- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
In this study, we present the clinicopathologic features and immunophenotypic characteristics of five cases of uterine tumors resembling ovarian sex cord tumors and three cases of
endometrial stromal tumors with sex cord-like elements, with emphasis on immunohistochemical markers of sex cord differentiation. The mean patient age was 42 years (range 19–69 years), and
vaginal bleeding was the most common clinical presentation. The tumors were usually polypoid masses arising in the uterine fundus, with a mean tumor size of 6.7 cm. Sex cord patterns in
uterine tumors resembling ovarian sex cord tumors, including anastomosing cords, trabeculae, small nests, tubules, and in one case, a striking retiform architecture with Leydig-like cells,
comprised from 70 to 100% of the tumor volume. All uterine tumors resembling ovarian sex cord tumors were positive for two or more markers of sex cord differentiation; all five cases showed
strong immunoreactivity for calretinin, with coexpression of CD99 (four cases), Melan-A (two cases), and inhibin (two cases). Endometrial stromal tumors with sex cord-like elements were less
frequently positive for markers of sex cord differentiation, with each case positive for one marker (calretinin, two cases; CD99, one case). In addition, all eight cases were frequently
positive for cytokeratin, CD10, vimentin, estrogen receptor, and progesterone receptor; desmin immunoreactivity, when present, was limited to minor foci of smooth muscle. Overall, the
morphologic and immunohistochemical findings in uterine tumors resembling ovarian sex cord tumors strongly support that these unusual uterine tumors are polyphenotypic neoplasms with true
sex cord differentiation.
Uterine tumors resembling ovarian sex cord tumors (UTROSCT) are an unusual group of stromal neoplasms exhibiting prominent sex cord-like differentiation. In their initial description almost
30 years ago, UTROSCT were designated as Group II tumors, characterized by benign behavior, to distinguish them from endometrial stromal tumors with sex cord-like elements (ESTSCLE; Group I
tumors) which were associated with increased risk of recurrence and metastasis.1 UTROSCT are placed in the miscellaneous category in the most recent World Health Organization classification
of tumors of the uterine corpus,2 although most investigators consider these rare neoplasms to be variants of endometrial stromal tumors.3
UTROSCT show a predominant, if not exclusive, pattern of cords, nests, and trabeculae resembling granulosa or Sertoli cell tumors of the ovary, while ESTSCLE contain focal sex cord-like
areas in a background of an otherwise typical endometrial stromal nodule or endometrial stromal sarcoma. True Leydig cell differentiation has not been described in these tumors, although
some cases have been observed to contain luteinized-like cells with abundant eosinophilic or foamy cytoplasm.4, 5, 6, 7 Numerous immunohistochemical and ultrastructural studies have
attempted to phenotype the sex cord-like cells in UTROSCT and ESTSCLE, with variable evidence supporting myoid,8, 9, 10, 11, 12, 13, 14 epithelial,4, 15 and true sex cord differentiation.6,
7, 16, 17, 18, 19, 20 Specifically, inhibin and CD99,3, 6, 7, 14, 17, 18, 19, 20, 21 as well as Melan-A,19, 21 and most recently, calretinin,7, 20 have been utilized as immunohistochemical
markers of sex cord differentiation in UTROSCT and ESTSCLE based on application of these markers to sex cord–stromal tumors of the ovary.22, 23, 24, 25, 26, 27, 28, 29
The present study was initiated following the diagnosis of a UTROSCT exhibiting a striking retiform pattern and Leydig-like stromal cells, indistinguishable from a Sertoli–Leydig cell tumor
of the ovary. This index case prompted an immunohistochemical and clinicopathologic study of UTROSCT and ESTSCLE, with emphasis on the more recently used markers of sex cord differentiation.
We sought to determine the diagnostic utility of these and other markers and to contribute to the understanding of the phenotype and behavior of these unusual tumors.
Five UTROSCT and three ESTSCLE were retrieved from the consultation files of one of the authors (JP). Clinical information, including presenting symptom, surgery, adjuvant therapy, and
patient outcome was obtained from the contributing pathologists and gynecologists. All available pathology reports were examined and the diagnosis confirmed in each case by review of
hematoxylin- and eosin-stained slides. Tumors were evaluated for approximate proportions of sex cord, endometrial stromal, and smooth muscle elements; tumors with predominant (>50%) or minor
(≤50%) sex cord differentiation were diagnosed as UTROSCT and ESTSCLE, respectively. Other histologic parameters including infiltrative margins, vascular invasion, nuclear atypia, mitotic
index, and necrosis were also assessed.
Immunohistochemistry was performed on all eight cases for calretinin, melan A, CD99, inhibin, CD10, desmin, cytokeratin (CAM 5.2), vimentin, estrogen receptor, and progesterone receptor.
