- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
… BUT WIDEN THE SEARCH IF YOU MUST The nursing home industry has lost 15 percent of its workforce since March 2020, according to federal figures. Many facilities have limited resident
populations to maintain the quality of their care, says Holly Harmon, senior vice president at the American Health Care Association and the National Center for Assisted Living (AHCA/NCAL), a
joint organization that represents nursing homes and assisted living facilities. “This means that family members should be prepared to possibly expand their search to find a facility that
is able to accept their loved ones, depending on their area,” Harmon says. AARP, Medicare and AHCA/NCAL offer detailed checklists of questions to ask prospective nursing homes. PANDEMIC
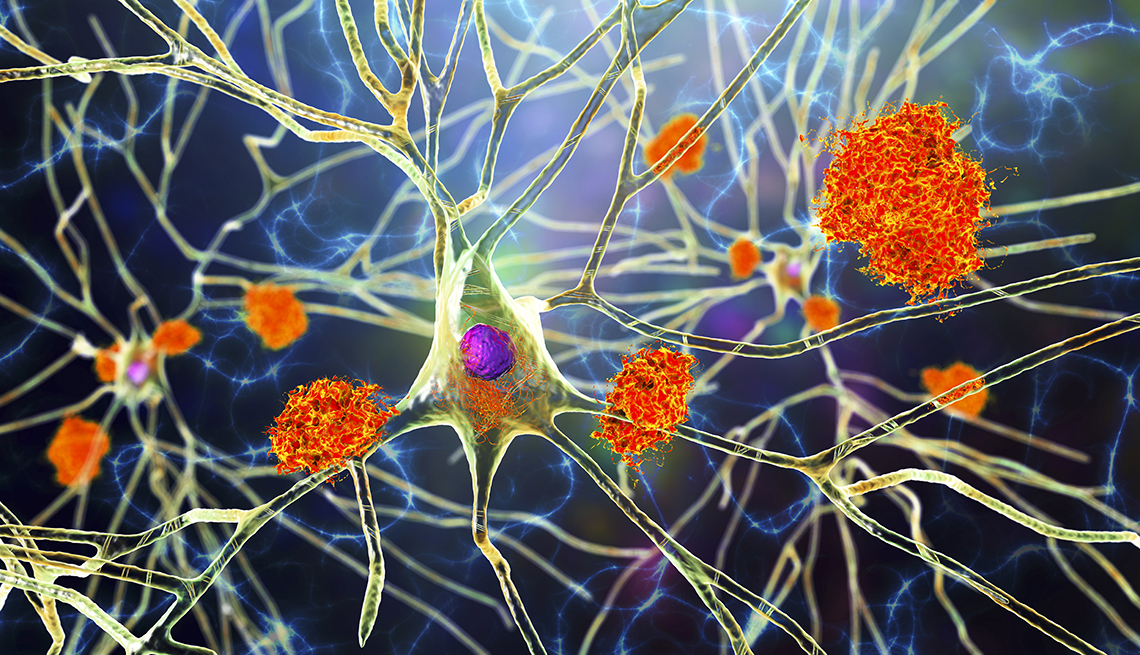
PRIORITIES COVID-19, which has devastated nursing home populations, introduced a new set of concerns and considerations for families seeking placements for loved ones. Here are some things
to ask, and know, about what facilities are doing to reduce the spread of infection and disease. AIR QUALITY: Check if your candidate facilities have invested in portable room cleaners
equipped with high-efficiency particulate air (HEPA) filters. These have become popular as a proven way to reduce the spread of COVID-19 particles. INFECTION CONTROL: Federal regulations
mandate that nursing homes have an infection control and prevention program with written standards for issues such as how to identify infections and prevent spread to other residents or
staff. The facility must have, at minimum, a part-time staffer trained in infection prevention; ask if there is anyone dedicated full-time to the issue. HYGIENE AND MITIGATION: “Core
practices” such as hand hygiene and use of personal protective equipment (PPE) are required, according to the AHCA/NCAL. Nursing homes may customize other infection control procedures based
on local factors, such as COVID-19 spread in the surrounding community. On your visit, look for how employees observe protective and preventive measures such as PPE use, and ask questions
like: * Does the facility have a staff member dedicated full-time to infection control? * Does it regularly test staff and residents? * Are visitors required to take a test, or show proof
of a recent negative test, to enter? * What happens when residents test positive? Are they moved into a dedicated COVID-19 unit or quarantined in their room? * How are residents and
families notified when there’s a case on-site? Are their changes in activities, communal dining or visitor polices when that happens? Infection control isn’t just a COVID concern. Well
before the pandemic, nursing homes struggled with infection problems. Fully 82 percent of facilities surveyed by the Centers for Medicare & Medicaid Services (CMS) between 2013 and 2017
were cited for infection-control deficiencies, the U.S. General Accounting Office reported in 2020. Influenza can spread rapidly within nursing homes, and more than 1 in 11 people older than
65 who contracted a health care–associated infection called _Clostridioides difficile_ died within a month of diagnosis, according to the U.S. Centers for Disease Control and Prevention
(CDC). _C. diff _spreads by tiny spores left on bedside tables and other surfaces, making thorough cleaning essential. UNDERSTAND YOUR PAYMENT OPTIONS Private-pay rates at nursing homes are
typically expensive, and so are the amenities. The 2021 national median for monthly nursing home costs was $7,908 for a shared room and $9,034 for a private room, according to the 2021 Cost
of Care Survey by insurance company Genworth. Prices for care vary widely by state and region. For instance, a private room costs a monthly median of $12,775 in New York state, more than
twice the median rate in Oklahoma. Long-term care insurance may pay some costs for nursing home residency, as does Medicaid, if you qualify. Medicare, however, does not cover long-term
residency in a nursing home. It might pay some costs of short-term stays under specific, limited circumstances. For example, a doctor might send your loved one to a skilled nursing facility
for specialized care and rehabilitation after a hospital stay. If the patient had a stroke or serious injury, recovery could continue there. In such instances, original Medicare can pay a
portion of the cost for up to 100 days in a skilled nursing facility. But there are strict rules: The patient must have received at least three consecutive days of inpatient hospital
treatment. He or she must be admitted to the skilled nursing facility within 30 days of leaving the hospital. The skilled nursing care must be for the same illness or injury, or for a
condition related to it. _Deborah Schoch is an independent journalist who spent 18 years at the _Los Angeles Times_ and helped found the Center for Health Reporting at USC. She is a board
member with the Association of Health Care Journalists._





![[withdrawn] authorised testing facility (atf) service bulletin 01-17: update for diesel opacity meters](https://www.gov.uk/assets/static/govuk-opengraph-image-03837e1cec82f217cf32514635a13c879b8c400ae3b1c207c5744411658c7635.png)