMed Google Scholar * McNicol A, Stirrups D R . Radiation dose during the
dental radiographic techniques most frequently used during orthodontic treatment. _Eur J Orthod_ 1985; 7: 163–171. Article Google Scholar * Isaacson K G, Jones M L . _Orthodontic
Radiography Guidelines_ British Orthodontic Society, 1st ed, 1994. Google Scholar * Ferguson J W, Evans R I, Cheng L H . Diagnostic accuracy and observer performance in the diagnosis of
abnormalities in the anterior maxilla: a comparison of panoramic with intraoral radiography. _Br Dent J_ 1992; 173: 265–271. Article Google Scholar * Borg E, Kallqvist A, Grondahl K,
Grondahl H G . Film and digital radiography for detection of simulated root resorption cavities. _Oral Surg, Oral Med, Oral Path, Oral Radiol, Endod_ 1998; 86: 110–114. Article Google
Scholar * Whaites E . _Essentials of Dental Radiography and Radiology_. Churchill Livingstone, 2nd ed. 1996. Google Scholar * Giles S A, Taylor N G . Are anterior occlusal radiographs
still indicated for orthodontic assessment? _Br Dent J_ 1997; 183: 325–328. Article Google Scholar Download references ACKNOWLEDGEMENTS The authors would like to thank Helen Knight for her
assistance in the management of one of the cases described, and to thank Churchill Livingstone for their permission to reproduce Figures 1,2, 4,5,6,7,8,9 from Whaites' 'Essentials
of Dental Radiography and Radiology' 2nd Ed. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Specialist Registrar, Department of Child Dental Health, Bristol Dental Hospital, Lower
Maudlin St., Bristol, BS1 2LY H A Leach * Consultant Orthodontist, Orthodontic Department, Royal United Hospital, Combe Park, Bath, BA1 3NG A J Ireland * Senior Lecturer and Honorary
Consultant, Dental Radiology Department, Guy's, King's and St Thomas' (GKT) Dental Institute, London, SE1 9RT E J Whaites Authors * H A Leach View author publications You can
also search for this author inPubMed Google Scholar * A J Ireland View author publications You can also search for this author inPubMed Google Scholar * E J Whaites View author publications
You can also search for this author inPubMed Google Scholar ADDITIONAL INFORMATION REFEREED PAPER RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Leach,
H., Ireland, A. & Whaites, E. Radiographic diagnosis of root resorption in relation to orthodontics. _Br Dent J_ 190, 16–22 (2001). https://doi.org/10.1038/sj.bdj.4800870 Download
citation * Received: 27 March 2000 * Accepted: 07 August 2000 * Published: 13 January 2001 * Issue Date: 13 January 2001 * DOI: https://doi.org/10.1038/sj.bdj.4800870 SHARE THIS ARTICLE
Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided
by the Springer Nature SharedIt content-sharing initiative