Sources and dilutions of these antibodies are provided in Table 1. Heat-induced antigen retrieval was conducted by immersion of the sections in sodium citrate buffer (0.01 M sodium-citrate
monohydrate, pH 6.0) or EDTA buffer (pH 8.0) and incubation in an autoclave (Matachana, Barcelona, Spain) at 120°C for 10 min. The immunohistochemical reactions were performed in a Dako
TechMate Horizon immunostainer and visualized following the EnVision system with diaminobenzidine as the chromogen. Immunohistochemical staining was graded as 0 (negative), 1+ (50% positive
cells). Positive tissue control and negative control slides, the latter performed by omission of the primary antibody, were included with each batch of immunohistochemical slides.
The clinicopathologic features for all eight cases are presented in Tables 2 and 3. The mean patient age was 42 years (range 19–69 years); the most common clinical presentation was vaginal
bleeding (data not shown). Patients underwent total abdominal hysterectomy and bilateral salpingo-oophorectomy (four cases) or simple hysterectomy (four cases). Evidence of extrauterine
spread was present in one patient with ESTSCLE.
Most tumors were polypoid or nodular masses, usually located in the uterine fundus, with a mean tumor size of 6.7 cm (range 3.5–14 cm). Infiltrative margins were noted in two UTROSCT and in
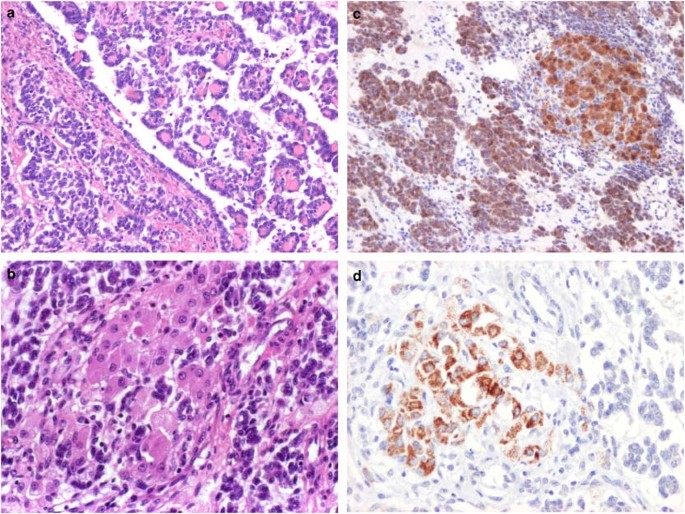
two ESTSCLE. Microscopically, two UTROSCT consisted exclusively of sex cord elements; one of these, the index case (case 1), exhibited a striking retiform pattern, with many small papillae
showing hyalinized cores lined by cuboidal cells (Figure 1a). Discrete nodules of polygonal, Leydig-like cells with abundant eosinophilic cytoplasm and round nuclei were scattered throughout
the tumor (Figure 1b). Crystals of Reinke were not identified. In the remaining cases, sex cord patterns in both UTROSCT and ESTSCLE were variable but most commonly consisted of thin
anastomosing cords, trabeculae, small nests, and tubules (Figure 2a and b). Cells typically had scant cytoplasm and round to oval nuclei with indistinct nucleoli.
UTROSCT (Case 1) with a striking retiform pattern composed of small papillae with hyalinized cores projecting into larger cyst (a) and clusters of Leydig-like cells (b). Irregularly
branching, slit-like tubules were seen elsewhere. The tumor cells were strongly positive for calretinin (c). Melan-A immunoreactivity in Leydig-like cells is shown in (d).
UTROSCT (Case 4) with anastomosing cords and nests of cells (a, b) and occasional small nodules of smooth muscle (a). Foci of scattered foam cells were present (c). The tumor cells showed
strong immunoreactivity for calretinin (d) and CD99 (e); less than 10% of cells were inhibin positive (f).
Five tumors (3/5 UTROSCT and 2/3 ESTSCLE) contained a mature smooth muscle component, in four cases consisting of occasional small nodules and fascicles of cells interspersed between the sex
cord areas (Figure 2a). One ESTSCLE (case 7) showed focal areas with a starburst pattern of cells surrounding a central hyalinized core. One UTROSCT contained scattered foam cells,
consisting of single cells and small aggregates of cells with round, central nuclei and abundant clear to foamy cytoplasm (Figure 2c). Minor foci of endometrial stromal-type cells were
evident in one UTROSCT, arranged in ill-defined, cellular clusters merging with the adjacent sex cord areas. The stromal cells had minimal cytoplasm, with small, oval nuclei and even
chromatin.
Nuclear atypia was mild to moderate in all eight cases. The mitotic index was low in the UTROSCT group, ranging from one to three mitoses per 10 high-power fields, and up to six mitoses per
10 high-power fields in the ESTSCLE group. Necrosis was present only in the largest tumor of the series (case 7). Vascular invasion was present in all three ESTSCLE but in only one UTROSCT.
Of the three ESTSCLE, two tumors demonstrated usual low-grade endometrial stromal sarcoma; one case consisted of high-grade stromal sarcoma (case 7).
The immunohistochemical profile of each case and their relative proportions of sex cord, endometrial stromal, and smooth muscle elements are given in Table 4. Each of the five UTROSCT cases
were immunoreactive for two or more markers of sex cord differentiation. All five UTROSCT were strongly immunoreactive for calretinin, with coexpression of CD99 in four cases, melan-A in two
cases, and inhibin in two cases. The index UTROSCT case showed immunoreactivity for calretinin (Figure 1c) and melan-A (Figure 1d) in both the Sertoli- and Leydig-like components, while
only the latter was positive for inhibin. Three of the remaining UTROSCT cases and all three ESTSCLE were inhibin negative. In case 4, the sex cord cell and foam cell components showed
immunoreactivity for calretinin, CD99, and inhibin (Figures 2d–f). Immunohistochemical staining for calretinin was present in two of three ESTSCLE but with less intensity than that observed
in the UTROSCT group. All three ESTSCLE were negative for Melan A; one case was immunoreactive for CD99.
CD10 was variably positive in 4/5 UTROSCT and strongly positive in 2/3 ESTSCLE. Of the five cases with desmin immunoreactivity, four showed positive staining only in the smooth muscle
component. All eight cases were strongly immunoreactive for vimentin, and the majority (6/8 cases) were cytokeratin positive. Three UTROSCT showed ER immunoreactivity, in two cases
restricted to the sex cord elements, while four UTROSCT were PR positive. Two ESTSCLE were positive for both ER and PR.
Information regarding adjuvant therapy and clinical follow-up was available for seven patients (Table 2). For four patients with UTROSCT, three received no additional treatment and one
underwent pelvic radiotherapy with brachytherapy to the vaginal vault; all four patients were alive without evidence of disease at a mean of 3.5 years. The fourth patient (case 3) had no
residual tumor in the hysterectomy specimen and was subsequently lost to follow-up. Of the three patients with ESTSCLE, two received no additional therapy and are without evidence of disease
at 1 year 3 months and 2 years. The third patient (case 7) received chemotherapy but developed pulmonary and bony metastases and died of disease 10 months from the operative date.
Since the initial description of UTRSOCT in 1976, there have been numerous efforts to further characterize this unusual group of uterine neoplasms. Results have been variable, with
ultrastructural and immunohistochemical evidence of myogenic, epithelial, and sex cord differentiation.6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 In the present study, we applied
a panel of antibodies, inclusive of the most recently identified markers of sex cord differentiation (calretinin, melan A, CD99, and inhibin) as well as smooth muscle and endometrial
stroma, to a series of UTROSCT and ESTSCLE. We found that all UTROSCT were immunoreactive for at least two markers of sex cord differentiation, often with coexpression of cytokeratin, CD10,
vimentin, estrogen receptor, and progesterone receptor; desmin immunoreactivity, when present, was restricted to minor foci of smooth muscle. Our results support that UTROSCT are
polyphenotypic neoplasms with true sex cord differentiation. As shown in Table 5, our data are in general agreement with previous studies addressing the issue of immunohistochemical
expression of sex cord markers in UTROSCT6, 7, 14, 17, 18, 19, 20, 21, 24, 30 and is the first to concurrently examine the four most commonly used markers. This literature review also
highlights that ESTSCLE, or Type I tumors, less frequently show immunoreactivity for markers of sex cord differentiation, a finding which correlates with their morphologic appearance and
relatively minor component of sex cord elements.6, 14, 18
Of the five UTROSCT analyzed in this study, the proportion of sex cord elements comprised between 70 and 100% of the tumor volume, based on routine microscopic evaluation. In most cases, the
sex cord formations consisted of thin cords, trabeculae, and nests of cells; in the index case, a striking retiform pattern with interspersed clusters of eosinophilic Leydig-like cells was
present, indistinguishable from an ovarian Sertoli–Leydig cell tumor. Eosinophilic cells resembling luteinized stromal cells have been described,6, 7 as well as foam cells,1, 4, 6, 7 both of
which have shown strong inhibin and CD99 immunoreactivity.6, 7 In our index UTROSCT case, composed exclusively of sex cord elements, inhibin immunoreactivity was restricted to the
Leydig-like cell component, while calretinin and Melan-A were diffusely positive. The morphology and immunophenotype of foam cells, eosinophilic ‘luteinized’ cells, and Leydig-like cells
suggests that they represent a spectrum of variably differentiated sex cord cells. Indeed, some authors have suggested that these cells may have steroid-producing function, although this
remains speculative at present.7
Overall, calretinin was the most consistently expressed sex cord marker, present in >50% of cells in all five UTROSCT and in two of three ESTSCLE (





![[withdrawn] doing business in sweden: sweden trade and export guide](https://www.gov.uk/assets/static/govuk-opengraph-image-03837e1cec82f217cf32514635a13c879b8c400ae3b1c207c5744411658c7635.png)

